The increasing challenge of managing morbidly obese patients with gallstone disease in a non-bariatric centre (1) « Contents
Sian Davies, Ghaleb Goussous, Amaar Aamery, Aliyah Choudray & Mangta Manu
Royal Wolverhampton NHS Trust
Conflicts of Interest Statement
We can confirm that we have no conflicts of interest to disclose.
Abstract
Background: An important risk factor for gallstone disease is obesity which poses a significant problem for surgical management. The aim of our study was to show that laparoscopic cholecystectomy is still safe to be performed as a day case or short stay procedure (<24hrs) in the obese and morbidly obese patient in a non-bariatric center.
Method: A retrospective observational study analysing all patients who underwent laparoscopic cholecystectomy at Royal Wolverhampton Hospital between January 2013 and January 2017 was performed. Patients were identified using RWH HES data and Length of stay, operative duration, and readmission rates were compared for BMI categories. Statistical analysis was performed by Chi-square test and one-way Anova test as appropriate. A p-value of <0.05 was considered significant.
Results: We identified 1055 cases. Male to female ratio was approximately 1:3. There was no significant difference between the primary outcomes of length of stay, Number performed as day case, operative duration and 30-day readmission rates between all BMI groups. In all groups the number of cases being performed as day case with same day discharge was 70-78% with no significant difference between the groups. The mean operative duration for the highest BMI group (BMI>41) of 59.78 mins compared to the lower BMI groups (BMI 26-30) of 55.25 mins this was not significantly different. 30-day readmission rates for all BMI groups were comparable (P = 0.61).
Conclusion: Our results highlight that obese (BMI 35-39) and morbidly obese (BMI >40) patients can have a laparoscopic cholecystectomy performed safely in a non-bariatric center and as day case/short stay procedure (discharge within <24hrs) with no significant increase to operative duration, LOS or 30-day readmissions rates.
Introduction
Laparoscopic cholecystectomy is one of the most common elective operations in the UK with over 60,000 cases performed each year (1). It is associated with a very low morbidity and mortality and often performed as a day case procedure in most centres with a very low risk of conversion to an open procedure. The main indication for performing this procedure is cholelithiasis which has a UK population incidence of 10-15%. An important risk factor for gallstone disease is obesity (2) and with an obesity crisis in the UK this presents a significant problem for surgical management. Currently 1 in 4 people in the UK are obese (BMI >30 (28.1%)) with 1 in 10 being morbidly obese (BMI>40 (2.9%)) (3). These are set to rise over the next 10 years and its predicted that more than a 3rd of the UK population will be obese by 2020 (4).
Obese and morbidly obese patients post a significant challenge both anesthetically (5) and surgically with some studies suggesting increased operative times and increased LOS, and previously there has been a hesitancy to offer these patients a laparoscopic cholecystectomy in a non-bariatric center (6). However increasing evidence has shown that laparoscopic cholecystectomy is safe even in the morbidly obese patient and have also suggested that they can also be performed as a day case safely (7) (8) (9). The aim of our study was to show that laparoscopic cholecystectomy is still safe to be performed as a day case or short stay procedure (<24hrs) in the obese and morbidly obese patient in a non-bariatric center.
Methods
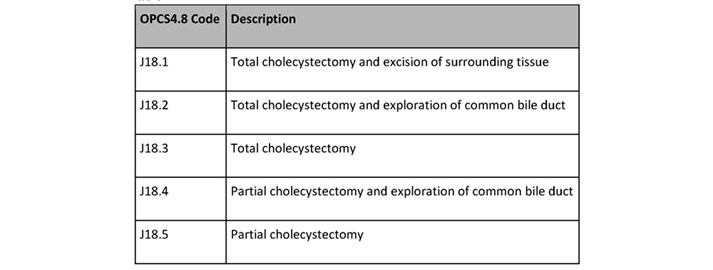
A retrospective observational study was performed analyzing all patients who underwent laparoscopic cholecystectomy at Royal Wolverhampton Hospital between January 2013 and January 2017. Patients were identified using the Royal Wolverhampton Hospital HES (Hospital episode Statistics) data coded for elective laparoscopic cholecystectomy using the OPCS4.8 codes for cholecystectomy (table 1)
Table 1.
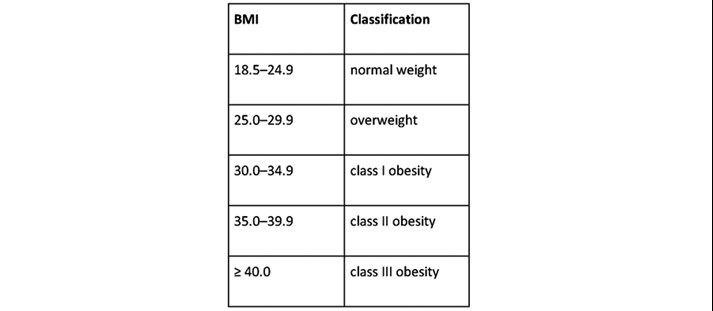
Patients were divided into individual BMI groups based on WHO anthropometry guidance on obesity classification (Table 2).
Table 2.
Primary outcomes include length of stay and operative duration were compared for BMI categories. Secondary outcomes were post-operative morbidity rates, conversion to an open procedure and readmission rates. Post-operative 30-day morbidity was classified using the Clavien-Dindo classification. Patients with a prolonged LOS (>24hrs) had their notes and discharge letters assessed and complications classified.
Exclusion criteria included those admitted as emergencies and non-standard laparoscopic cholecystectomy (single incision laparoscopic surgery, and those patients who had previous surgery and an adaptive approach was used). Statistical analysis was performed using GraphPad Prism software V7 (GraphPad Software Inc). Statistical analysis was performed by Chi-square test and one-way Anova test as appropriate. A p-value of <0.05 was considered significant.
Results
A total of 1055 cases were identified that met our inclusion and exclusion criteria. Male to female ratio was approximately 1:3 (803 females, 252 males). In the higher BMI groups, there was a significantly higher ratio of females of males (p= <0.0001) and the higher BMI groups were generally younger patients as demonstrated in table 1.
Operative and Post-operative results are shown in Table 2. There was no significant difference between the primary outcomes of length of stay (LOS), Number performed as day case, operative duration and 30-day readmission rates between all BMI groups. In all groups the number of cases being performed as day case with same day discharge was 70-78% with no significant difference between the groups. The mean operative duration for the highest BMI group (BMI>41) of 59.78 mins compared to the lower BMI groups (BMI 26-30) of 55.25 mins this was not significantly different.
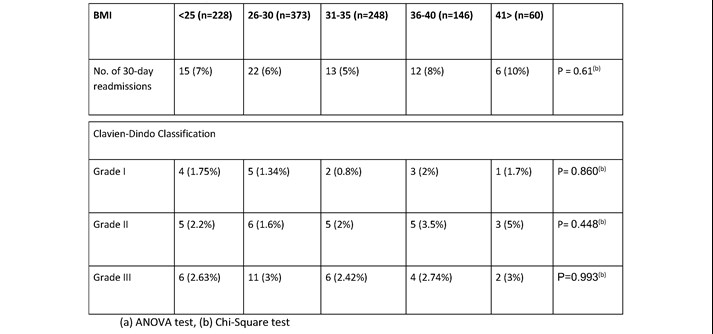
When analysis was performed looking at the reasons for prolonged stay (>24hrs) using the Clavian-Dindo classification there was no significant difference in complications. The most common reason for prolonged stay was post-operative pain (1.9%), and urinary retention (0.6%). Other more clinically significant complications included post-operative bleeding (1.3%) and bile duct injury (table 3). 30-day readmission rates for all BMI groups were comparable (P = 0.61). On specific analysis of the reasons for readmission these were again also comparable across the groups with the majority of readmissions for wound infections (1.2%) and missed or retained stones (0.8%) (table 4).
Table 1. Patient Demographics for BMI categories.
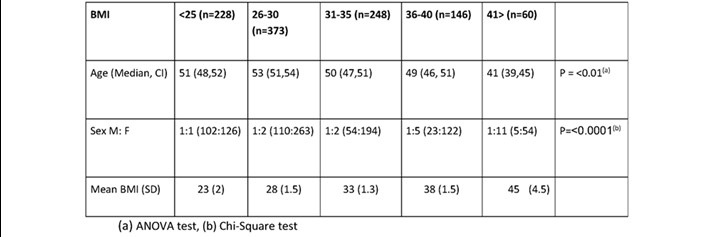
(a) ANOVA test, (b) Chi-Square test
Table 2. Operative and Post-operative results for BMI categories.
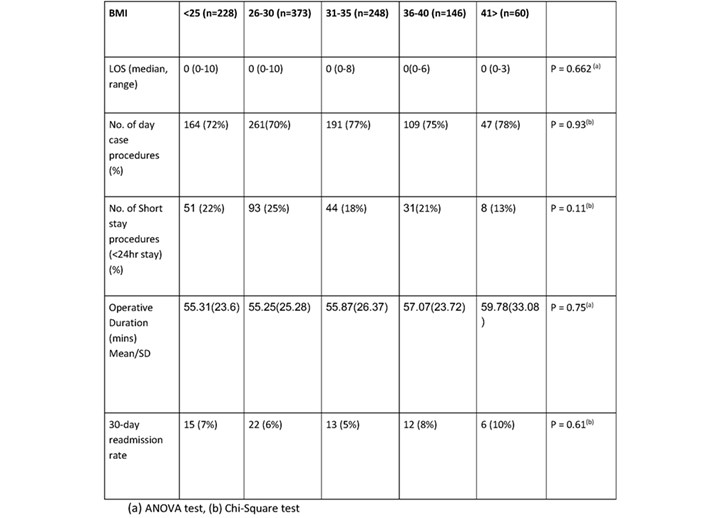
Table 3. Post-operative complications resulting in length of stay >24hrs.
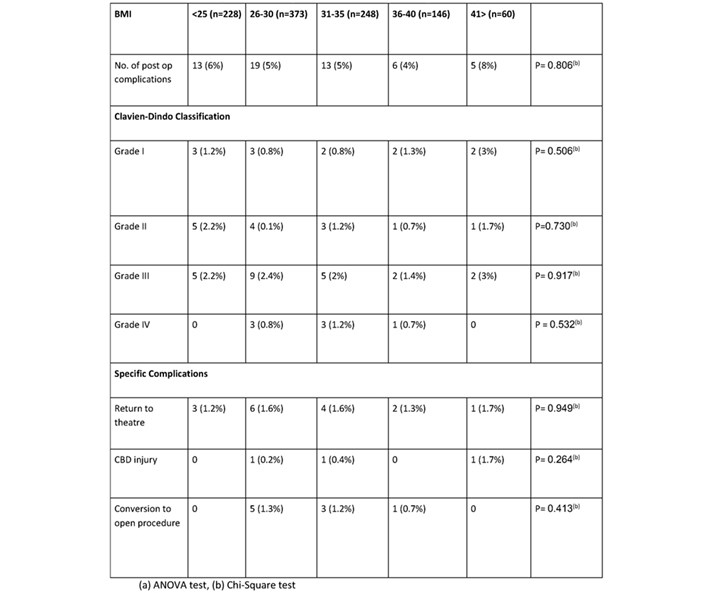
Table 4. 30-day Readmission related to operative complications.
Discussion
Increasing evidence has shown that laparoscopic cholecystectomy is safe in the obese patient and our large cohort study builds on this data by showing no significant difference in length of stay, 30 day rea30-dayon rates, post-operative complications or operative duration between BMI groups for patients undergoing laparoscopic cholecystectomy in a no bariatric center. We have also shown that these potentially higher risk groups of patients can still have their procedures performed as day case without any serious risk of complication which is highlighted by the lack of difference in 30-day readmission rates. The fears of operating on the group maybe allayed when data from study shows that the higher BMI group tend to be a younger cohort of patients (median 41 (Class III obesity), median age 51 (normal weight)) and higher female prevalence, in whom fat distribution tends to be subcutaneous rather than internally (9). There was a small difference in operative duration between the normal weight patients and the class III obese patients (mean = 55.31 vs. mean = 59.78, p=0.75) this was not significant. There is an appreciation that this increase can be accumulative during a list, but overall difference would still be marginal, and this could be taken into account during list design. There was also no difference in the rate of conversion to an open procedure between the BMI groups.
With higher national tariff payments for day case procedures and no significant increase risk of post-operative complications, or 30-day readmission rates, these higher BMI groups should still be considered for day case management wherever possible even in a non-bariatric centre. Not offering these higher group patients a cholecystectomy put this group at a higher risk of the complications of gallstones disease particularly in gallstones pancreatitis. Studies have shown that obese patients are at higher risk of necrosis and complications of pancreatitis and is proportional to their BMI (10) (11) (12).
Operating on the obese and morbidly obese patient is a growing issue globally and our practice needs to adapt to account for this. Our study has shown that it is safe to offer a laparoscopic cholecystectomy to the obese (class I to III) patient as a day case in a non-bariatric centre and BMI should not be a limiting factor. We recognize limitations of this study include a retrospective methodology using HES Data which relies on accurate data entry and coding which in recent years has improved. Also, we did not include seniority of surgeon which may be a confounding factor in shorter operative duration, and this could be an area for future research.
References
- NICE and RCS of England. [Online] Dec 2016. Commissioning guide: Gallstone disease. https://www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=10&ved= 2ahUKEwi0nJyQwe3hAhWXRxUIHeHFB9oQFjAJegQIAhAC&url=https%3A%2F%2Fwww.rcseng.ac.uk%2F-%2Fmedia%2Ffiles.
- Epidemiology of gallbladder disease: cholelithiasis and cancer. Stinton LM, Shaffer EA. 2, 2012, Gut Liver, Vol. 6, pp. 172-187.
- Baker, Carl. Obesity Statistics. s.l. : House of Commons Library, 2018.
- Morbid obesity in the UK: A modelling projection study to 2035. Keaver L, Xu B, Jaccard A, Webber L. 2018, Scand J Public Health.
- Anaesthesia and morbid obesity. Sharmeen Lotia, Mark C. Bellamy,. 5, 2008, Continuing Education in Anaesthesia Critical Care & Pain, Vol. 8, pp. 151-156.
- Laparoscopic cholecystectomy in morbidly obese patients. Ammori BJ1, Vezakis A, Davides D, Martin IG, Larvin M, McMahon MJ. 11, 2001, Surg Endosc, Vol. 15, pp. 1336-9.
- Obesity: an indication rather than contraindication to laparoscopic cholecystectomy. Unger WS, Unger MH, Edelman SD et al. 1992, Obes Surg, Vol. 2, pp. 29-31.
- Day case laparoscopic cholecystectomy in patients with high BMI: Experience from a UK centre. A Tandon, G Sunderland, QM Nunes, N Misra1, M Shrotri. 2016, Ann R Coll Surg Engl, Vol. 98, pp. 329–333.
- Sex differences in human adipose tissues - the biology of pear shape. Karastergiou K, Smith SR, Greenberg AS, Fried SK. 1, s.l. : Biol Sex Differ, 2012, Vol. 3, p. 13.
- Obesity and pancreatitis. Khatua B, El-Kurdi B, Singh VP. 5, s.l. : Curr Opin Gastroenterol, 2017, Vol. 33, pp. 374-382.
- Obesity-Related Effects on Pancreatic Disease . Zyromski, Nicholas J. s.l. : Pancreapedia: Exocrine Pancreas Knowledge Base, 2015.
- Combination of APACHE-II score and an obesity score (APACHE-O) for the prediction of severe acute pancreatitis. Johnson CD1, Toh SK, Campbell MJ. 1, s.l. : Pancreatology, 2004, Vol. 4, pp. 1-6.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/42062/303-the-increasing-challenge-of-managing-morbidly-obese-patients-with-gallstone-disease-in-a-non-bariatric-centre.pdf