Enhanced recovery in major vascular surgery « Contents
Authors: Ajit Dhillon & Tim Rowlands
Derbyshire Vascular Services, Royal Derby Hospital, Derby.
Enhanced recovery after surgery (ERAS) also known as fast track surgery is a multimodal post-operative recovery programme. It is based on the concept that postoperative recovery is determined by numerous factors associated with the preoperative, intraoperative and postoperative phases. The preoperative phase where existing organ dysfunction is recognised and improved; the intraoperative phase, which is determined by the anaesthetic and surgical techniques, and, postoperative phase which concentrates on analgesia, fluid management, nutrition, mobilization, nursing care and a planned recovery programme. It is a multi-disciplinary approach with an emphasis on regional anaesthesia and postoperative non-opioid analgesia being used sparingly. As more specialities take on board the ERAS model, it is being recognised that a procedure-specific approach is important (Kehlet, 2009)1. The goal of ERAS is not necessarily about reducing length of stay but to achieve a pain and risk free operation whilst recognising the postoperative stress response with inevitable organ dysfunction (Kehlet, 2015)2.
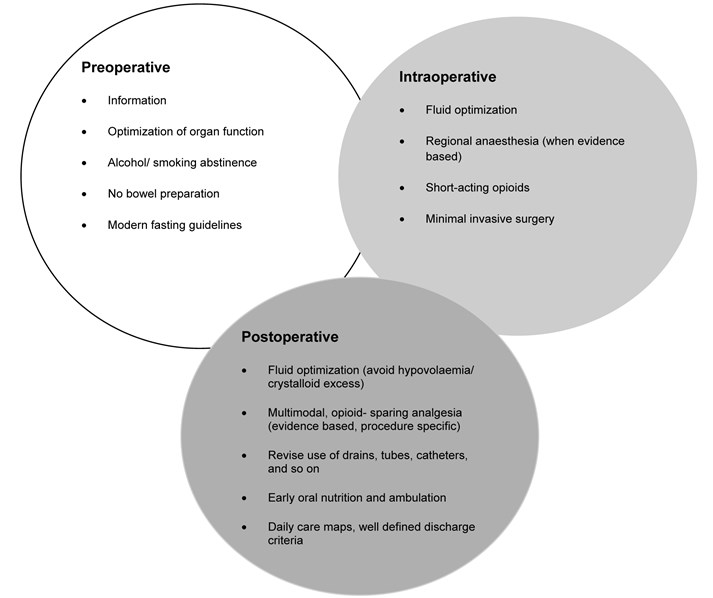
The usefulness of ERAS is well established in colorectal surgery but there is very limited literature about its application in major, non-cardiac vascular surgery. The principles of ERAS in their current form, as shown in Figure 1 (Kehlet, 2009)1, may not all be relevant to non-cardiac vascular surgery but, with appropriate modification may prove useful.
We aim to review the factors that are known to extend length of postoperative stay and associated with mortality as a method of assessing modifiable factor that may contribute towards a procedure specific ERAS approach in open repair of abdominal aortic aneurysms (AAA), carotid endarterectomy (CEA), infra-inguinal lower extremity bypass (LEB) and major lower limb amputation (LLA). We have excluded asymptomatic patients undergoing CEA as there is still little clarity in practice.
Figure 1. Principles of the fast- track methodology to enhance postoperative recovery (must be procedure specific).
Open repair of abdominal aortic aneurysm (AAA)
A non-randomised prospective study of ERAS in open repair of AAA involved the implementation of a modified ERAS programme in 52patients undergoing surgery after 2008, and, conventional care in 75 patients operated upon prior to 2008. The modifications included counselling in the out-patient setting and upon hospital admission; the day before surgery patients were permitted a low residue diet until the evening, followed by an enema and permitted to drink fluids and juices until the morning of the day of the surgery. In the post-operative phase, patients were allowed to drinks fluids 3hours after extubation, with administration of pro-kinetic anti-emetics. Patients were encouraged to consume high calories in the form of fat emulsions alongside administration of amino acids and glucose. The surgical wound was protected with a specified highly waterproof dressing. Post-operative transfusion was kept to a minimum, only to maintain haemodynamic stability. The only statistically significant difference between the groups was coronary artery disease, 36% and 57.7% respectively, p=0.04. Postoperative complications in the ERAS group consisted of one case each of deterioration in renal function, surgical site infection and anastomotic stenosis. Yet in the conventional care group 8patients had complications, 2 cases of deteriorating renal function, 3 cases of surgical site infection, 2 cases of pneumonia and 1 case of cerebral infarction. Ileus is the most widely recognised primary morbidity associated with an open repair of AAA. Patients in the ERAS group were allowed to resume a diet when they started to pass flatus, this shortened the time to meal consumption to 59+/- 15hours after surgery compared with 93+/- 25hours in the conventional management group. The shorter length of stay was statistically significant in the ERAS group at 9+/- 3day compared with 16+/- 5days (p=0.001) in the conventional management group (Tatsuishi, 2012)3. Impaired lung function has been shown to have an inverse association on length of stay following elective open repair of AAA. Preoperative lung function tests to assess forced expiratory volume in one second (FEV1), with FEV1 <1.9L was associated with a mean stay of 15.0 +/- 1.43 days, reducing incrementally with increasing FEV1 until patients with FEV1 >2.5L, had a mean stay of 11.2 +/- 0.3days. Impaired respiratory function will have an existing negative impact on a patients functional ability but will also increase the risk of postoperative prolonged intubation, development of pneumonia and respiratory failure. Preoperative smoking also increased length of stay although it failed to reach statistical significance. Preoperative blood results such as haemoglobin levels, patient age and gender, previous myocardial infarction failed to show an impact on length of stay. Preoperative myocardial infarction was not directly associated with postoperative myocardial infarction (UK Small Aneurysm, 1998)4.
Chang et al report (Chang, 2003)5 outcomes of a modified early form of ERAS type pathway. The patients were counselled pre-operatively, that their expected length of stay (LOS) would be less than 5day without complications. The main difference compared with the currently accepted ERAS pathway was routine intra- and post-operative monitoring with arterial as well pulmonary artery catheterisation, and, liberal administration of intra-venous fluids in the first 24-48hours to allow for third-spacing and based on pulmonary catheter monitoring. The mean LOS for ‘complicated recovery’ was 13.8+/- 6.7days but 6.9+/- 2.9 days in ‘uncomplicated recovery’. Kaplan- Meier analysis of factors significantly increasing LOS in the pre-operative phase were age above 75years of age and chronic obstructive pulmonary disease (COPD); intra-operative factors including blood loss more than 500ml, duration of surgery more than 5hours; post-operative factors including any complications but specifically wound infection. Factors that would be expected to affect LOS but did not in this study was history of cardiac disease including coronary artery bypass graft (CABG), myocardial infarction (MI), congestive heart failure (CHF), aortic stenosis and ventricular arrhythmia. The data was re-analysed using Cox regression and the significant pre-operative factors prolonging LOS were age over 75years and COPD and, any post-operative complications. Duration of surgery above 5hours (p=0.684) and the arbitrary threshold of 500ml blood loss did not reach statistical significance. A further review (Huber, 2001)6 of outcomes after open repair of AAA in 16, 450 patients with mean age 72+/- 7 years not following an ERAS type pathway reported a median LOS of 8 days (mean 10.0 +/- 8.1). The factors associated with in-hospital mortality were increasing age, 70-79years, odds ratio (OR) 1.8 and, over 79years, OR 3.8; female gender, OR 1.6. The presence of more than 3 co-morbidities, OR 11.2, whereas presence of 2-3 co-morbidities had OR 3.2 but did not reach statistical significance (p=0.06). The individual pre-operative co-morbidities associated with increased mortality were cerebrovascular disease OR 1.8, renal insufficiency OR 9.5, whereas COPD did not reach statistical significance with OR 1.0 and p= 0.67.
UK registry data for a 3-year period, January 2012 to December 2014 for open and endovascular repair of AAA found that (Watson, 2015)7 reported the median LOS post open repair was 8days (range, 7-12days), including up to 2days spent on a level 2 or 3 critical care unit in 95% of cases, before returning to the main ward. Post-operative ‘defined complications’ refer to body systems but no specific complications. The nationally reported complications were cardiac 5.7% (95% CI 4.6- 7.0), respiratory 12.3% (95% CI 10.7- 14.1), haemorrhage 2.1% (95% CI 1.4- 2.9), limb ischaemia 3.3% (95% CI 2.4- 4.3), renal failure 4.2% (95% CI 3.3- 5.4) and, other 0.8% (95% CI 0.4- 1.4). 6.7% (95% CI 5.5- 8.1) returned to theatre and 30-day re-admission rate of 5.7% (95% 4.4- 7.3%). The in-hospital risk- adjusted mortality for elective open repair of AAA was 3.0%.
A prospective randomised trial (Muehling, 2009)8 in patients undergoing open repair of infra-renal AAA using the basic elements of ERAS; no bowel preparation, reduced pre-operative fasting, patient controlled epidural analgesia, enhanced post-operative feeding and post-operative mobilisation. Fewer of the ERAS group (6.1% versus 32%, p=0.002) required post-operative ventilation, earlier enteral feeding in the ERAS group (5 versus 7days, p<0.0001) and fewer post-operative complications (16% versus 36%, p=0.039). The LOS was shorter in the ERAS group (10 days versus 11 days, p=0.016) with 0% mortality rate in both groups.
A pooled analysis of case series (Gurgel)9 analysing the cumulative results for 1, 250 patients following an ERAS pathway and 1, 429 patients following a conventional care pathway found a mortality rate of 1.51% (95% CI 0.009, 0.0226) and 3% (95% CI 0.0183, 0.0445) respectively. The post-operative complication rate was 3.82% (95% CI 0.0259, 0.0528) and 4% (95% CI 0.03, 0.05) respectively. Sub-group analysis of post-operative complications found acute MI, 1.77% (95% CI 0.0103, 0.0270) and 2.9% (95% CI 0.019, 0.042); renal failure requiring renal replacement therapy, 2.79% (95% CI 0.0159, 0.432) and 0.69% (95% CI 0.0030, 0.0123); stroke, 0.26% (95% CI 0.0005, 0.0063) and 1.8% (95% CI 0.0091, 0.0299) respectively. The authors cite clinical and methodological heterogeneity between the case-series included in the pooled analysis. This included difference in the elements and indeed the number of ERAS elements implemented in each series. This may be a large contributing factor to their conclusion that outcomes were similar in both ERAS and conventional care groups.
Carotid endarterectomy (CEA)
The UK guideline issued by National Institute for Health and Care Excellence (NICE) 10 recommend a 2week target from initial symptoms to surgery and accept that some patients may become symptomatic with a carotid artery stenosis of 50- 99%. The UK registry for Jan- Dec 20147 analysed data submitted for 4862 interventions carried out on 4464 patients undergoing. A majority of 44.9% patients had an occlusion of 70-89%, 24% had 50-69% stenosis and 28.8% had 90-99% stenosis. 92.4% of patients were already commenced on anti-platelet therapy, 87.4% on statin therapy, 25.6% on beta-blocker therapy and 37.4% on ACE inhibitor therapy. There was variation in surgical and anaesthetic techniques employed such as 52% of patients had general anaesthetic only compared with 27.3% receiving local anaesthetic. Carotid shunt was used in 49.6% of cases with 73.3% having endarterectomy and patch. Post-operatively, 45.8% of patients were admitted to either level 2 or level 3 critical care with a median LOS of 1 day in each. The overall LOS was 4 days (2-6). The recognised complications following CEA are MI, bleeding, cranial nerve injury and stroke. In the review period the complication rates for major complications were MI, 0.9% (95% CI 0.8- 1.1), bleeding, 2.8% (95% CI 2.6- 3.1), death and/ or stroke within 30days, 2.0% (95% CI 1.8- 2.2) and, cranial nerve injury, 1.6% (95% CI 1.4- 1.8)7. The registry data did not allow for analysis of when complications occurred and what factors delayed discharge.
A retrospective review of unit data (Sheehan et al; 2001) 11 for 835 consecutive patients found 62patients (8.0%) experienced either a neural deficit (26 patients, 3.4%) or neck haematoma (36patients, 4.7%) within 24hours of surgery. Further breakdown of those experiencing complications showed 24patients (66%) experienced neck haematoma and 19patients (73%) experienced neural deficit whilst still in the operating theatre or in the recovery area, 11patients (31%) had neck haematoma and 5patients (19%) had neural deficit within 8hours with the remaining patients exhibiting signs beyond 8hours. They excluded 64patients from the analysis because having had another operation, concomitant coronary bypass grafting or required heparinization. Unfortunately they excluded patient who experienced complications beyond the first 24hours10. A detailed review of 421 patients who underwent CEA carried out by 2neurosurgeons12 (Angevine et al, 1999), Cohort I, 171 patients had CEA following a conventional care pathway, Cohort II, 295patients had CEA when the unit was instituting a stay reduction policy on selected patients, and, Cohort III, 155 patients who had CEA after institution of a universal single-day stay policy. The mean age of patients in the cohorts was 70.1 +/- 0.6, 70.0 +/- 0.8 and 70.5 +/- 0.7 years respectively, 70.2+/- 0.4yearsfor the whole cohort. Pre-operatively, in the whole cohort, the symptomatic patients had >70% stenosis 75patients had suffered an ipsilateral stroke, 123 patients had suffered an ipsilateral transient ischaemic attack (TIA) or amaurosis fugax. 203patients were asymptomatic but had critical stenosis of >60%. Risk factor data was only available for 364patients (86%), 231 patients had hypertension, 115 patients had hypercholesterolaemia, 73patients had diabetes mellitus. All patients were assessed by Duplex scan and MRI. Only symptomatic patients continued intravenous heparin infusion up until surgery. All patients received 5000IU bolus of heparin prior to carotid artery cross-clamping and all patients were monitored by EEG and a shunt was used only when there was ≥50% decrease in amplitude of the alpha or beta frequencies, or loss of all cerebral activity. The carotid arteriotomy was closed primarily except in 1patient who underwent re-operation, or 2patients who had previously received radiation to the neck. These latter 3patients had vein patch closure. All patients stayed in intensive care for 1night post-surgery. There was no link between LOS and major complications. The complications deemed were death, MI or stroke. Mean post-operative LOS for the whole cohort was 2.1 +/- 0.2days; Cohort 1, 2.6 +/- 0.3 days; Cohort 2, 2.3 +/- 0.4 days; Cohort 3, 1.6 +/- 0.1 days with a statistically significant difference between Cohorts 1 and 2 (p< 0.0001) and Cohort 1 and 3 (p< 0.0001). 2patients (0.48%) died peri-operatively following ipsilateral ischaemic strokes (one each in Cohort 1 and 3). 2patients (0.48%) suffered MI but discharged haemodynamically stable. 13patients (3.1%) suffered a stroke, including the 2patients who died (Cohort 1, 7 (4.1%); 2, 3 (3.2%); 3, 3 (2.0%)). 7patients (1.7%) underwent re-operation, 3 for exploration of operated vessel for contralateral hemiparesis or hemiplegia with angiographic evidence suggesting thrombus or significant intimal flap, 2 for acute evacuation of neck haematoma, 2 for delayed drainage of wound infection. 13patients had nerve injury, 9 patients had injury to the marginal mandibular nerve, 2 patients had injury to the hypoglossal nerve and 2patients had mild hoarseness caused either by endotracheal intubation or retraction injury. All nerve injuries resolved by 6weeks post-CEA. They achieved a statistically significant, 20% reduction in the use of routine laboratory investigations including full blood counts. The study noted an increase in next day discharge from 32% to 70%, once all stakeholders had become ‘emboldened’ that patients did not require further observation beyond 18-24hours post- CEA. Any complications would manifest within this time.
Other factors that delay discharge beyond day 1 post- CEA include female gender; history of angina, valve disease, heart failure and cerebrovascular disease (Hernandez)13. Roddy et al14 reviewed reasons for prolonged stay beyond their critical pathway aim of discharge on day 1 after CEA, in their cohort of 188patients, found that the mean post-operative LOS was 1.65+/- 0.08 and total LOS was 2.17 +/- 0.14 days. 57% of patients were discharged home as intended on the pathway, on day 1 post-CEA. Significant factors for prolonged stay were post-operative complications such as TIAs (1%), MIs (1%), neck haematomas requiring surgical drainage (2.7%), small haematomas requiring observation for an extra day (2.1%), age >79years, diabetes mellitus, female gender and intravenous vasodilator therapy requirement. Previous atherosclerotic risk factors, previous neurologic symptoms, use of vasopressor agents and re-operation had a lesser association. The post-operative mortality from stroke was 1.6%14.
Whilst very few patients have isolated risk factors, the effect of having multiple risk factors such as age above 80-years, congestive heart failure, COPD, renal failure, contralateral carotid artery occlusion, recurrent ipsilateral carotid artery stenosis, ipsilateral hemispheric symptoms within 6weeks and, coronary artery bypass grafting (CABG) within 6months in a retrospective review of 1370patients undergoing CEA between 1990 and 1999. 11 patients (0.8%) died; 6patients (0.4%) had disabling stroke and 10patients (0.7%) had non-disabling stroke. There was no statistical difference between outcome of death or stroke between patients with 1 or more risk factors (p=0.689) and no risk factors (p=0.681). The 20-day mortality was significantly greater in patients with 2or more risk factors compared to those without risk factors (2.8%, 0.3%p= 0.4). Only contralateral carotid artery occlusion was a significant predictor of adverse events (RR 4.3%, 95% CI 1.2-12.3; p=0.01) (Reed et al, 2003)15. Similarly, Halm et al16 found an adverse association between age above 80-years (OR 1.3, 95% CI 1.50-2.54), contralateral carotid artery stenosis ≥50% (OR 1.44, 95% CI 1.45- 1.79) and coronary artery disease (OR 1.51, 95% CI 1.20- 1.91).
An effort to comprehend the intra-operative factors that can lead to post-operative neurological deficit including stroke was noted in 63 of 2365patients operated on during the period 1965 to 1991, revealed there were more than 20different mechanisms that could be responsible. In 10 out of 66patients who had peri-operative stroke secondary to carotid artery injury related to clamping and de-clamping of whom 5patients had difficulty in placement of a shunt and 1patient becoming hypotensive whilst the shunt was in place, 1patient developed a bradycardia post-surgery thus reducing cerebral flow, the remaining patients suffered a stroke in the contralateral hemisphere likely secondary to a delay in shunt placement. Post-operative thrombus and embolism in 25patients in the immediate post-operative period, causing 9 out of15patients suffering a stroke whilst in the recovery area and 4 out of 15 patients having a stroke within 10hours of surgery, only 2 out of 15 patients had a stroke more than 24hours after surgery (6days and 14days later). All these patients had tolerated carotid artery clamping whilst under cervical block anaesthesia. Surgical exploration found technical defects leading to platelet aggregation such as clamp injuries, kinks in the redundant vessels, ledges at the end of the endarterectomy, stenosis at the closure of the arteriotomy and platelet aggregation on the synthetic patch material. The authors infer embolism as the cause of stroke in this group. In 10 out of 25patients labelled with delayed stroke secondary to embolic phenomena without thrombus present, they were managed conservatively. 8 out of 66patients had intracerebral haemorrhage having had a pre-operative stroke and, 4out 66aptients had transient ischaemic attacks (TIAs). 8out of 66 patients had a stroke not attributable to surgery or the reconstructed artery (Riles)17
Infra-inguinal Lower limb bypass
The in-hospital mortality in the UK, following lower limb bypass in 5387patient in 2014, were 2.7% (95% CI 2.3- 3.2). The registry noted 1 in 10 patients were re-admitted within 30-days of surgery but the reasons for this are unknown7. A series review of 4874patients over a 2year period, found the average LOS 7.5days. The independent risk factors for an arbitrarily defined protracted LOS of more than 8days were, distal bypass (OR 1.3, 95% CI 1.1-1.8); obesity (OR 1.3, 95% CI 1.1-1.5); partial functional dependence (OR 2.8, 95% CI 1.8- 2.4); history of cardiac disease (OR 1.5, 95% CI 1.1- 2.0); history of peripheral vascular interventions (OR 1.3, 95% CI 1.1- 1.5); bleeding disorders (OR 1.2, 95% CI 1.03- 1.4); emergency operation (OR 1.9, 95% CI 1.4- 2.7); age above 80-years (OR 1.45, 95% CI 1.3- 1.7); tissue loss (OR 1.9, 95% CI 1.6- 2.3); extended pre-operative hospital stay (OR 2.2, 95% CI 1.8- 2.6); renal dialysis (OR 1.6, 95% CI 1.3- 2.0)18. Prolonged LOS in the index admission is an independent risk factor for re-admission (p<0.0001). The increased LOS was a reflection of disease severity such as advanced peripheral arterial disease (PAD) and emergency department admission and occurrence of post-operative complications. Complications such as urinary tract infection, pneumonia, respiratory failure, congestive cardiac failure and more specifically, graft and wound infections, graft complications such as thrombus. 30-day re-admission was a reflection of underlying pathology such as advanced PAD, diabetes, chronic lung disease, renal failure, post-operative congestive cardiac failure and discharge to a rehabilitation type nursing facility19. A retrospective review of 6558 patients who underwent lower extremity bypass over a 3-year period found that the average LOS was statistically significantly shorter for those not re-admitted within 30-days, 5.5days compared to 8.3days for those were re-admitted within 30-days. 35% of the cohort were re-admitted within 30-days. The significant factors increasing LOS were increased disease severity and post-operative complications, emergency admission, advanced peripheral vascular disease (PVD), post-operative complications such as pneumonia, urinary tract infection, wound/graft infection, graft complications and if the patient was discharged to a nursing home i.e. not discharged to their own home. Factors that predicted 30-day re-admission were a reflection of the patients co-morbidities such as advanced PVD, diabetes, renal failure, chronic lung disease, post-operative heart failure and again, discharge to place other than their own home. Age was a protective factor for LOS but not for 30-day readmission20. A multi-centre review of LOS suggested a very weak link between increased LOS and 30-day re-admission after adjusting for age, gender, race, non-elective admission, co-morbidities, major post-operative complications and, discharge destination (Gonzalez)20.
Meyrs et al (2008)21 assessed the relationship between qualitative and quantitative measures of PVD. The disease was assessed by ankle-brachial pressure index (ABI) and in more detail on CT, MRI or invasive angiography. The claudication distance was assessed on a treadmill speed set at 0.67ms-1 (1.5mph) and at 10% gradient. The initial claudication distance was at the onset of claudication symptoms and the absolute claudication distance was the total distance walked before stopping due to pain. The walking speed was also assessed once patients had been familiarised with the use of the treadmill. The qualitative measures were carried out by using the validated, disease specific Walking Impairment Questionnaire (WIQ) that assesses pain, distance, walking and stair climbing, and, the Medical outcomes Study Short Form 36 (SF-36) Health Survey which assesses physical function, limitation due to physical health, limitation due to physical health, limitation due to emotional problems, energy, mental health, bodily pain, general health and social function. Control subjects were recruited on the basis their ABI was >0.9 such that there was a statistically significant difference between both groups for ABI. There were also statistically significant differences between the groups for their WIQ scores and on the SF-36, for physical function, physical limitations, bodily pain, social functioning and general health. The level of disease did not affect the outcomes on WIQ or SF-36. ABI had a significant correlation with the distance and speed components of WIQ but none of the components of SF-36 or the claudication distances. Yet claudication distance had significant correlation with many components of both WIQ and SF-36. Interestingly self-selected pace did not correlate with the qualitative measures. Ultimately, claudication distance, both initial and absolute, correlated with qualitative measures. Also, the WIQ was the reflection of actual ambulatory ability of patients with PAD.
An ERAS-type of critical pathway was proposed and assessed by Stanley et al (1998)22 for patients undergoing LEB. They acknowledged the heterogeneity of their patient cohort including emergency admissions and those patients transferred from other centres for vascular surgery input, similar to the model running in England and Wales currently. The model was based on a 5-day pathway and included many of the components of the current ERAS model such as removal of urethral catheter and encouragement of mobilisation on day 1 post-surgery. Crucially, the patient and family were educated about the pathway prior to elective surgery, as well as assessment of discharge needs with discharge planning commenced. The median LOS post-operatively in the post-pathway group was significantly reduced at median 6days (2-35) compared with 7days (2-29) pre-pathway (p=0.02). The anaesthetic route did not influence LOS in either pre- or post-pathway patients but the duration of epidural prolonged LOS. 55% of patients following the pathway were discharged to an intermediate care facility compared to 72% of pre- pathway patients were discharged directly home. The pathway did not affect the mortality and re-admission outcomes. Whilst age and body mass index (BMI) did not affect LOS, post-operative complication rates were increased in those with existing diabetes (30%) compared to those without diabetes (13%) and, those with cardiac disease (24%) compared to those without (15%). Patients with COPD, low pre-operative haematocrit or high pre-operative creatinine, also had prolonged LOS. Patients undergoing bypass for limb salvage had longer period of stay compared to those with claudication symptoms but also, the more distal anastomoses especially tibial vessels had longer hospital stay than more proximal anastomoses such as the popliteal artery. Again, those discharged to a facility other than their own home had a prolonged LOS. After adjustment, the independent factors associated with prolonged LOS were pre-operative anaemia, anastomosis to tibial vessels, pre-existing coronary artery disease and post-operative complications. Ultimately the pathway was not associated with a shorter LOS after adjusting for these factors. 8 of 69 pathway patients and 4 of 67 pre-pathway patients stayed beyond 14 days post-surgery. the reasons for their prolonged stay was existence of open ulcers necessitating debridement or amputation, suffering peri-operative MI, cardiac arrhythmia, ethanol withdrawal, respiratory failure caused by chronic pulmonary disease or large post-operative haematoma. Re-analysis of LOS after excluding the 12 patients with LOS greater than 14days, the only factor that was a predictor of longer LOS was diabetes. Another factor associated with increased length of stay and increased risk of post-operative wound complications is prolonged duration of bypass surgery. The duration of surgery was divided into quartiles of ≤149 minutes (6.3%), 150-192 minutes (9.0%), 193-248 minutes (10.1%) and, ≥249 minutes (13.9%) with p<0.01, a population of 2644 patients undergoing infra-inguinal bypass. The authors recognise there may be many confounders including system factors and surgeon factors involved but carrying out the operation in a reasonable time is an appropriate target to facilitate quality improvement (Tze-Woei)23.
Major lower limb amputation
Major lower limb amputation is indicated when revascularisation is no longer an option or amputation is expected to prolong life and even improve the patients quality of life7, 24- 25. A UK review of amputation data showed an average LOS of 32days (range, 7-67days). Early discharge planning is recommended but only 36.3% of vascular units had a dedicated vascular/ amputee discharge co-ordinator present. 25 Other aspects of planning for and managing patients pre- and post- amputation are assessment by a consultant vascular surgeon. 84% of trusts reported that all patients undergoing major amputations were preoperatively assessed by a consultant vascular surgeon. To facilitate discharge planning, 80% of vascular units reported patients were assessed by a rehabilitation physiotherapist, 61% reported patients were assessed by an occupational therapist and 25% reported preoperative assessments were available from a prosthetics service. 7
A review of Canadian data, 5342patients, 68% were male with a mean age of 67 +/- 13. The co-morbidities ranged from diabetes in 96%, hypertension in 33%, ischaemic heart disease in 18%, congestive cardiac failure in 10% and hyperlipidaemia in 5%. In 81% of admission, diabetic complications were commonest (81). Below knee amputation (BKA) was carried out in 65% of patients, followed by above knee amputation in 29%, the remainder having foot (4%), toe (1%) and ankle (1%) amputation. Factors statistically significantly associated with prolonged LOS, arbitrarily set at 7days were, amputation carried out by a general surgeon (OR 1.51, 95% CI 1.21- 1.87), an AKA (OR 0.71, 95% CI 0.61- 0.83), hypertension (OR 1.34, 95% CI 1.13- 1.58), ischaemic heart disease (OR 1.54, 95% CI 1.24- 1.91), congestive cardiac failure (OR 2.60, 95% CI 1.86- 2.63) and re-amputation (OR 10.50, 95% CI 5.16- 21.35) within index admission. In-patient mortality was 9%. 65% of patients were discharged to a rehabilitation nursing facility and only 27% discharged home. Part of the explanation why those operated upon by a general surgeon is that the teams and possibly the hospitals where the surgery was carried out did not have the infrastructure set up for steering a complex discharge26.
Results
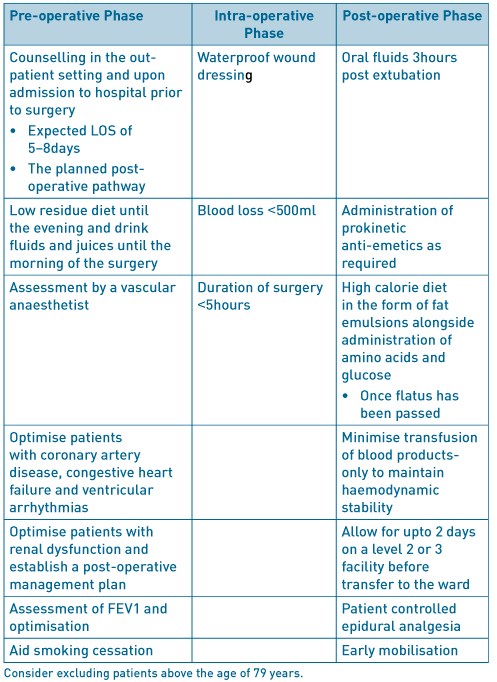
Open repair of AAA
Table 1. ERAS factors to consider in open AAA.
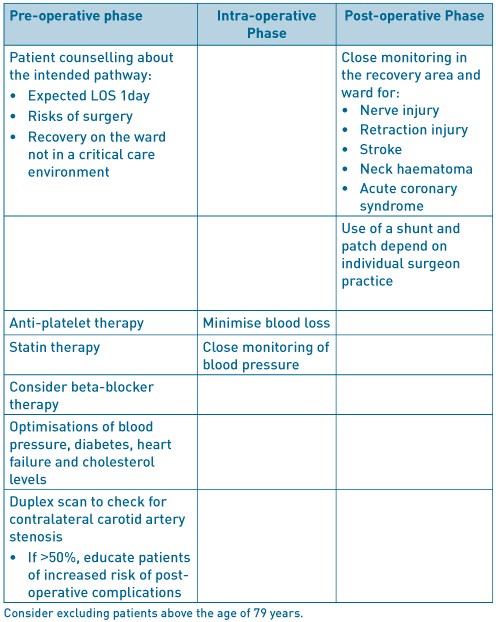
Carotid endarterectomy
Table 2. ERAS factors to consider in carotid endarterectomy.
Infra-inguinal lower limb bypass
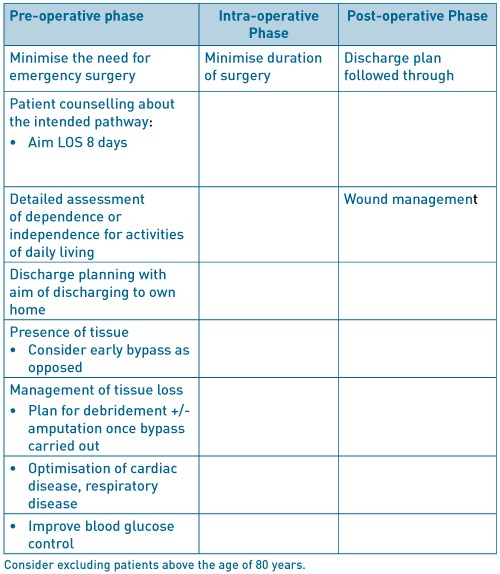
Table 3. ERAS factors to consider in infra-inguinal lower limb bypass
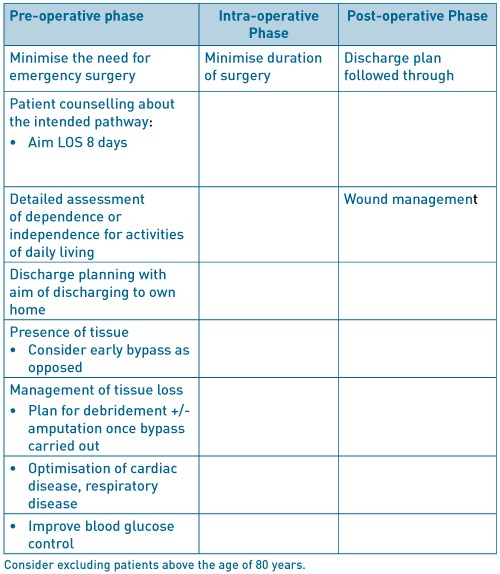
Major lower limb amputation
Table 4. ERAS factors to consider in major lower limb amputation.
As can be seen Tables 1-4 above, there are common themes present in all the major vascular surgery interventions. Primarily, optimisation of the major co-morbidities and pre-operative assessment by an anaesthetist specialising in vascular surgery. Cardio-pulmonary exercise testing is now widely being used in the assessment of patients prior to elective vascular surgery7. Also, factors such as smoking cessation therapy introduced 4-6weeks prior to surgery has been shown to reduce post-operative cardiac complications and LOS. Initial reduction of lung secretions and improving lung function can be augmented by an exercise program. The use of statins commenced 30-days prior to surgery and continued indefinitely, improve cardiac morbidity and mortality. The use of beta-blocker agents particularly bisoprolol, commenced 30-days prior to surgery, in patients with the highest and intermediate cardiovascular risk27.
Conclusions
Although ERAS in its current form may not be applicable to non-cardiac vascular surgery, with modifications for the different types of surgery, it can be seen to be useful to not only reduce length of stay but improve patient progress and well- being. In-depth assessment is required for each major intervention.
References
- Kehlet H. Multimodal approach to postoperative recovery. Curr Opin Crit Care 2009;15:355-358.
- Kehlet H. Enhanced Recovery After Surgery (ERAS): good for now, but what about the future? Can J Anesth 2015;62:99-104.
- Tatsuishi W, Kohri T, Kodera K, Asano R, Kataoka G, Kubota S, Nakano K. Usefulness of an enhanced recovery after surgery protocol for perioperative management following open repair of an abdominal aortic aneurysm. Surg Today 2012;42:1195-1200.
- UK Small Aneurysm Trial Participants. Length of Hospital Stay following Elective Abdominal Aortic Aneurysm Repair. Eur J Vasc Endovasc Surg 1998;16:185-191.
- Chang JK, Calligro KD, Lombardi JP, Dougherty MJ. Factors that predict prolonged length of stay after aortic surgery. J Vasc Surg 2003;38:335-339.
- Huber TS, Wang JG, Derrow AE, Dame DA, Ozaki CK, Zelenock GB, Flynn TC, Seeger JM. Experience in the United States with intact abdominal aortic aneurysm repair. J Vasc Surg 2001;33:304-311.
- Waton S, Johal A, Heikkila K, Cromwell D, Loftus National Vascular Registry: 2015 Annual Report. London: The Royal College of Surgeons of England, November 2015.
- Muehling B, Schelzig H, Steffen P, Meierhenrich R, Sunder-Plassmann L, Orend KH. A prospective randomized trial comparing traditional and fast-track patient care in elective open infra-renal aneurysm repair. World J Surg 2009;33(3):577-585.
- Gurgel SJT, Dib R El, Nascimento P Do. Enhanced Recovery after Elective open Surgical Repair of Abdominal Aortic Aneurysm: A Complementary Overview through a Poole Analysis of Proportions from Case Series Studies. PLoS ONE 9(6): e98006. doi:10.1371/journal.pone.009800.
- National Institute for Health and Care Excellence. Transient Ischaemic Attack Pathway https://pathways.nice.org.uk/pathways/stroke/transient-ischaemic-attack#content=view-node%3Anodes-assessing-and-managing-carotid-stenosis accessed 15/07/2016.
- Sheehan MK, Baker WH, Litgooy FN, Mansour A, Kang SS. Timing of postcarotid complications; A guide to safe discharge planning. J Vasc Surg 2001;34:13-16.
- Angevine PD, Choudri TF, Huang J, Quest DO, Solomon RA, Mohr JP, Heyer EJ, Connolly S. Significant Reductions in Length of Stay After Carotid Endarterectomy Can Be Safely Accomplished Without Modifying Either Anaesthetic Technique or Postoperative ICU Monitoring. Stroke 1999;30:2341-2346.
- Hernandez N, Salles- Cunha SX, Daoud YA, Dosick SM, Whalen RC, Pigott JP, Siewert AJ, Russell TE, Beebe HG. Factors related to short length of stay after carotid endarterectomy. Vasc Endovascular Surg 2002;36(6):425-437
- Roddy SP, Estes JM, Kwoun MO, O’Donnell TF, Mackey WC. Factors predicting prolonged length of stay after carotid endarterectomy. J Vasc Surg 2000;32:550-554.
- Reed AB, Gaccione P, Belkin M, Donaldson MC, Mannick JA, Whittemore AD, Conte MS. Preoperative risk factors for carotid endarterectomy: Defining the patient at high risk. J Vasc Surg 2003;37:1191-1199.
- Halm EA, Tuhrim S, Wang JJ, Rockman C, Riles TS, Chassin MR. Risk Factors for Perioperative Death and Stroke After Carotid Endarterectomy. Stroke 2009;40:221-229.
- Riles TS, Imparato AM, Jacobwitz GR, Lamparello PJ, Gianglo G, Adelman MA, Landis R. The cause of perioperative stroke after carotid endarterectomy. J Vasc Surg 1994;19:206-216.
- Siracuse JJ, Jones DW, Gill HL, Graham A, Schneider DB, bush HL, Karwowski Connolly PH, Meltzer AJ. Lower Extremity Bypass for Critical Limb Ischaemia- Predicting Extended Length of Stay. J Vasc Surg 2013;58(4):1151.
- Damrauer SM, Gaffey AC, Smith DeBord, Fairman RM, Nguyen LL. Comparison of risk factors for length of stay and readmission following lower limb bypass surgery. J Vasc Surg 2015;62(5):1192-1200.
- Gonzalez AA, Mell MW, Osborne NH. Reducing Length of Stay Is Not Associated With Increased Readmission Rates Following Lower Extremity Arterial Bypass. J Vasc Surg 2015;61(6):189S.
- Meyers SA, Johanning JM, Stergion N, Lynch TG, Longo GM, Pipnos II. Claudication distance and the Walking Impairment Questionnaire best describe the ambulatory limitations in patients with symptomatic peripheral arterial disease. J Vasc Surg 2008;47:550-550.
- Stanley AC, Barry M, Scott TE, LaMorte WW, Woodson J, O.Menzoian J. Impact of a critical pathway on postoperative length of stay and outcomes after infrainguinal bypass. J Vasc Surg 1998;27:1056-65.
- Tze-Woei T, Kalish JA, Hamburg NM. Shorter Duration of Femoral-Popliteal Bypass Is Associated With decreased Surgical Site Infection and Shorter Hospital Stay. J Am Coll Surg 2012;215:512-518.
- The Vascular Society of Great Britain and Ireland. Quality improvement framework for major amputation surgery. 2010. Vascular Society of Great Britain and Ireland. http://www.vascularsociety.org. uk/news-and-press/2010/47-quality-improvementframework-for-major-amputation-surgery-.html
- National Confidential Enquiry into Patient Outcomes and Deaths. Lower Limb Amputation: Working Together 2014. London: NCEPOD, 2014.
- Kayssi A, de Mestrel C, Forbes TL, Roche- Nagle G. A Canadian population-based description of the indications for lower-extremity amputations and outcomes. Can J Surg 2016;59(2):99-106.
- Moll FL, Powell JT, Fraedrich G, Verzini F, Haulon S, Waltham M, van Herwaarden JA, Holt PJE, van Keulen JW, Ranter B, Schlosser FJV, Setacci F, Ricco JB. Management of Abdominal Aortic Aneurysms Clinical Practice Guidelines of the European Society for Vascular Surgery. Eur J Vasc Endovasc Surg 2011; 41:S1-S58.
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2017-journal/jods-274-2017/enhanced-recovery-in-major-vascular-surgery/
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6177/274-dhillon.pdf