Uterine Fibroid Embolisation, Time for day case? The Stoke Protocol « Contents
Authors
R. D. Wells, A. K.Allouni & S. Merron
Authors' Addresses
Wells R.D. Consultant Interventional Radiologist. Lead and corresponding author, UHNM NHS Trust, Royal Stoke University Hospital, Newcastle Road, Stoke-on-Trent ST4 6QG
Keywords
Day case, UFE, Fibroid embolisation, fibroids, radial access.
Abstract
Setting up a day case Uterine Fibroid Embolisation (UFE) service has been a challenge for Interventional Radiologists for many years. There is a body of opinion that the immediate post-procedural phase is just too painful to treat these patients on an ambulatory care basis. However, in a healthcare system under the strain of in-patient bed shortages our unit decided to review practice and find ways of delivering effective therapy to patients in more efficient ways. Clinicians believed that the service could be successfully delivered with patients going home on the same day as the embolisation. We worked with patients, anaesthetists, gynaecologists, day case and surgical assessment units to produce a practical, pragmatic approach to provide women with the option of a day case procedure. In this article we describe in detail the evolution of this successful service and the rationale for each component in the pathway.
Introduction
Prior to 2017 our strategy for managing patient’s ischaemic pain from embolising the uterine arteries relied on preoperative anti-inflammatory medications and Patient Controlled Anaesthesia (PCA) during the procedure and overnight stay. (Fig. 1).
Figure 1 Pre-2017 analgesia protocol.
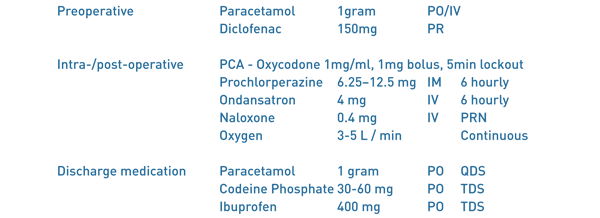
In our experience, although the PCA provided adequate pain relief in the majority of patients, a significant number had a poor experience due opioid related nausea and constipation. Indeed, these were their main complaints when seen in follow up. We also noticed that there could be significant delays in patients being discharged following an overnight stay. This tended to be due to a combination of logistical and human factors; including the PCA not being taken down in time, take home medications not being processed and nurse understaffing.
Methods
In 2017, we reviewed the then current day case analgesia practices for patients undergoing gynaecological day case surgery, including laparoscopic myomectomy. Much of this concentrated on the conduct of the anaesthetic and care given within the post-operative recovery area. We also researched other strategies employed in the management of acute peri-operative pain. For example the use of gabapentinoids within the acute pain setting. Given preoperatively this class of drugs can also provide anxiolysis for patients. There is also good evidence that gabapentinoids significantly reduce opioid consumption in the post-operative period (1,2,3)
Collaborating with an anaesthetic consultant who has a special interest in interventional radiology (4) we produced a comprehensive analgesic regime which relies heavily on preventing the ischaemic pain experienced by some women. Senior nursing staff in the interventional radiology unit, the radiology day case unit (RDCU) and Surgical Assessment Unit (SAU) were all involved in creating a patient pathway that was geared to discharging the patient on the same day, but with provision for an overnight bed for failed day case discharges. The surgical day case unit (DCU) has an overnight stay facility and, at least in the first few cases, this was booked as a fall back, but was never utilised. It was also necessary to offer a safety net for those patients who had been successfully discharged on the day of the procedure. If a patient either, required advice, or to needed to return to hospital, then it was agreed that this would be facilitated by direct access to the nursing staff on the SAU. The literature suggests an expected readmission rate of at most 10% (5, 6).
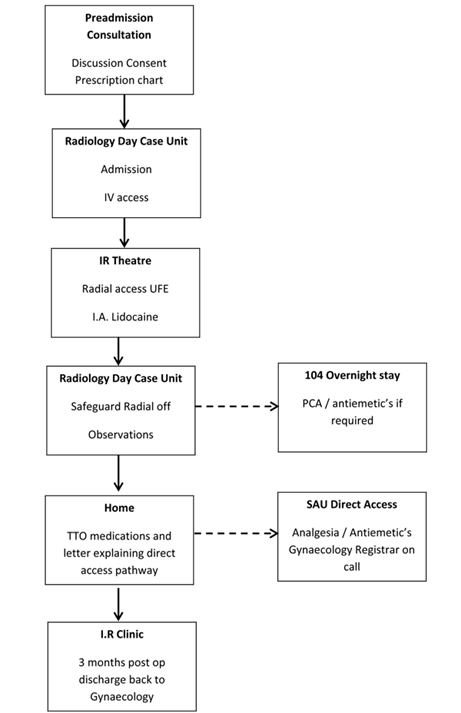
The prospect of a successful day case scenario truly emerged however, with adoption of the trans-radial (TR) arterial approach. Compared with a traditional trans-femoral (TF) approach, TR access dramatically reduces the risk of significant access site haemorrhages and allows patients to mobilise immediately (7). Closure of the radial arteriotomy is achieved using a variable compression wrist device. Once this radial band is removed, on average 40 minutes, and the discharge protocol parameters met, the patient can be safely discharged. The only issue to manage then was pain. The full day case pathway is summarised in (Fig. 2).
Figure 2 Patient pathway.
Pre-admission
Patients are referred by local gynaecologists having been diagnosed with symptomatic uterine fibroids, usually on ultrasound and clinical grounds. Most patients have not responded to or declined medical therapy. Every patient undergoes an MRI examination to characterise the size and location of the fibroids and any associated disease process such as adenomyosis. We then invite patients to a pre-assessment joint clinic run by an interventional radiologist and a specialist nurse. This affords the opportunity to council the patient on UFE, review the imaging, and allows time to go through a rigorous consent process. At this point it is often clear if patients are motivated by the prospect of a day case procedure and their pathway can be planned accordingly. All patients have routine blood tests within 30 days of the procedure; including coagulation profile, Full blood count, renal function and CRP. Pregnancy screening is completed on the day of admission.
Day case medications: rationale and mechanism of action
Figure 3 Post-2017 day case protocol.
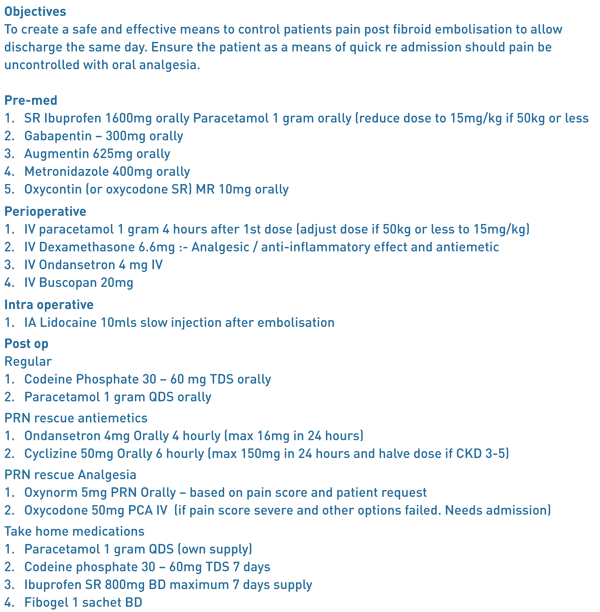
Preoperative Medication
Ibuprofen SR 1600mg orally: Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID). NSAIDs inhibit the action of the cyclooxygenase enzymes. This leads to a reduction the production of inflammatory and pain causing prostaglandins.
Gabapentin 300mg orally: Gabapentin is a gabapentinoid drug with an onset of action within 30-90 minutes after oral dosing. It activates the inhibitory Gaba-ergic receptors associated with the central NMDA receptors. It can exert anxiolytic and sedative effectives and also alters the transmission of nociception at a spinal cord level. It has been well established that gabapentinoids work synergistically with opioids and reduce overall opioid requirements. Gabapentinoids not only improve the quality of analgesia, but reduce the incidence of post-operative nausea and vomiting, by reducing opioid consumption (1,2,3). In trials, patient satisfaction with postoperative pain management was significantly higher at 24 hours following pre- and postoperative oral gabapentin compared with placebo (p<0.001) (2). However we decided that, due its sedative action, gabapentin would not be routinely used postoperatively. Similarly, we do not give intraoperative midazolam.
Oxycodone SR 10mg orally: Oxycodone is a euphoric opioid analgesic with approximately 1.5 times the efficacy of comparable morphine doses. Onset is within 30 minutes with a duration of between 4 and 6 hours.
Perioperative Medication
Paracetamol 1 gram IV: (if >50 kg otherwise 15mg/kg): The mechanism of action of paracetamol is still poorly understood. It is generally accepted that it acts on multiple levels in the pain pathways, having effects on prostaglandin inhibition, the serotonin pathway and endocannabinoid enhancement. The introduction of IV paracetamol has made the bioavailability much more predictable with a speed of onset of 5 minutes and duration of 4-5 hrs. (8,9).
Dexamethasone 6.6mg IV: This is a potent synthetic corticosteroid . It has been shown to have both analgesic and anti-inflammatory effects . It has a strong anti-emetic effect , especially when used in conjunction with other more conventional antiemetic’s (10, 11).
Ondansatron 4mg IV : This medication has powerful antiemetic properties. It exerts these through competitive antagonism of the 5-HT3 receptors within the brain.
Intraoperative Medication
Lidocaine 5ml 1% IA : into both uterine arteries . This was shown to significantly reduce the pain scores at 4 hrs and reduce the opioid requirement by up to 50% (12).
Postoperative Medication
Paracetamol 1 gram PO: Regularly. Four times daily.
Codeine Phosphate 30-60mg PO: Regularly. Three times daily.
Ondansatron 4mg IV : As required.
Oxynorm 5mg PO: As required rescue analgesia. Based on pain score.
Oxycodone 50mg PCA IV: As required rescue analgesia. If pain score is severe and other options failed. This necessitates an admission.
Discharge Medication
Paracetamol 1 gram PO: Regularly. Four times daily. 7 day supply.
Codeine Phosphate 30-60mg PO: Regularly. Three times daily. 7 day supply.
Ibuprofen SR 800mg PO: Twice daily. 7 day supply.
Fibogel 1 sachet PO: Twice daily. 2 sachets.
Discharge protocol
For patients to be safely discharged home they require transport and an adult present in their home overnight.
Figure 4.
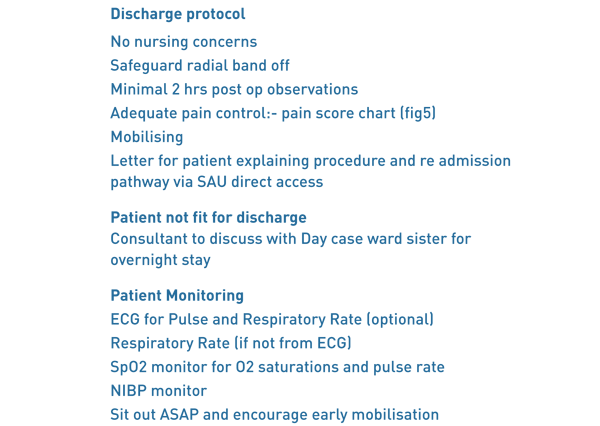
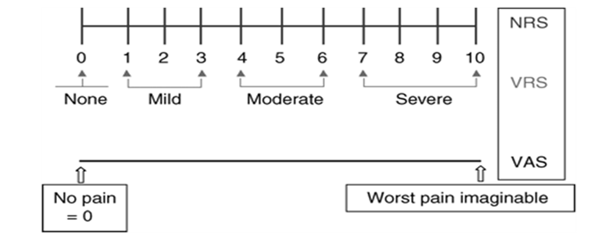
On the ward the radial arteriotomy site is checked. There is a minimum of two hours stable blood pressure, pulse and oxygen saturations. The patient’s pain score is assessed and documented (Fig. 5).
If the pain score is less than 6 and patient is able to cope then the patient is given their take home medications and a letter for direct access back to the surgical assessment unit.
Fig 5 Pain score chart.
Follow up
Following discharge, a specialist nurse conducts a telephone consultation with the patient within the following week to assess for any short term complications such as on-going pain, signs of infection or heavy discharge. Patients then return 3 months post procedure for a consultation with an interventional radiologist to assess the symptomatic outcome of the procedure. At this point, re-intervention may be discussed, often with a follow-up MRI.
Early Results
Of the first ten patients following this protocol, 9 patients were discharged before 8pm and had no complications or complaints at the 48-hour, nurse led telephone follow up. One patient progressed to an overnight stay, however, this was no due to pain or complications, but simply she had failed to disclose a lack of somebody at home to care for her in the overnight postoperative period; a fundamental criteria for day case admission. This patient did not require a PCA and was discharged home the following morning. There were no readmissions via the surgical assessment (SAU) rapid access protocol for pain or infection. Of the cases that have returned for 3 months clinic follow-up, all have been technically successful with significant improvement in symptoms. The mean screening time was 14min 65sec with a mean dose (DAP) of 549.05 mGy/cm2 .
Discussion
Day case procedures have become the mainstay of a modern NHS practice. With advances in techniques, especially radial artery access UFE, the support of a working group and increased demand from patients we have developed an evidenced based structure to deliver this patient orientated pathway in IR.
To set up a practice like this takes a coordinated approach from a preadmission IR nursing team that informs and involves the patient before the procedural day. To ensure enough recovery time, the procedure needs to first on the list in the morning and the clinicians have to promptly prescribe the preoperative medication. Ensuring the perioperative and intraoperative medication is given in a timely manner prevents the build-up pain. The pathway is followed through to the post op care, discharge and finally follow-up.
We have a strict discharge protocol (Fig. 4), if the pain score (Fig. 5) is above 6 with all the medication given, then the patient is assessed for overnight stay or even a traditional PCA. Once the patient has been discharged they are given a letter for rapid access back through the SAU to be seen by the gynaecology registrar on call.
Day case UFE lends itself well to radial access. In our institution the radial procedure has proven to be quicker with less radiation dose and the patient is free to mobilise to the bathroom, sit out or lie more comfortably in the bed than common femoral groin access. There is also no risk of a retroperitoneal haematoma and no use of a closure device.
Conclusion
Using a collaborative, evidence based approach, tailored to the specific needs of patients undergoing UFE we were able to formulate a safe, effective and validated strategy for a day case procedure. We do expect some patients to be re admitted for pain control. This should not be seen as a failure of day case, rather a safety net for some patients
References
- Effects of Gabapentin on postoperative morphine consumption and pain after abdominal hysterectomy : A randomised double blind trial. Dierking G, Duedahl TH, Rasmussen ML, Fomsgaard JS, Møiniche S, Rømsing J, Dahl JB Acta anaesthesiologica Scandinavica 2004;48(3):322-7.
- Gabapentin: An alternative to the cyclooxygenase-2inhibitors for perioperative pain management. Turan A, White PF, Karamanlioglu B, Memis D, Tasdogan M, Pamukçu Z, Yavuz E. Anaesthesia and analgesia 2006;102(1):175-81
- Efficacy of pregabalin in acute postoperative pain: a meta-analysis. Zhang J, Ho KY, Wang Y. Br J Anaesthesia. 2011 Apr;106(4):454-62.
- The Royal College of Radiologists. Sedation, analgesia and anaesthesia in the radiology department, second edition. Ref BFCR (18)2
- Tolerance, Hospital Stay, and Recovery after Uterine Artery Embolization for Fibroids: The Ontario Uterine Fibroid Embolization Trial. Pron, Gaylene et al. Journal of Vascular and Interventional Radiology, Volume 14, Issue 10, 1243–1250
- Outpatient uterine artery embolization for symptomatic uterine fibroids: experience in 49 patients. Siskin GP, Stainken BF, Dowling K, Meo P, Ahn J, Dolen EG. J Vasc Interv Radiol 2000;11:305–311.
- Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. Kolkailah AA1, Alreshq RS, Muhammed AM, Zahran ME, Anas El-Wegoud M, Nabhan AF. Cochrane Database Syst Rev. 2018 Apr 18;4:CD012318. doi: 10.1002/14651858.CD012318.pub2
- What anaesthesiologists should know about paracetamol (acetaminophen), Minerva Anestesiol , Mattia C, Coluzzi F. 2009, vol. 75 pg. 644-53
- Intravenous acetaminophen: a review of pharmacoeconomic science for perioperative use, Am J Ther , 2Jahr JS, Filocamo P, Singh S. 2013, vol. 20 pg. 189-99
- Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis N. H. Waldron C. A. Jones T. J. Gan T. K. Allen A. S. Habib BJA: British Journal of Anaesthesia, Volume 110, Issue 2, 1 February 2013, Pages 191-200
- The cellular mechanisms of the antiemetic action of dexamethasone and related glucocorticoids against vomiting. Eur J Pharmacol. 2014 Jan 5;722:48-54. Chu CC1, Hsing CH2, Shieh JP3, Chien CC4, Ho CM5, Wang JJ6.
- Intra-arterial Lidocaine for Pain Control in Uterine Artery Embolization: A Prospective, Randomized Study. Noel-Lamy M1, Tan KT2, Simons ME2, Sniderman KW2, Mironov O2, Rajan DK2. J Vasc Interv Radiol. 2017 Jan;28(1):16-22.
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2018-journal/jods-284-december-2018/uterine-fibroid-embolisation-time-for-day-case-the-stoke-protocol/
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6045/284-wells.pdf