Day-case Parathyroidectomy as standard: a single centre experience of safe surgical practice « Contents
Jessica Chang General Surgical Specialty Registrar
Christodoulos Neophytou General Surgical Specialty Registrar
Sian Davies General Surgical Specialty Registrar
Emma Howard Foundation Doctor
Andrew Houghton Consultant Vascular and Endocrine Surgeon
Authors, address
Shrewsbury and Telford NHS Trust, Mytton Oak Road, Shrewsbury SY3 8XQ
Corresponding author Jessica.chang@nhs.net
Keywords Same-day discharge; parathyroidectomy; day-case.
Abstract
Introduction: Despite a shift towards same-day discharge in many surgical departments, true day-case rates remain low following parathyroidectomy (10% nationally in UK). Our standard practice is same day discharge for all patients having surgery for primary hyperparathyroidism. Patients are discharged on oral calcium/vitamin D with outpatient calcium checks day 6 - 7 and follow up day 10. Our retrospective study assesses the safety of this practice.
Methods: All patients undergoing parathyroidectomy for primary hyperparathyroidism (bilateral or unilateral neck exploration) were identified between 01/01/2010 and 30/12/2019. Patients with renal hyperparathyroidism were excluded. Demographics, histology, biochemical results, and length of stay were extracted from patient records.
Results: 257 parathyroid procedures for primary hyperparathyroidism were performed during the study period. The cohort included 199 females, median age of 63 (range 15 – 88). Day-case procedures were carried out in 93.0%, with 17 requiring overnight admission for anaesthetic/social reasons (length of stay 0 – 4 days). Three patients presented postoperatively with symptoms of relative hypocalcaemia despite being biochemically normo-calcaemic, a single patient requiring intravenous calcium for symptomatic hypocalcaemia (adjusted calcium 1.8mmol/l).
Conclusion: Day-case parathyroidectomy should become standard practice in the majority of patients undergoing surgery for primary hyperparathyroidism. It is both popular with patients and is also safe. Matching our day-case rates nationally could save more than 1,900 hospital bed days per year. Symptomatic hypocalcaemia is minimised by oral calcium/vitamin-D supplements and routine calcium checks are not required prior to discharge.
Introduction
In recent years there has been a drive across the United Kingdom to provide same-day discharge for surgical patients. More and more surgical procedures are being considered suitable for this approach. There have been a number of retrospective studies suggesting that same-day discharge for parathyroidectomy is safe (1-7). Despite mounting evidence however, the most recent British Association of Endocrine and Thyroid Surgeons (BAETs) audit (8) in 2017 found that only 10% (an increase from 5% reported in 2012) of all parathyroidectomies are carried out as true day-case operations. The majority of these are “targeted” surgical procedures with a 25% (increasing from 11.6% 2012) day-case rate in these cases. In bilateral neck exploration a day-case rate of just 2.5% is reported.
One suggestion for the rationale of continuing with routine overnight observation is concern about bleeding requiring re-operation (incidence reported of around 0.4%) (8-10). There is also concern about unrecognised hypocalcaemia and significant complications occurring from this following discharge. The incidence is reported from 10 – 46% (11-15), with a significantly higher incidence reported in renal hyperparathyroidism.
The purpose of this paper is to describe a snapshot of our single-surgeon practice and discuss how we may further develop day-case parathyroidectomy in the UK.
Methods
A retrospective, observational cohort study was carried out at the Royal Shrewsbury Hospital. In our single-centre unit all cases are carried out by a single surgeon, who has developed his practice over 20 years. All patients who underwent parathyroidectomy for primary disease, between 01/01/2010 and 30/12/2019 were included. All patients were referred from regional endocrine specialists with both symptomatic and asymptomatic disease. Patients included those who had had previous negative or failed parathyroidectomy. Patient data was recorded by the operative surgeon during the study period using a prospectively collected database. This list was cross-checked with histopathology records for parathyroid samples received during the time period. Patient demographics, pre-operative and post-operative calcium, serum parathyroid hormone (PTH) levels, pre-operative imaging, localisation and histopathology were recorded retrospectively. All 30-day morbidities were documented, and length of stay confirmed. Primary outcome was length of stay. Secondary outcomes include post-operative bleeding, hypocalcaemia, and persistent hypercalcaemia (more than 6 months post-operatively).
Exclusions
Patients with renal failure, referred with secondary or tertiary hyperparathyroidism undergoing total parathyroidectomy.
Surgical Process
Pre-operatively patients undergo single or multiple imaging modalities; usually including ultrasound and a SPECT CT (single proton emission computerised tomography) scan.
Every patient underwent a standard transverse incision, of around 6cm. All patients with positive pre-operative localisation of an affected gland underwent unilateral exploration (with bilateral exploration only performed if the adenoma was not found or did not appear large enough). For those patients without preoperative localisation, bilateral exploration was carried out. A single adenoma was removed if located with ease, in the few cases where no overt adenoma was identified, biopsies of all four parathyroid glands was carried out. Removal of 3 ½ glands was performed if diffuse hyperplasia appeared to be the diagnosis. Re-explorations were almost always scan directed and sometimes included hemithyroidectomy if an intra-thyroid adenoma was suspected.
Intraoperatively, excised samples were sent for fresh frozen section; with results telephoned to the operative consultant within 30 minutes. We do not have access to intra-operative PTH testing, nor do we routinely use any other intra-operative technique to aid visual identification of parathyroid glands.
Patients are discharged same day, being prescribed calcium/vitamin-D supplementation as standard. Patients are then seen day 10 post-operatively in outpatients, with serum levels checked approximately day 6 or 7. Oral calcium supplementation is stopped once normocalcaemic on serum testing (usually at first follow up).
Definitions
Hypocalcaemia defined as serum adjusted calcium <2.10mmol-1 as per BAETs.
Statistics
Statistical analysis was performed using GraphPad Prism (software version). Fischer’s exact test was used and p = <0.05 was statistically significant.
Results
The study period included operations performed between 01/01/2010 and 30/12/2019. During this study period a total of 300 parathyroid procedures were performed: 257 for primary hyperparathyroidism. The remaining 43 patients were renal patients undergoing total parathyroidectomy.
Patients included 201 females, 56 males. Patients had a median age of 63 (range 15-90). The age distribution was not significantly different comparing males and females.
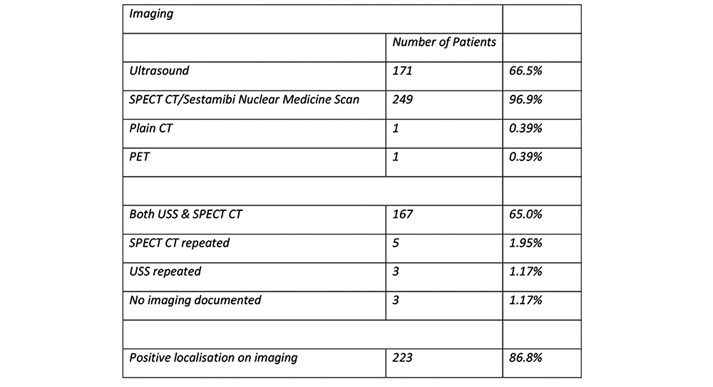
Pre-operative imaging
Of the 257 patients, three patients have no record of pre-operative imaging. The remaining 254 patients underwent radionuclide imaging (SPECT CT or Sestamibi scan), with ultrasound as well in most cases (figure 1). 5 patients could not tolerate radionuclide imaging and only had ultrasound assessment. In 223 cases positive localisation of the affected parathyroid gland was obtained pre-operatively via imaging.
Figure 1: Pre-operative imaging performed for localisation.
Histopathology
Histopathology confirmed 244 (94.9%) adenomas and 2 adenocarcinomas. 11 samples were reported as hyperplasia of the parathyroid gland. 1 sample in a patient undergoing re-exploration was suggested to be a parathyroid adenoma on frozen section, but paraffin sections showed thyroid tissue. This patient required a third exploration at a later date, when a further scan showed a retrosternal adenoma.
Day-case rates
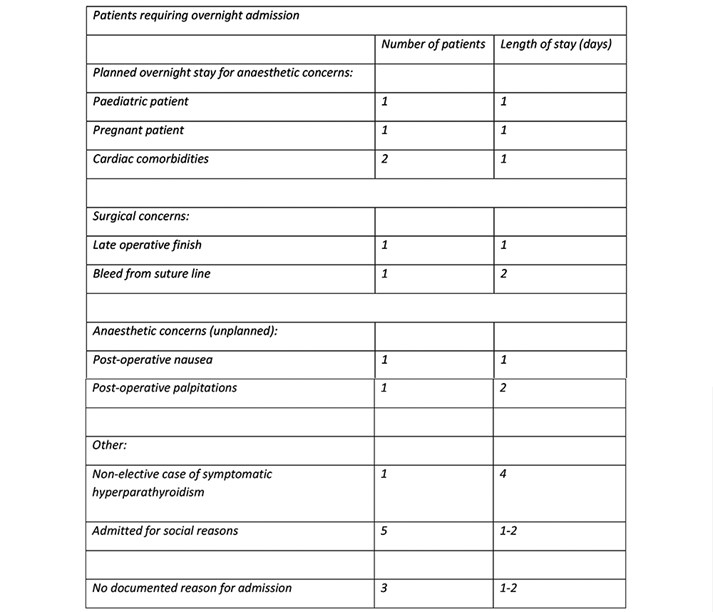
Day-case procedures were performed in 240 patients (93%). 12 patients (4.7%) were discharged next day and 4 patients (1.56%) within 48 hours of surgery. A single patient was discharged 4 days post-operatively, this patient underwent non-elective surgery following admission with symptomatic hypercalcaemia.
Reasons for admission were in the most part due to comorbidities or social needs (figure 2). Only two patients were admitted with post-operative concerns.
Figure 2: Reasons for admission following parathyroidectomy.
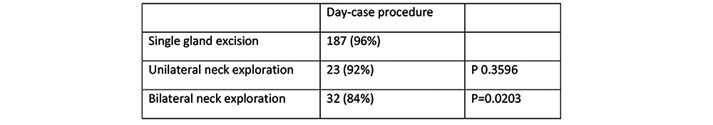
All patients underwent transverse neck incision. They then underwent either excision of single gland (194 patients, 73%), unilateral neck exploration (25 patients, 9.7%) or bilateral neck exploration (38 patients, 14.7%).
Day-case rates have been calculated for three subsets of patients (undergoing single gland excision, unilateral neck exploration or bilateral neck exploration – figure 3). There is no significant difference in day-case rate between single gland excision and unilateral neck exploration (96% vs 94%, p = 0.3596). When comparing bilateral neck exploration however a significant decrease is seen (96% vs 84%, p = 0.0203). Individual analysis of reasons for admission in the bilateral neck exploration cohort shows two patients admitted for post-operative anaesthetic reasons, one for medical admission (emergency procedure) and one for a late finish.
Figure 3: Day-case rates compared across subsets (single gland excision,
unilateral neck exploration or bilateral neck exploration).
Post-operative Morbidity
A single patient developed palpitations post-operatively. They were not found to have clinical hypocalcaemia (post op calcium 2.30mmol/l). No clinical diagnosis was reached. A second patient had significant bleeding from their suture line which required over-sewing in recovery. No further intervention was required, and they had an otherwise uneventful post-operative period. A further patient presented to our surgical assessment unit 18 days later with a seroma, which was aspirated and required no further intervention.
Three patients re-attended with symptoms suggestive of hypocalcaemia, with serum calcium levels of 2.30mmol/l, 2.30mmol/l and 3.10mmol/l, respectively. All of these patients had preoperative calcium levels in excess of 3.0 and were diagnosed as having relative hypocalcaemia. These patients were continued on oral calcium and vitamin D supplementation until resolution of symptoms and all 3 were normocalcaemic at follow up.
One patient presented as an emergency with symptoms of hypocalcaemia (adjusted calcium at 24 hours post-operatively 1.8mmol/l). This patient received intravenous calcium and vitamin D and was discharged after 24 hours observation. This patient continued oral calcium and vitamin D supplementation at follow up. Of note, this patient had undergone 3 explorations for hypercalcaemia in 2013, 2016 and 2017 respectively. At the third exploration in 2017 a retro-manubrial adenoma was identified, the patient previously having a histologically proven right upper adenoma removed.
30-day morbidity has been analysed and detailed as per Clavien-Dindo (Figure 4).
Figure 4: 30-day post-operative morbidity described as per Clavien-Dindo classification.
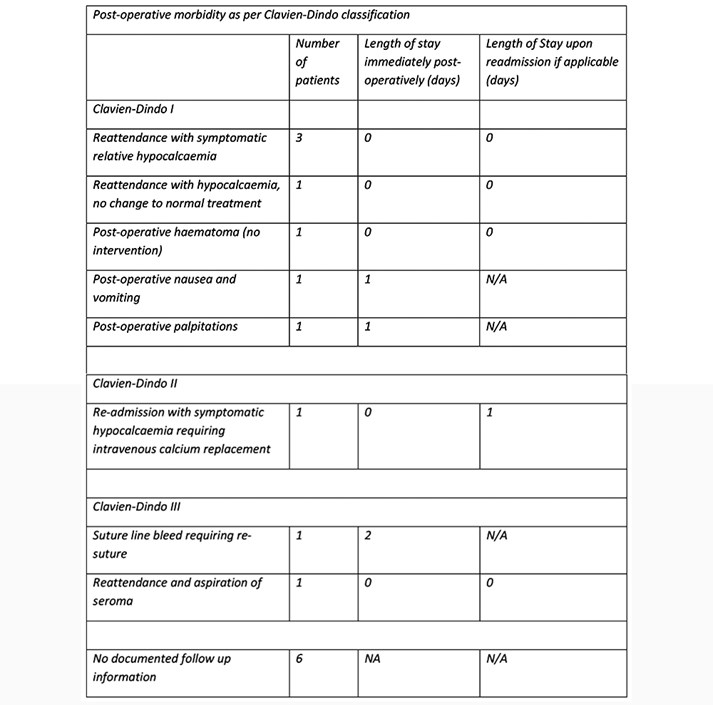
As per figure 4, there were 5 reattendances without admission and one overnight readmission within 30 days.
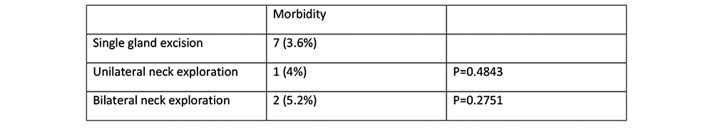
Each subset (single gland excision, unilateral neck exploration or bilateral neck exploration) was analysed for 30-day morbidity. Rates were then compared against single gland excision as the control (figure 5). There was no significant difference identified during this comparison.
Figure 5: 30-day morbidity as per subset (single gland excision,
unilateral neck exploration or bilateral neck exploration).
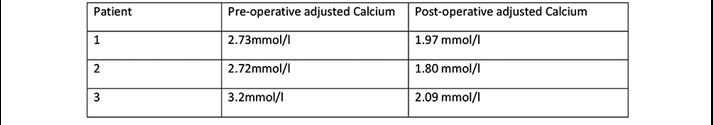
Calcium control
Three patients (figure 6) undergoing parathyroid lobectomy for adenoma had post-operative hypocalcaemia on the routine day 6 follow up blood test (adjusted calcium <2.10mmol/l). Two of the three patients were asymptomatic (adjusted calcium 1.97mmol/l and 2.09mmol/l). Oral supplementation was continued short-term and both were normo-calcaemic on repeat testing. The final patient was admitted for intravenous calcium replacement as per-previous comment.
Figure 6: Patients with post-operative hypocalcaemia compared with
pre-operative levels.
Long-term follow-up
Of our 257 patients, 9 underwent re-exploration due to persistent hypercalcaemia, with 1 patient requiring a 3rd exploration before cure. One patient continued to have persistent hypercalcaemia despite repeat neck exploration. The overall failure rate after the first operation is therefore 3.8% (comparable with reported BAETS figure of 4.4%) (8).
Discussion
The BAETs audit reports of 2012 and 2017 show a trend towards same-day or day-case parathyroidectomy, but the rate in 2017 was still only 10%. The latter report suggests that one reason for reticence in adopting same-day discharge routinely is concern about missing post-operative bleeding, specifically that which can cause airway compression. The BAETS audit reports an incidence of post-operative haemorrhage requiring re-operation as 0.4%. Most of the literature concentrates on post-thyroidectomy bleeding rather than post-parathyroidectomy. Reported rates of post-thyroidectomy bleeding (requiring surgical intervention) are reported between 0.7%-0.8% (9-10). There are very few cohort studies concentrating solely upon patients undergoing parathyroidectomy, however within broader studies (including both parathyroidectomy and thyroidectomy) when just analysing parathyroidectomies, bleeding requiring re-operation has a lower incidence of just 0.3% (9,10). No significant difference in the incidence is found with varying operative approaches, be that focused single gland excisions or bilateral neck explorations (10).
Another reason for post-operative admission is to avoid undiagnosed hypocalcaemia. Incidence of hypocalcaemia post-parathyroidectomy is reported between 20-30% (12-15), with a higher risk of hypocalcemia following re-operation. Some studies have suggested that problematic hypocalcaemia becomes most likely around day 3-5 (12,13), so traditional practice of testing levels 24 hours post-operatively is not of benefit. Our results suggest it is safe to wait until day 6-7 before checking the postoperative calcium level, unless patients are symptomatic. All of our patients are given instruction on symptoms to be aware of and contact details if they have any concerns. With a single surgeon practice, it has often been the case that patients contact the surgical team directly who will arrange for immediate serum testing and review if needed.
Ours is not the first discussion of whether or not same-day discharge is safe (1-7). Several of these papers originate in the USA (1,2,3) where ambulatory surgical practice is more common. In the UK a large retrospective cohort study (7) (including both thyroid and parathyroid surgery) was carried out and concluded that day-case surgery is a safe option. Even this study reported same-day discharge of just 40% of patients post parathyroidectomy. Our data shows that it is safe to adopt day-case surgery as normal practice.
It is unclear why the surgical community has yet to embrace same-day discharge after parathyroidectomy. Both the current literature and our results offer reassurance it is a safe option. With such a simple regime of oral supplementation and easy access to review it seems something all units could adopt.
Our unit uses what some consider a more invasive approach, with all patients undergoing a standard neck incision. This is due to surgical preference as the operating surgeon has been disappointed with the results of “minimally invasive parathyroidectomy”. Despite this, the overall day-case rate is still 95%. As expected, there is a higher day-case rate in those undergoing unilateral parathyroid exploration (96%), although the day-case rate with bilateral neck exploration is still well above that reported elsewhere (84%).
Conclusion
Day-case parathyroidectomy is safe in the majority of patients undergoing surgery for primary hyperparathyroidism. Symptomatic hypocalcaemia can be minimised using postoperative oral calcium/vitamin-D supplements. Routine postoperative calcium and vitamin D supplementation means that close calcium monitoring is not required in the immediate postoperative period and serum calcium testing can safely be postponed until day 6 or 7 postoperatively. At this stage the main value of testing allows for identification of patients with persisting hypercalcaemia. If patients are found to have a raised calcium at day 6 - 7 postoperatively the supplements are stopped.
We acknowledge there may not be many units which run a single surgeon service such as ours, which in many ways confers a natural advantage to streamline services. We feel most units should be able to adopt a similar approach and provide patients with a simple consistent post-operative routine to ensure appropriate calcium monitoring with good use of outpatient resources.
Instructions on post-operative medications and when to undergo blood tests are given on the day of surgery. All patients have out-patient pathology forms given to them and they are able to present to drop-in phlebotomy services on the day(s) specified. As results are expected they are chased up and patients contacted directly with any modifications to calcium supplements.
Follow up is routinely 10 days post-operatively, with an expectation to overbook clinics when required to ensure this is not delayed. Whilst increasingly difficult to guarantee outpatient capacity, especially given the current situation, these systems lend themselves well to adaptation with out-patient blood testing alongside routine telephone outpatient follow up.
In the most recent BAETs audit a total of 13,012 parathyroid operations were recorded over a 5-year period. Of these 11,463 were patients undergoing parathyroidectomy for primary hyperparathyroidism. If all units nationally moved towards day-case procedures at a rate comparable to ours (93%) this could represent a saving of 9,514 bed days during the audit period, or 1,903 bed days per year. With ever increasing demands on hospital resources it is of utmost importance we develop more day-case practices where safe to do so.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/43855/304-chang.pdf