Successful strategies to expand the scope of day case hand and wrist surgery and avoid unplanned admissions « Contents
Matthew Allan Jonesa, Dan Morellb, Chrishan Mariathasc, Meg Birksd
aConsultant Hand and Wrist Surgeon, University Hospital Coventry
bConsultant Hand and Wrist Surgeon, Doncaster and Bassetlaw Teaching Hospitals
cHand Fellow
dConsultant Hand and Wrist Surgeon, Sheffield Hand Centre
Sheffield Hand Centre, Northern General Hospital, Herries Road, Sheffield S5 7AU
Corresponding author: Matthew Allan Jones, Consultant Hand and Wrist Surgeon, Orthopaedic Offices, Level 5, University Hospital Coventry, Clifford Bridge Road, Coventry CV2 2DX . Email: Matthew.jones2@uhcw.nhs.uk
Key words: Unplanned admission; unanticipated admission; day surgery; hand surgery
Acknowledgements
The authors wish to acknowledge and thank Georgina Jones, Professor of Health Psychology at the School of Social Sciences at Leeds Beckett University for her assistance with statistical analysis.
Conflicts of interest statement
No funding was received and there are no conflicts of interest.
Abstract
Introduction: The UK Department of Health recommends that 75% of elective surgery should be undertaken as a daycase with an unplanned admission rate below 3%. Most hand surgery is undertaken with the intention of discharge on the day of admission. We sought to establish our unplanned admission and readmission rates, and implement changes in practice to improve these.
Methods: A hospital database review identified the number of patients treated at the hand centre with a length of stay of more than 0 days, or readmission within 48 hours. The patient records were analysed for factors which may indicate the need for an overnight stay. Reasons for admission were recorded. Changes were made to post-operative analgesia and patient information leaflets. Regional block techniques were refined and more widely used. The process was then repeated to establish the efficacy of the changes.
Results: From April 2012 to March 2014, 4407 patients were admitted to the hand centre. Sixty-six had an unplanned overnight stay or readmission (1.50%). Common reasons were pain and post-operative nausea and vomiting. After the changes were implemented, a repeat review from April 2016 to June 2016 identified 886 admissions with only 3 having an unplanned overnight stay (0.34%).
Conclusions: Attention to timing of surgery, anaesthetic techniques, post-operative analgesia, patient information and social arrangements can minimise unplanned admission rates in daycase hand surgery at minimal cost.
Introduction
Guidance introduced by the UK Department of Health recommends that 75% of elective surgery should be undertaken as a daycase with an unplanned admission rate below 3% (1). Unplanned admissions and readmissions after daycase surgery are undesirable from both the patients’ and the healthcare provider’s perspective for financial, operational and quality reasons. Daycase surgery is preferred by the majority of patients due to convenience, reduced requirement for social arrangements, and a reduction in the likelihood of acquiring a nosocomial infection (2-4). Avoiding an overnight stay results in a significant saving for healthcare commissioning groups.
The aim of this study was to assess the rate of unplanned admissions and readmissions after daycase hand surgery at a tertiary referral adult hand centre. The centre is based in a UK teaching hospital serving a local population of 500,000 and an extended catchment of 3 million, where the majority of elective and trauma work is carried out on an ambulatory, same day discharge basis. Improvements to the service to reduce these rates were sought.
Methods
The first phase of the study was to carry out a retrospective review of performance. All patients admitted under the care of hand surgery consultants over a two year period (1st April 2012 to 31st March 2014) were identified from the hospital databases. Those with a length of stay (LOS) greater than zero days were identified and each case investigated. ‘Daycase’ was defined as admission and discharge on the same day (i.e. no overnight stay). Patients with planned overnight stay as per their operation note and incorrectly recorded cases of overnight stay were excluded.
Routine admission was anticipated for patients undergoing total wrist arthroplasty, brachial plexus surgery or those requiring inpatient neuro-rehabilitation post-operatively. Trauma patients requiring intravenous antibiotics, observation of neurovascular status and monitoring for the development of compartment syndrome were also considered planned admissions and therefore excluded. Those who had been discharged on the day of surgery but then readmitted within 48 hours were also identified and included.
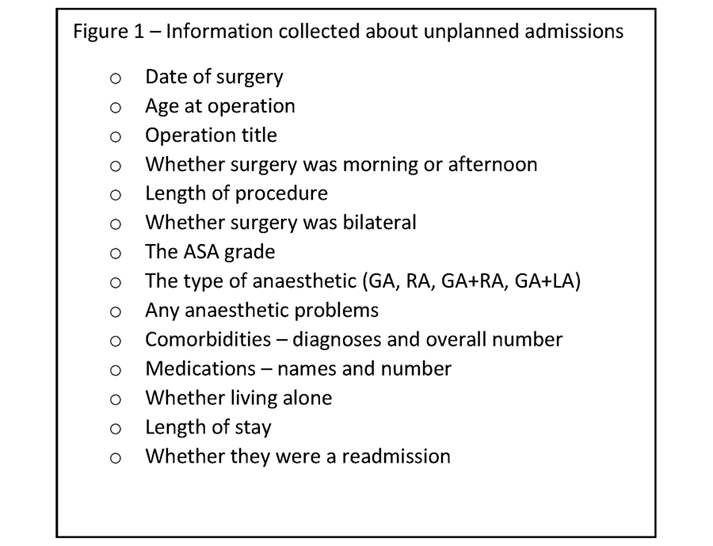
Electronic and paper case notes were scrutinised for demographics and details surrounding the care episode (figure 1). Data were analysed with the assistance of a statistician and Chi-squared tests were carried out using SPSS.
Figure 1 – Information collected about unplanned admissions.
The first phase identified post-operative pain as the main reason for unplanned admission. The following strategies were formulated in collaboration with colleagues in anaesthetics to mitigate this problem:
- Addition of ibuprofen to the take-home analgesic medications for 48 hours post-operatively for all patients, including those having bony surgery, unless contraindicated.
- Introduction of a post-operative analgesia patient information leaflet to augment the verbal information provided at discharge (figure 2)
- Refinement of the regional anaesthetic techniques for hand and wrist surgery using a short-acting brachial plexus block and long-acting peripheral nerve block to enhance post-operative analgesia without an associated flail limb
- The anaesthetic team expanded the number of clinicians trained in the administration of regional anaesthesia, including a number of Physicians’ Assistants, ensuring almost all hand surgery lists are staffed by someone competent in ultrasound-guided regional anaesthesia.
The second phase of data collection was then carried out in the same way as the first, for a three month period, after the interventions to assess their effect.
Figure 2 – Post Operative Pain Relief Patient Information Leaflet.
Results
First phase
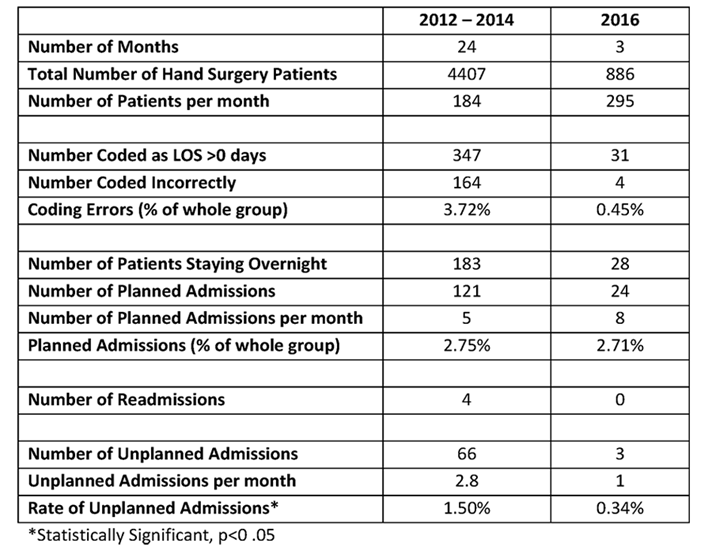
During the first study phase (April 2012 to March 2014) 4,407 patients were admitted via the hand centre. A flow chart detailing the fate of those individuals can be seen in figure 3; 62 were unplanned admissions on the day of surgery. In addition there were four readmissions in the first 48 hours after surgery. The total number of unplanned admission at this time was 66 making the rate of unplanned admissions 1.5%. Thirty-two were male and 34 female.
Figure 3 – Flow chart of Patient Cohort Phase 1 (April 2012 – March 2014).

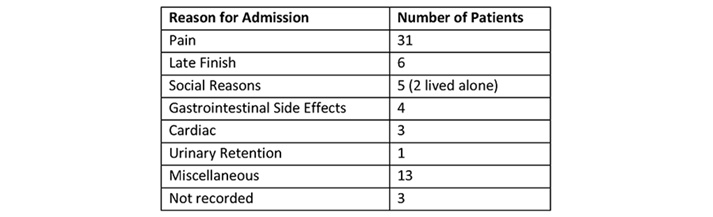
Other features of the group are shown in Table 1. Of these 66 patients, 17 lived alone, 30 lived with someone and for 19 their home circumstances were not recorded. The reasons for admission are shown in Table 2.
Table 1 – Patient Demographics and General Information.
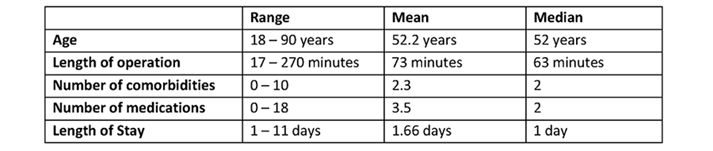
Table 2 – Reason for Overnight Admission.
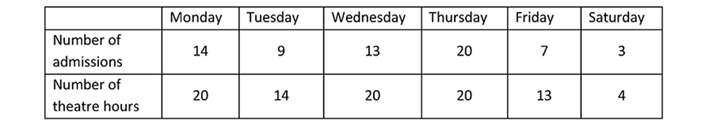
Time of surgery is shown in table 3. Operations carried out in the afternoon were markedly more likely to result in an unplanned admission. However, the day of the week was not linked to likelihood of admission (table 4).
Table 3 – Time of Day Surgery Performed.
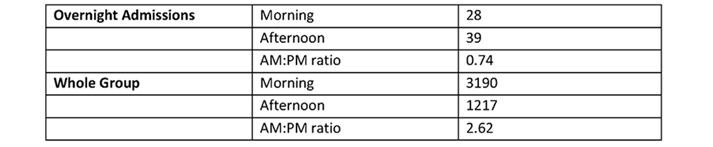
Table 4 – Day of the Week Surgery Performed.
The type of surgery had a clear influence on unplanned overnight admission. The total number of unplanned admissions per operation, or type of operation, is presented in Table 5 along with the total number of those procedures carried out by the Hand Service during that period. Statistical analysis reveals that Ulna Shortening, Brunelli Ligament Reconstruction, Corrective Osteotomy (all) and Open Reduction Internal Fixation (ORIF) (all) each had a significantly higher chance of being admitted (p value <0.01). Soft Tissue Procedures have a significantly lower risk of unplanned admission, p <0.01.
Table 5 – Rate of Admission by Type of Surgical Procedure.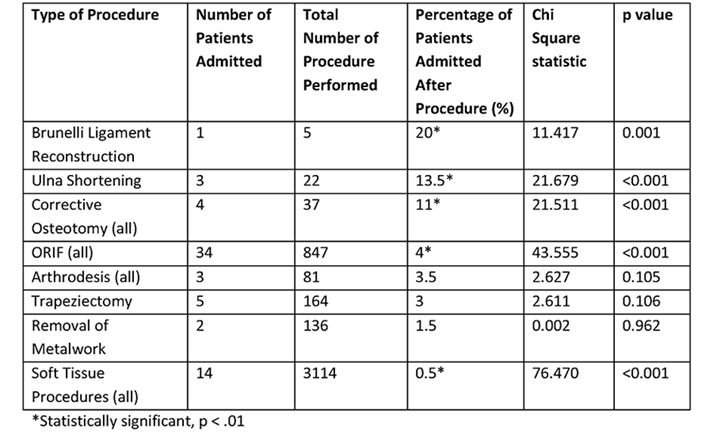
Assessment of whether anaesthetic factors contributed to unplanned admission was hampered by inability to obtain detailed anaesthetic information for the group successfully treated as day patients. The modal ASA grade in the unplanned admission group was 2 (range 1-4).
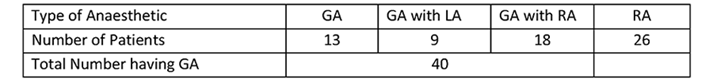
The type of anaesthetic received by these patients is shown in Table 6. In the unplanned admission group, GA represented all or part of the technique for 61% of patients. Data regarding combined anaesthesia (GA with RA or local anaesthesia) is not recorded in a format that can be easily retrieved and assessment of large numbers of successful day case hand surgery patients was not feasible. During the initial study period 20% of all hand surgery patients received a general anaesthetic (GA).
Table 6 – Type of Anaesthetic.
Second phase
To evaluate the changes in practice, the second phase was carried out from April to June 2016. During this period 886 patients were admitted to the hand centre for hand surgery (figure 4). This number is similar to the number admitted in April-June 2012 and April-June 2013 (during the first phase), accepting a gradual increase in the activity of the unit over time. Of these, 31 were coded as having a length of stay greater than zero days. There were only four coding errors in this sample. The rate of coding errors reduced from 3.6% in 2012-14 to 0.45% in 2016.
Figure 4 – Flow chart of Patient Cohort Phase 2 (April 2016 – June 2016).
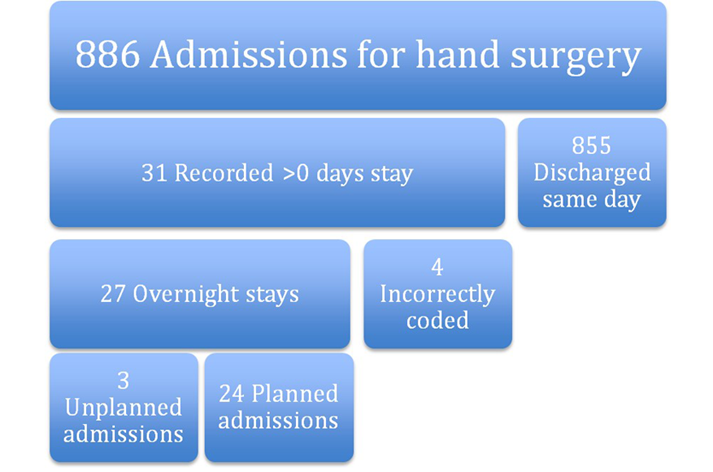
There were 24 planned admissions; the majority were for post operative intravenous (IV) antibiotics. The rate of planned admissions remained static. There were three unplanned admissions, a rate of 0.34%. Table 7 shows a comparison of the two study periods. The reduction in unplanned admissions is significant at p < 0.05. Of note there was a reduction from approximately one in two to one in three unplanned admissions resulting from pain.
Table 7 – Comparison of 2012-14 and 2016 Study Periods.
Discussion
Phase one of the study identified that almost half of unplanned admissions were attributed to inadequate pain control. This is in keeping with other studies which also cite bleeding and post-operative nausea and vomiting (PONV) as common reasons (5-13). The changes implemented regarding anaesthetic techniques and post-op analgesia contributed to the improved rate of successful daycase surgery.
Procedures on bone were more likely to result in unplanned admission. In a hand surgery cohort, Goodman et al found more invasive surgeries had higher complication rates (9). Other studies have found that the type of surgery undertaken, and the specialty delivering the care, have a profound effect. General surgery, urology and gynaecology are associated with higher rates of admission (6, 10, 14). Rates of unplanned admission can be as high as 30% (11) for procedures such as laparoscopic cholecystectomy, whereas for orthopaedic day cases, rates tend to be much lower. Cardosa et al published a 1.07% admission rate in daycase knee arthrosopy patients at an orthopaedic centre (15). Minatti et al found a post-discharge admission rate of 1% within 30 days, halving to 0.49% when only including the orthopaedic cohort (14). Our rate of 0.34% in phase two of our study is compares favourably to other published studies, partly due to the suitability of regional and local anaesthesia in hand surgery and the minimal impact on patient mobility. Goodman et al found an even lower rate of 0.15% based on a 30 day reoperation and/or admission rate in an elective hand surgery population (9). The majority of their admissions/operations happened in the second post-operative week and these were mostly due to infection. This usually takes longer than 48 hours to present, and therefore there may be a group of patients in our cohort who were admitted later than 48 hours post op and are therefore not identified by our study. Furthermore, some complications can present much later such as tendon rupture.
Lack of suitable social support can sometimes prevent safe discharge – accounting for 5 cases of unplanned admission in this study – but this can usually be pre-empted and suitable arrangements made. Others have also found social reasons to be a factor in unplanned admission (5, 10, 12, 13, 16).
Some of our patients may have had a minor complication and presented to their general practitioner rather than the hospital, and these patients would not have been captured by the study.
Duration and timing of surgery are also risk factors for unplanned admission. Both Garcea and Soler-Dorda found that unplanned admissions/readmissions had significantly longer operation times (7, 11). Surgery in the afternoon was a negative factor in our study. Thus one way of reducing unplanned admissions could be to undertake longer, more complex and bony surgeries earlier in the day. Smaller cases, that are less likely to require an overnight stay, can be done in the afternoon.
We found no particular trends in patient factors such as age, ASA grade or number of comorbidities in the admitted group. In contrast, Soler-Dorda found age >65, and Minatti age >90 to be statistically significant risk factors (11, 14). An ASA greater than 2 has been associated with higher admission rates (11, 12).
Obstructive sleep apnoea in children has also been identified as possible risk factors for admission (12), but Bryson found no such association with obstructive sleep apnoea in adults (17).
Administration of general anaesthesia was another risk factor for admission. This finding helped to inform and drive further development of the regional anaesthesia service in our unit, and was addressed by the third of our interventions after phase one. Most hand patients undergoing hand surgery do not need to have a general anaesthetic, making them ideal candidates for daycase surgery. Most patients in our study who had combined general and regional anaesthesia had experienced an inadequate regional block, but this block may well have helped their post-operative pain. For safe discharge and effective post-operative analgesia, we recommend that general anaesthesia alone is insufficient, especially for bony surgery.
Our study is limited by the lack of a control group, which would more robustly have identified risk factors for admission. We studied readmission rates at 48 hours post-discharge. This identified early post-operative problems such as pain and nausea, but will not have captured infections as these will generally represent later. We did not set out to establish infection rates, which are known to be low in hand surgery in general (9).
The cost of our interventions was minimal. The development of a patient information leaflet cost very little, and the majority of patients buy their own ibuprofen over-the-counter.
Coding errors have reduced in our unit thanks to a new patient administration and tracking system. Patients are discharged or transferred electronically, reducing the potential for errors, improving the information available to general practitioners and other healthcare providers and providing a more robust audit trail.
Low cost improvements in post-operative pain control and anaesthetic techniques resulted in a demonstrable improvement in unplanned admission/readmission rates in our centre. Similar interventions could be undertaken in other units for the mutual benefit of patients and healthcare providers.
References
- Royal College of Surgeons of England. Commission on the provision of surgical services. Guidelines for day case surgery. London: HMSO, 1992.
- Peplow J, Randall E, Campbell-Cole C, Kamdar R, Petzer E, Dhillon P, Mergatroyd F, Scott P. Day-case device implantation – A prospective single-center experience including patient satisfaction data. Pacing Clin Electrophysiol. 2018 May;41(5):546-552.
- Ridings LM, Colby JM, Burch NE. Evaluation of patient satisfaction following percutaneous endoscopic gastrostomy (PEG) insertion: day case versus in-patient model in UHCW NHS Trust. Gut 2014;63(Suppl 1):A229.
- Tysome JR, Padgham ND. A comparative study of patient satisfaction with day case and in-patient major ear surgery. J Laryngol Otol. 2006 Aug;120(8):670-5.
- Aldwinckle RJ1, Montgomery JE. Unplanned admission rates and postdischarge complications in patients over the age of 70 following day case surgery. Anaesthesia 2004 Jan;59(1):57-9.
- Barros AL, Duque MR, Nunes F, Ribeiro S, Ventura C, Assuncao JP. Five year retrospective study of unanticipated admission after ambulatory surgery. Eur J Anaesthsiol, 2014 Jun;31(SUPPL. 52):27.
- Garcea G, Majid I, Pattenden CJ, Sutton CD, Neal CP, Berry DP. Predictive factors for unanticipated admission following day case surgery. J Eval Clin Pract. 2008 Feb;14(1):175-7.
- Gold BS, Kitz DS, Lecky JH, Neuhaus JM. Unanticipated admission to the hospital following ambulatory surgery. JAMA 1989 Dec 1;262(21):3008-10.
- Goodman AD, Gil JA, Starr AM, Akelman E, Weiss AC. Thirty-Day Reoperation and/or Admission After Elective Hand Surgery in Adults: A 10-Year Review. J Hand Surg Am 2018 Apr;43(4):383.e1-383.e7.
- Hardman DTA, Patel MI, Yiing D, Warden JC. The unplanned admission: a review of the daycase experience. Ambulatory Surg 1997(5):21-4.
- Soler-Dorda G, San Emeterio Gonzalez E, Martón Bedia P. Risk factors for unplanned admission after ambulatory laparoscopic cholecystectomy. Cir Esp. 2016 Feb;94(2):93-9.
- Whippey A, Kostandoff G, Ma HK, Cheng J, Thabane L, Paul J. Predictors of unanticipated admission following ambulatory surgery in the pediatric population: a retrospective case-control study. Paediatr Anaesth 2016 Aug;26(8):831-7.
- Zulfiquer FA, Pattanayak K. Evaluation of unplanned admission following day surgery at a new surgical centre in London. Ambulatory Surg 2009 Nov;15.4:93-96.
- Minatti WR, Benavides F, Capelino P, Ramos R, Premoli G, Statti M. Postdischarge unplanned admission in ambulatory surgery – a prospective study. Ambulatory Surg 2006(12):107-12.
- Cardosa M, Rudkin GE, Osborne GA. Outcome from day surgery knee arthroscopy in a major teaching hospital. Arthroscopy 1994; 10: 624-629.
- Deshpande S, Watts J. Unanticipated admission following day surgery. Anaesthesia 1998 Oct;53(10):1033-4.
- Bryson GL, Gomez CP, Jee RM, Blackburn J, Taljaard M, Forster AJ. Unplanned admission after day surgery: a historical cohort study in patients with obstructive sleep apnea. Can J Anaesth 2012 Sep;59(9):842-51.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29261/jones.pdf