Is it time to default hysterectomies to day surgery? A review of outcomes in a district general hospital day surgery unit « Contents
Anna Fergusson Specialty Trainee in Anaesthetics1
Andrew Weir Specialty Trainee in Anaesthetics1
Rowan Mankiewitz Trust Doctor1
Subramanian Narayanan Consultant Gynaecologist2
Jonathon Hindley Consultant Gynaecologist2
Eleanor Rayner Specialist Registrar in Obstetrics and Gynaecology2
Mary Stocker Consultant Anaesthetist1
Authors' Addresses
1Department of Anaesthetics, Torbay Hospital
2 Department of Obstetrics and Gynaecology, Torbay Hospital
Keywords: Day Surgery, Hysterectomy, Gynaecology
Abstract
Introduction: Hysterectomies are common procedures which traditionally have been performed via an inpatient pathway. However, there is evidence that day case surgery is safe, has a high level of patient satisfaction, and provides a cost-effective, bed-saving service. This audit reviews patient outcomes and satisfaction following day case hysterectomy.
Method: The data for a 5-year period for all patients undergoing laparoscopic and vaginal hysterectomy were reviewed. Patient outcomes including unplanned admissions, reasons for admission, complications at day 1 for discharged patients and patient satisfaction were collected.
Results: During the 5-year period 678 laparoscopic and vaginal hysterectomies were performed of which 60.8% were via a day case pathway; of these 57.5% were laparoscopic and 42.5% vaginal. Of the day case group, 77 required admission (18.7%). Since the introduction of the day case hysterectomy service, the planned day case rate has increased from 37.4% to 81.3% for laparoscopic hysterectomies, and from 74.6% to 80% for vaginal hysterectomies. During this time unplanned admissions rates have reduced, demonstrating an improvement with confidence and experience.
The commonest reason for admission was pain (38.3% of unplanned admissions) followed by surgical complications. Pain was also the commonest complication reported at day 1 amongst those who were discharged; 21% reported moderate pain and 3% reported severe pain. Of those who were discharged, 100% were satisfied or very satisfied with their experience.
Conclusions: This audit demonstrates that both laparoscopic and vaginal day case hysterectomies can be safely performed with an acceptable admission rate, minimal post-op morbidity and good patient satisfaction.
Introduction
Hysterectomies are the most common major gynaecological operation performed worldwide, with almost 35,000 performed in the UK in 2018/20191. Until recently, the vast majority of these have been performed via an inpatient pathway; HES data from 2018/2019 shows that 1.5% of hysterectomies performed in England were day cases1. There is however evidence that day case surgery is safe and has a high level of patient satisfaction for a variety of gynaecological procedures, including laparoscopic2 and vaginal hysterectomy3. Day case surgery is associated with reduced inpatient bed usage and health economic benefits.
The Torbay Hospital Day Surgery Unit is a progressive unit and has experience in performing major procedures as day cases. For the majority of this study period it was open until 8pm, at which point all patients are either discharged or admitted to the main hospital. Recently the unit’s opening hours have been extended to 9pm and we anticipate that this will further increase our successful discharge of complex surgical procedures such as hysterectomies. From 2015, hysterectomies have been preferentially planned and listed as day cases, unless there are convincing surgical, anaesthetic or social contraindications. This review aims to assess the outcomes over this period.
Methods
The data for all patients having a hysterectomy at Torbay Hospital over a 4-year and 8-month period from April 2015 to November 2019 was retrospectively reviewed. For those planned as day cases, data was collected from our Day Surgery Unit computer database, Galaxy Surgery (ÓCSC). This database records multiple aspects of the patient’s pathway, including date of surgery, age, American Society of Anaesthesiologists (ASA) physical status classification grade, timings, surgical procedure(s), anaesthetic technique and discharge or unexpected admission. As is routine at Torbay Day Surgery Unit, those discharged were telephoned the following day by a dedicated team of nursing staff to offer support and advice, trouble shoot any post-operative complications and collect post-discharge follow up data. This data includes information on pain level, nausea and vomiting, dizziness, drowsiness, bleeding and any other complications using multiple choice questions. Patient satisfaction is also collected using a three-point Likert scale (very satisfied, satisfied, not satisfied) and there is an opportunity for the patient to feedback any further information or comments. Where post discharge follow-up data were missing, we examined the patient’s electronic record to identify any admissions or attendances at the Emergency Department (ED) or Surgical Assessment Unit.
For those patients who had an unexpected admission, patient records and discharge summaries were examined to determine the cause of admission. For those on an inpatient pathway, patient demographics and type of surgery were collected for comparison.
Specific anaesthetic technique was not protocolised and was left to the discretion of the anaesthetist. However, anaesthetic techniques within our day surgery unit are all tailored to deliver short-acting anaesthesia, with minimal side effects and multi-modal analgesia. The majority of patients received standard analgesic premedication of paracetamol 1g PO and ibuprofen 1600mg SR PO (if no contraindications were present) and single or dual antiemetic therapy (dexamethasone and/or ondansetron). There are strict protocols in use within our day surgery unit such that long-acting opioids are not available, nitrous oxide is not used and the large majority of patients are anaesthetised using total intravenous anaesthesia. Analgesia is provided both intra-operatively and in the primary recovery unit by use of intravenous fentanyl supplemented with oral morphine as required. Surgery was performed by a number of consultant or senior registrar surgeons, each with their own slightly different surgical and local anaesthetic technique.
Data were analysed using simple descriptive statistics. Where appropriate the Chi-squared test and paired t-test was used to indicate significance.
Results
Table 1.
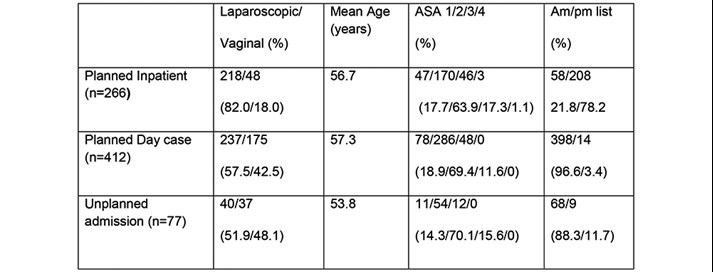
Figure 1a. Laparoscopic Hysterectomies: Change in Inpatient vs Day case numbers over time.
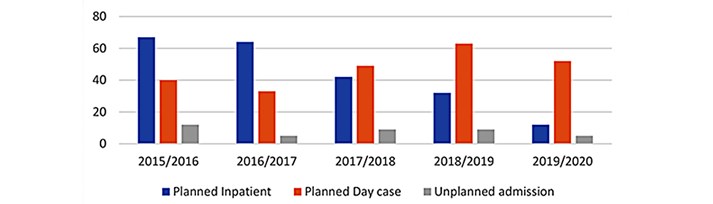
Figure 1b. Vaginal Hysterectomy: Change in Inpatient vs Day case numbers
over time.
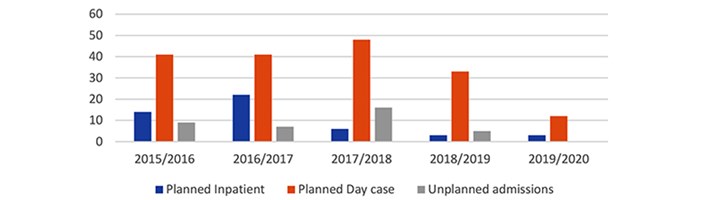
During the 5-year period a total of 678 laparoscopic and vaginal hysterectomies were performed, of which 412 (60.8%) were via a day case pathway (see Table 1). The proportion of patients who were on a day case pathway increased throughout the 5-year period (see figure 1a and 1b). In 2019/2020, 52/64 (81.3%) of laparoscopic hysterectomy patients and 12/15 (80%) of vaginal hysterectomy patients were planned as day case, compared with 40/107 (37.3%) of laparoscopic and 41/55 (74.5%) of vaginal hysterectomy patients in 2015/2016.
Age was not a factor in determining whether a patient was scheduled for a day case or inpatient pathway. The mean age of patients planned as a day case was 56.7 years vs 57.9 years for the inpatient pathway (p= 0.289). Patients who were ASA 1 or 2 were more likely to be scheduled for a day case pathway compared to an inpatient pathway (p=0.038). There were similar numbers of ASA 3 patients in the day case and inpatient groups (48 vs 46), and all ASA 4 patients were scheduled for an inpatient pathway. These results reflect the policy of our day unit in that patients are not excluded from day surgery due to either age or ASA status.
In the day case group, 237/412 (57.5%) were planned to be performed laparoscopically and 175/412 (42.5%) were planned to be performed vaginally. By comparison, in the inpatient group, 218/266 (82%) were planned to be performed laparoscopically, and 48/266 (18%) vaginally. One hundred and seventy five out of 223 (78.5%) of all vaginal hysterectomies, and 237/456 (52%) of all laparoscopic hysterectomies were planned as day case procedures. One of the factors for a higher number of planned inpatient laparoscopic hysterectomies is that one of our two laparoscopic surgeons has his main operating list scheduled in inpatient theatres in the afternoon. These patients are much less likely to achieve same day discharge so are usually scheduled via an inpatient pathway. It is hoped that in the future more morning operating provision will be available in the day surgery unit to enable these patients to be converted to a day case pathway.
Of the day case group, 77/412 (18.7%) required admission. However, these rates have significantly decreased over time from 25.9% in 2015/2016 to 7.1% in 2019/2020 (p=0.0048). Admission rates were similar in those performed vaginally (37/175, 21.1%) and those performed laparoscopically (40/237, 16.9%, p=0.27). There was a trend but no significant difference between age and unplanned admission rate, with the mean age of 53.8 years in those admitted, compared with 57.3 years in those discharged (p=0.0549). Patient’s ASA grade did not have a significant impact on likelihood of admission. Sixty five out of 364 (17.9%) of ASA 1 and 2 patients required admission compared to 12/48 (25%) of ASA 3 patients (p=0.233). The vast majority of patients were operated on during morning lists; however, of the 14 patients who were operated on during the afternoon, 9 (64.3%) were admitted (p<0.0001).
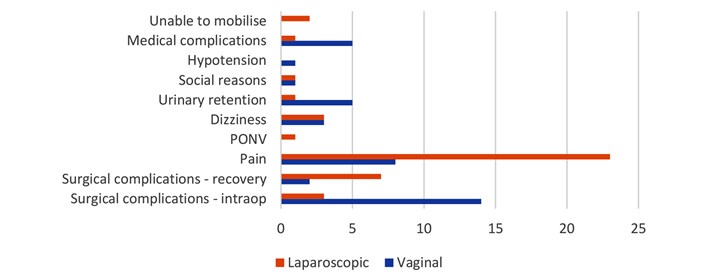
The most common reason for admission was pain (31/77, 40.3% of unplanned admissions). Of these, rates were significantly higher in those having laparoscopic compared to vaginal surgery (23/40, 57.5% vs 8/37, 21.6%, p=0.00134). The second most common reason for unplanned admission was surgical complications (26/77, 33.8% of unplanned admissions). These were split into those which were detected intra-operatively, such as bleeding or conversion to open surgery, and those which were detected in recovery, such as post-operative bleeding. Admission due to intra-operative surgical complications was statistically more common in those having a vaginal hysterectomy, compared to those having a laparoscopic hysterectomy (14/37, 37.8% vs. 3/40, 7.5%, p=0.00134). Other reasons for admission included social reasons, dizziness, urinary retention, inability to mobilise, medical complications, hypotension and post-operative nausea and vomiting (PONV), (see Figure 2).
Figure 2. Reason for admission in those planned as Day cases but required admission.
Post-operative take home analgesia is protocol driven and prescribed for all patients; co-codamol (30/500) 2 tablets 4 times a day plus ibuprofen 400mg 4 times a day if there are no contraindications. Patients are also prescribed Macrogol to avoid post-operative constipation associated with codeine. Day 1 complication rates were generally low, with the majority of patients reporting no or mild pain, nausea, dizziness and drowsiness, none or a little bleeding and none or one episode of vomiting (see Figure 3). Pain was the commonest day 1 complication, with 128/271 (47.2%) having mild pain, 57/271 (21.0%) having moderate pain and 8/271 (3.0%) patients reporting severe pain. Seventy eight out of two hundred and seventy one patients (28.9%) reported having no pain. These results are well within acceptable levels for pain following day case surgery as recommended by the Royal College of Anaesthetists.
Figure 3 Complications at Day 1 amongst those discharged home.
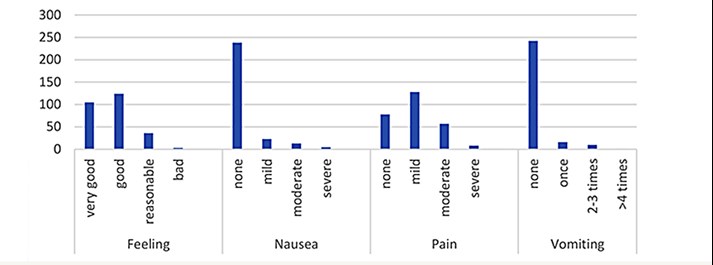
Of those who were discharged and where follow up was available, 100% of patients were satisfied or very satisfied with their experience.
There was no follow up data for 64 (19.1%) of the patients, either because they were not able to be contacted on day 1, or there was a shortage of DSU nursing staff to complete the telephone follow ups. The electronic records were reviewed for these patients to identify any who presented to the ED, surgical assessment unit or were admitted. The majority (56/64, 87.5%) had no further encounters with the hospital in the 7 days following their procedure. Of the 8 patients who re-attended either ED or SAU, 6 were admitted. The cause of the reattendance was bleeding in 4 patients, haematoma development in 2 patients, nausea and vomiting in 1 patient, and urinary retention in 1 patient. No patients reattended due to poorly controlled pain.
Discussion
This review has demonstrated that both laparoscopic and vaginal hysterectomies can be safely performed as day case procedures with minimal post-op morbidity and excellent patient satisfaction. The admission rate was initially relatively high with around 1 in 5 patients requiring admission. This figure is comparable with previous studies. A 2017 systematic review found that of 435 laparoscopic hysterectomy patients from studies that prospectively planned for same day discharge, 78.4% patients were discharged before midnight on the day of their surgery4.
Throughout the past 5 years, increasing numbers are being performed as day case surgery while admission rates appear to be falling. Over the period of the study with increasing confidence and developing expertise of the multidisciplinary day surgery team, these rates have dropped considerably to under 8%. Previous studies of vaginal and laparoscopic hysterectomy have demonstrated a wide range of admission rates, from 4 to 79%5. Unlike the majority of other studies where careful patient selection occurred, listing patients for day case surgery has been the default option for all patients at Torbay since 2015. This occurs regardless of comorbidities and ASA grade, unless an inpatient pathway is specifically selected by the surgeons at booking. This review demonstrated that there was no increase in admission rates amongst those who were ASA 3 compared to ASA 1 or 2. This finding is consistent with advice from the 2019 guidelines from the Association of Anaesthetists and the British Association of Day Surgery6, which recommends that ASA grade is not used as a determinant of suitability for day case surgery.
Hysterectomies performed on afternoon lists had a significantly higher rate of admission. Wherever possible, hysterectomies should be performed early in the morning to allow maximum time for discharge, or provisions made to allow later discharges.
Pain was the commonest reason for admission in those planned as day case; this was recorded significantly more frequently amongst those having a laparoscopic hysterectomy compared with a vaginal hysterectomy. Pain protocols utilising a multi-modal approach should be developed and standardised to aim for adequate intra-operative analgesia, and rapid and effective post-operative analgesia.
The second commonest cause for admission was surgical complications. The majority of these were detected in the intra-operative period, allowing the process of admitting the patient to start immediately post operatively. Vaginal hysterectomies were more likely to result in intra-operative surgical complications compared with laparoscopic hysterectomies.
We found that performing hysterectomies as day case surgery is generally well tolerated and associated with a low complication rate. Patient satisfaction amongst those discharged is universally very high.
This audit has a number of limitations. We have only reviewed information which was available within the DSU dataset; this excluded a number of factors likely to influence our results, such as surgical factors (including grade of surgeon and the use of local anaesthetic), and patient factors such as body mass index (BMI), and the presence of acute and chronic pain risk factors. There is likely to be a degree of bias in the data collection of post discharge complications and satisfaction levels; data collected non-anonymously by the care provider is notoriously unreliable. There was a failure to follow up a significant number of discharged patients – it is unclear if these patients will have been representative of patients as a whole or did not engage in the follow up process because of their experience. Patients on the boundaries of health care systems could have presented elsewhere with complications and would therefore not appear on our database, leading to an under-estimation of readmissions.
We believe that these results are representative of the wider population and as such can be extrapolated to similar hospitals and patient groups. Further work could explore specific analgesic protocols for use in laparoscopic hysterectomies, protocols for listing criteria using shared decision making, and formal health economic analysis.
References
- NHS digital. Hospital Admitted Patient Care Activity - NHS Digital [Internet]. [cited 2020 May 31]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity
- Schiavone MB, Herzog TJ, Ananth C V., Wilde ET, Lewin SN, Burke WM, et al. Feasibility and economic impact of same-day discharge for women who undergo laparoscopic hysterectomy. Am J Obstet Gynecol. 2012 Nov 1;207(5): 382.e1-382.e9.
- Rajappa GC, Vig S, Bevanaguddaiah Y, Anadaswamy TC. Efficacy of pregabalin as premedication for post-operative analgesia in vaginal hysterectomy. Anesthesiol Pain Med. 2016 Jun 1;6(3).
- Korsholm M, Mogensen O, Jeppesen MM, Lysdal VK, Traen K, Jensen PT. Systematic review of same-day discharge after minimally invasive hysterectomy. Vol. 136, International Journal of Gynecology and Obstetrics. Wiley Blackwell; 2017. p. 128–37.
- Dedden SJ, Geomini PMAJ, Huirne JAF, Bongers MY. Vaginal and Laparoscopic hysterectomy as an outpatient procedure: A systematic review. Eur J Obstet Gynecol Reprod Biol. 2017 Sep 1; 216:212–23.
- Bailey CR, Ahuja M, Bartholomew K, Bew S, Forbes L, Lipp A, et al. Guidelines for day‐case surgery 2019. Anaesthesia [Internet]. 2019 Jun 8 [cited 2020 May 31];74(6):778–92. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/anae.14639
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/43854/304-fergusson.pdf