Optimising Anaesthetic Factors to Facilitate Day Case Anterior Cruciate Ligament Repair « Contents
Hull, Frederick (Foundation Year 2), Huckle, Anthony (Foundation Year 2) & Thanawala, Vishal (Consultant Anaesthetist). Nottingham University Hospitals NHS Trust.
Author Contact: f.hull@nhs.net
Keywords
Anterior cruciate ligament repair; local anaesthetic infiltration; analgesia
Abstract
Introduction: The service level report generated by GIRFT (Get It Right First Time) showed that the average length of stay (LoS) for Nottingham University Hospitals (NUH) Trust following Anterior Cruciate Ligament Repair (ACLR) from April 2017 to March 2018 was 1.35-days. Reducing our LoS to match the national average of 0.13-days could save an estimated £45,000. We performed a review of anaesthesia and specifically postoperative nausea and vomiting (PONV) and pain as factors which may be contributing to our increased LoS to enable us to formulate perioperative guidelines.
Methods: 113 patients underwent ACLR in NUH between March 2018 and March 2019. Pain and PONV scores were analysed from recovery and at six-hourly intervals postoperatively using electronic observation data along with analgesic and antiemetic regimes used intra and postoperatively.
Results: Forty-seven patients (42%) experienced moderate-severe pain in the recovery room and 12 and 11 patients (11%, 10%) at 6 and 12-hours, respectively [Fig. 1-3]. Four patients (3.5%) received intraoperative local anaesthetic infiltration, and 13 patients (12%) received a femoral or adductor canal nerve block.
Conclusion: Use of intraoperative local anaesthetic infiltration/nerve block has been shown to improve pain control for up to 24-hours in ACLR [4]. We recommend use of local anaesthetic infiltration or regional anaesthetic nerve block for all patients as well as use of multi-modal postoperative analgesia consisting of paracetamol, NSAID’s and an opioid as part of the discharge medication for the first 48-hours to provide optimal analgesia and facilitate day case surgery. We are in the process of formulating day surgery pathways and guidelines to reduce inpatient stay, improve patient experience and save revenue for the Trust.
Introduction
The GIRFT (Get It Right First Time) report for 2017-18 showed that the average length of stay (LoS) for patients undergoing anterior cruciate ligament repair (ACLR) at Nottingham University Hospitals NHS Trust was 1.35 days. Reduction in the LoS to match the national average of 0.13 days can help save an estimated £45,000 annually, according to local trust data. Postoperative nausea and vomiting (PONV) and pain were evaluated as potential anaesthetic factors contributing to delayed discharge.
Aims
- Determine the number of patients operated as day cases.
- Determine the incidence of PONV and severity of pain.
- Evaluate the perioperative analgesia and antiemetic regimes.
- To recommend changes in practice to help facilitate day surgery for this group of patients.
Methods
Following ethical approval from the hospital clinical audit and quality improvement team, retrospective data collection was performed for all patients who underwent ACL repair from April 2018-March 2019. Digital Health Record (DHR) and Medway hospital data systems were used to gather data pertaining to perioperative analgesia and antiemetic drug usage from the anaesthesia booklet and the drug chart. PONV was classified as either absent or present and pain scores were rated as absent, mild, moderate, or severe.
Results
- 113 patients underwent ACLR in NUH between March 2018 and March 2019 and all of them (100%) were carried out as inpatients. 101 patients (89%) were discharged the next day, 11 patients stayed for two nights (9.7%), and one patient stayed for three nights (0.88%).
PONV:
- Two patients (1.8%) reported PONV in the recovery room, 10 patients (9%) at six-hours and two patients (1.8%) at 12 and 18-hours postoperatively. None of the patients reported PONV at 24-hours.
- Intraoperative antiemetic usage was as follows:
- 95 patients (84%) received ondansetron
- 61 patients (54%) received dexamethasone and
- 49 patients (43%) received cyclizine.
- Postoperatively, ondansetron, cyclizine, prochlorperazine and metoclopramide were used.
Pain:
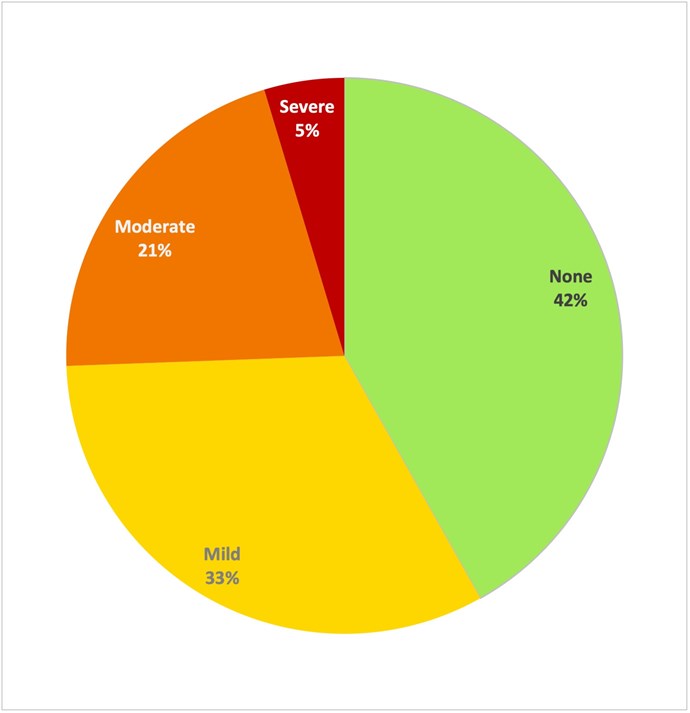
- Forty-seven patients (42%) experienced moderate-severe pain in the recovery room, 12 patients (11%) at six-hours, 11 patients (10%) at 12-hours, three patients (2.9%) at 18-hours and 11 patients (26%) at 24-hours postoperatively.
- Intraoperative analgesia usage was as follows:
- 95 patients (84%) received paracetamol
- 98 patients (87%) received morphine or oxycodone
- 83 (73%) received an NSAID. NSAID’s used intraoperatively included either naproxen or parecoxib or diclofenac.
- Multimodal pharmacological analgesia (MMPA) was deemed to be a combination of paracetamol, NSAID and a long acting opioid.
- Of the 65 patients who were in none or mild pain in recovery, 45 (69%) received MMPA.
- Of the 47 patients who reported moderate-severe pain in recovery, 29 (62%) received MMPA.
- 13 (12%) patients received a nerve block with nine (69%) of these being femoral nerve blocks and the remaining four (31%) adductor canal nerve blocks.
- Six patients (46%) who received a nerve block were in moderate-severe pain in the recovery room and one patient (20%) was in moderate-severe pain after 24-hours.
- Four patients (3.5%) were documented to have received local anaesthetic infiltration; in recovery two of these (50%) reported moderate pain, one (25%) mild pain and one (25%) had no pain.
Figure 1. Percentage of patients reporting PONV (blue) and moderate-severe pain (red) at 6-hr
intervals following ACLR.
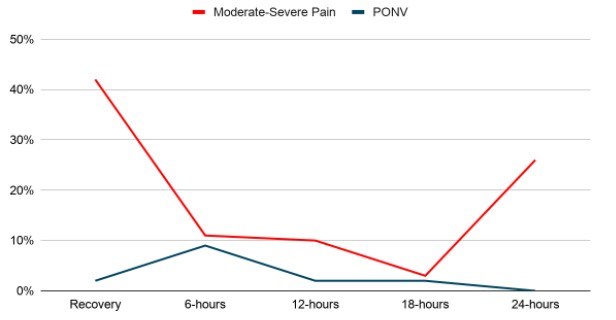
Figure 2. Pain scores (categorised by intensity) in recovery room post-ACLR. (n=112).
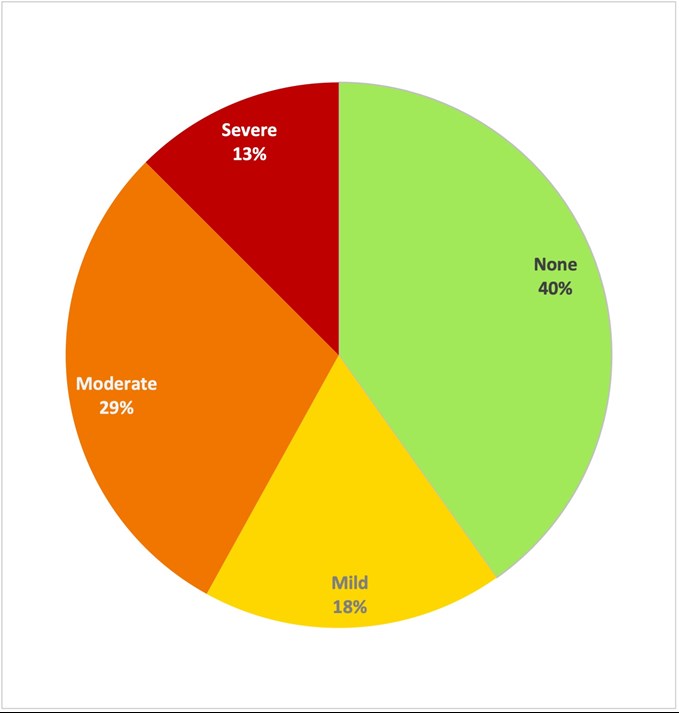
Figure 3. Pain scores (categorised by intensity) at 24hrs post-ACLR. (n=44).
Discussion
Our project aim was to identify potential anaesthetic factors which may contribute to delayed discharge for patients undergoing ACLR. The incidence of PONV was low peri-operatively, however we would like to suggest that all patients should receive at least two anti-emetics intraoperatively as per the departmental guidelines to reduce the potential incidence even further and enable timely discharge.
Postoperative pain was identified as a potential factor since 42% of patients reported moderate-severe pain in the recovery room and 26% of patients remaining in hospital experienced it at 24-hours postoperatively. Review of local nerve block usage showed that 12% of patients received a nerve block and 3.5% received local anaesthetic infiltration, albeit discussion with surgical colleagues suggests local anaesthetic infiltration was used for the vast majority of patients but it may not have been documented.
Several systematic reviews have been conducted into the efficacy of different regional analgesic techniques in ACLR operations (1, 2, 3). A recent literature review has recommended the use of multimodal analgesia in combination with local anaesthetic infiltration or addition of adductor canal nerve block in those patients at risk of severe pain (opioid tolerance, chronic pain) (4).
Limitations of this audit include that pain and PONV scores were recorded at a single point in time and may not fully represent the patients’ symptoms. The postoperative analgesia plan must be tailored for each patient individually taking into consideration their background comorbidities and opioid usage.
Overall, we suggest the use of local anaesthetic infiltration or adductor canal nerve block for all patients as part of multi-modal postoperative analgesia regime, in line with recommendations from the ACLR National Day Surgery Delivery pack (Appendix A) to ensure patients are comfortable in the postoperative period. The discharge analgesia prescription should include paracetamol, NSAID and a strong opioid for the first 48-hours to provide optimal analgesia.
We envisage that this audit will act to mitigate and minimize potential anaesthetic factors which contribute to delayed discharge and at the same time appreciate and understand the need of a multidisciplinary approach to address other non-anaesthetic causes. We have discussed the postoperative use of antibiotics and physiotherapy and are in communication with various stake holders of the multidisciplinary team to achieve the shared goal of day case surgery for all patients undergoing ACL repair.
References
- Vorobeichik L, Brull R, Joshi GP, Abdallah FW. Evidence Basis for Regional Anesthesia in Ambulatory Anterior Cruciate Ligament Reconstruction: Part I-Femoral Nerve Block. Anesth Analg. 2019 Jan;128(1):58-65. doi: 10.1213/ANE.0000000000002854. PMID: 29596099.
- Sehmbi H, Brull R, Shah UJ, El-Boghdadly K, Nguyen D, Joshi GP, Abdallah FW. Evidence Basis for Regional Anesthesia in Ambulatory Arthroscopic Knee Surgery and Anterior Cruciate Ligament Reconstruction: Part II: Adductor Canal Nerve Block-A Systematic Review and Meta-analysis. Anesth Analg. 2019 Feb;128(2):223-238. doi: 10.1213/ANE.0000000000002570. PMID: 29064877.
- Yung EM, Brull R, Albrecht E, Joshi GP, Abdallah FW. Evidence Basis for Regional Anesthesia in Ambulatory Anterior Cruciate Ligament Reconstruction: Part III: Local Instillation Analgesia-A Systematic Review and Meta-analysis. Anesth Analg. 2019 Mar;128(3):426-437. doi: 10.1213/ANE.0000000000002599. PMID: 29200071.
- Ramlogan R, Tierney S, McCartney CJL. Anterior cruciate ligament repair and peripheral nerve blocks: time to change our practice? Br J Anaesth. 2019 Aug;123(2):e186-e188. doi: 10.1016/j.bja.2019.05.028. Epub 2019 Jun 12. PMID: 31202563; PMCID: PMC6676314.
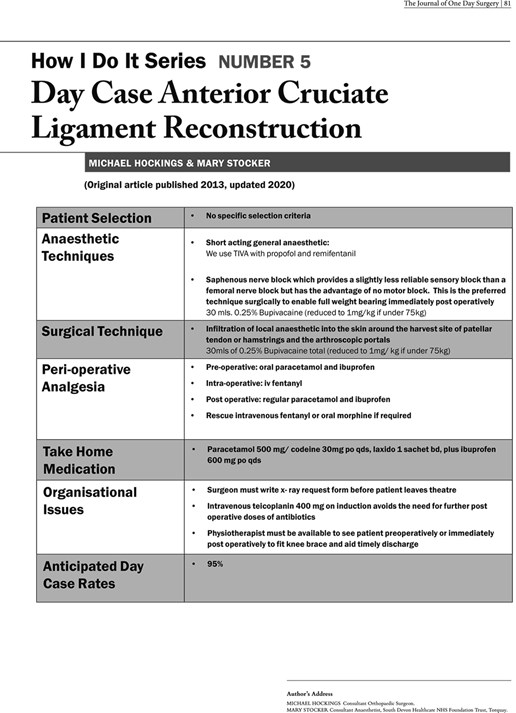
- Hockings M, Stocker M. How I Do It Series: Number 5: Day Case Anterior Cruciate Ligament Reconstruction. J One Day Surg. 2020.
Appendix A
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2021-journal/jods-312-may-2021/optimising-anaesthetic-factors-to-facilitate-day-case-anterior-cruciate-ligament-repair/
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/51040/312-optimising-anaesthetic-factors-to-facilitate-day-case-anterior-cruciate-ligament-repair.pdf