Improving Day Case Mastectomy Rate: A UK Hospital Experience « Contents
Shazia M Khan, Specialist Registrar in Surgery,1 Mahmoud Bakr, Medical Student, 1,2 Iman A Azmy, Consultant Oncoplastic Breast Surgeon, 1 Ciaran J Hollywood, Consultant Oncoplastic Breast Surgeon, 1 Amar Jawad, Consultant Anaesthetist, 1 Julia C Massey, Consultant Oncoplastic Breast Surgeon1
1 Chesterfield Royal Hospital NHS Foundation Trust . 2 The Medical School, University of Sheffield
Corresponding author: Shazia M Khan
Keywords: Day case, mastectomy, service improvement, audit loop
Declaration
There was no funding required for this project.
The authors have no affiliations that could be perceived as posing a potential conflict of interest in the publication of this article.
Abstract
Introduction: The 2016 BADS target for day case mastectomies was 30% (1). At Chesterfield Royal Hospital we achieved 25% (2). To improve this we conducted an audit to document our day case mastectomy rates, determine causes for inpatient stay and identify modifiable factors.
Method: All mastectomies performed in our unit over a 4 month period were included. Factors influencing admission were: carer presence post-operatively, distance from hospital, co-morbidities, type of surgery, surgical drain use, regional block, opioid use. Recommendations regarding modifiable factors were used to implement change. The audit was repeated one year later.
Results: In 2016, 10 out of 26 patients were planned day cases. 2 became unplanned admissions; making our actual day case mastectomy rate 31% (8/26). Modifiable factors influencing planned inpatient rates were identified: inaccurate allocation of patients’ hospital episode to the “planned admissions” group leading to coding errors (3/16), reason for inpatient planning not clearly documented (8/16), ANC (4/16) and bilateral mastectomy (2/16), use of drains in ANC (4/16). In 2017, 10 out of 19 patients were planned day cases. One became an unplanned admission; making our 2017 day case mastectomy rate 47%
Conclusions: The initial audit highlighted the need for: more robust documentation of reasons for inpatient admission planning, recognising that ANC and bilateral mastectomies alone shouldn’t necessitate admission, reviewing our use of drains in ANC & further promotion of our existing outpatient drain removal pathway in the minority that receive a drain. On re-auditing we saw an improved day case mastectomy rate from 31% to 47% following the implementation of the recommendations of the initial audit.
Introduction
Breast cancer is the commonest cancer in women in England & Wales with an annual incidence of 55,222 (3). 74% of breast cancer patients receive a surgical resection as part of their cancer treatment (4) and the majority of these patients undergo surgery as their first procedure.
Historically, patients undergoing breast cancer surgery required up to 6 days’ inpatient stay. Recognising the need for efficiency savings to be made in an era of diminishing available resources to serve the increasing demands placed on the National Health Service, the Department of Health in 2002 launched its “Day Surgery Strategy” with an aim of achieving 75% of all elective surgery in the UK to be performed on a day case basis by the year 2005. (5) Over the past 2 decades advancements in surgical and anaesthetic techniques have continued to improve and facilitate the national drive towards day case breast surgery. (6) An expansion of the age, ASA, and BMI eligibility criteria for day surgery procedures recommended in the in 2011 British Association of Day Surgery guidelines (7), in recognition of the national trends towards an aging population and rising levels of obesity, has enabled an even greater proportion of our patients to be considered as potential day case candidates.
Mastectomies are ideal procedures for day case surgery due to their significantly lower rates of post-operative events including pain, nausea & vomiting, venous thromboembolism and the greater feasibility of early mobilisation. (8,9) Patients report greater convenience in their own home environment with better recovery (9), while providers benefit from reduced hospital bed occupancy rates, reduced length of hospital stay (10) and hence reduced rates of hospital acquired infections; making this a financially sound option too.
In 2012 the “Quality & Productivity Case Study” published by NHS Improvement reported a 50% reduction in length of stay, release of 61,000 bed-day capacity and potential saving of £10.5 million if day case breast cancer surgery was rolled out nationally. (10) At Chesterfield Royal Hospital we estimated a potential saving of £5686 over the period April to July 2016 by moving from our recorded current practice to all day case mastectomies.
The day case procedure Best Practice Tariff (BPT) is a financial incentive for providers which aims to increase the proportion of elective activity performed as a day case, where clinically appropriate. The British Association of Day Surgery publishes a directory of procedures suitable for day-case admissions along with rates that they believe are achievable in most cases. Selection of procedures for day case BPT is based on the BADS directory. These are high volume procedures and have day case rates that vary significantly between providers and with achievement nationally that is below the BADS rates. In 2016 the BADS target for day case mastectomy was 30% (1). At Chesterfield Royal Hospital our published day case rate was only 25% (2). To identify ways in which we could improve our service, we conducted an initial audit to address this. The aims were to:
- document our day case and inpatient mastectomy rates
- determine causes for inpatient stay
- identify any modifiable factors to improve day case rate
- identify any coding errors impacting on our published day case rate
- identify achievable changes to our service that we can implement and re-audit
Methods
We conducted a retrospective initial audit of our service over a 4 month period in 2016, comparing this to nationally recommended day case rates for breast surgery. All patients having mastectomies with or without any form of axillary surgery and without immediate breast reconstructions between April and July 2016 were included. Patients were identified from the Service Improvement Lead & checked against consultants’ theatre diaries. Patients were excluded if their case notes were not available. A list of potential modifiable factors that would influence our day case activity was complied. Pre-operative factors in this list included co-morbidities, type of breast & axillary surgery (unilateral versus bilateral mastectomy and sentinel node biopsy versus axillary node clearance), distance from hospital, and availability of responsible adult at home for the first 24 hours post-operatively. Peri-operative factors included use of regional anaesthetic blocks, opioid analgesia & antiemetic use peri-operatively and use of surgical drains.
The audit was repeated for the same time period in 2017 following implementation of changes recommend by the 2016 audit.
Results
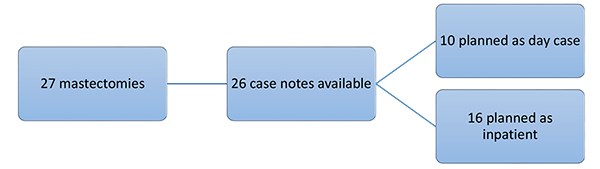
27 patients had mastectomies during the initial study period in 2016. 1 patient was excluded as her case notes were unavailable. Of the 26 cases studied, 10 were planned as day case. See figure 1.
Figure 1. Number of patients planned as inpatient and day case over four months in 2016.
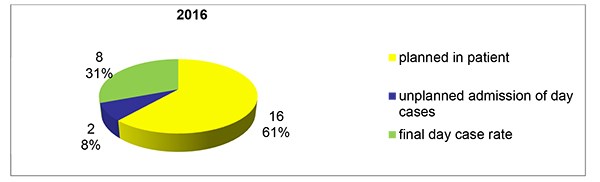
3 patients had been incorrectly coded as having planned inpatient stay post-operatively when in fact they had day surgery procedures. This increased our number planned as day case to 10. However, 2 out of these 10 patients ultimately required unplanned admission. One was due to PONV despite the patient having a regional block and anti-emetics with morphine. The other unplanned admission was due to low oxygen saturations post operatively in an asthmatic patient.
Thus we achieved a final day case rate for this period of 31% (8/26) once coding inaccuracies were removed, figure 2.
Figure 2. Mastectomies in the 4 Month Period 2016.
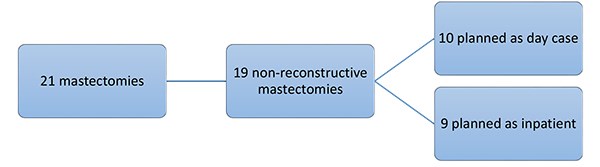
On re-auditing our practice over the April to July 4 month period in 2017 we found 21 patients had mastectomies. Two patients were excluded from further review as they had immediate breast reconstruction at the time of mastectomy. 10 of the remaining 19 patients were planned as day case (Figure 3)
Figure 3. Number of patients planned as inpatient and day case over four months in 2017.
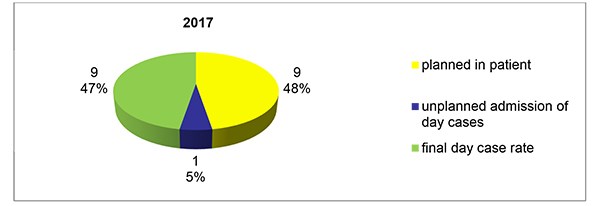
One of these 10 required an unplanned admission to hospital postoperatively due to having a persistently low respiration rate (<10 /min) post operatively. This patient was administered opiate analgesia intraoperatively. She was allowed home the following day when the opiate effect had worn off. Our final day case mastectomy rate was 47% (9/19) in the 2017 study period, Figure 4.
Figure 4. Mastectomies in the 4 Month Period 2017.
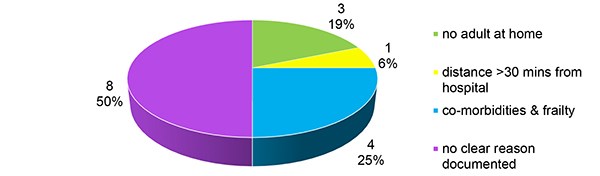
In 2016, 16 patients had a planned inpatient stay and reasons given for this are shown in Figure 5. The reason for inpatient stay was not clearly documented for 8 out of the 16 patients. On closer review, 4 of these patients had axillary node clearances with one patient having a surgical drain placed. 2 of the 8 had bilateral mastectomies. It was inferred that the types of surgery might have influenced the decision for inpatient stay; however, we routinely perform axillary node clearance as day case surgery. For the remaining 2 patients no potential reason for inpatient stay was identifiable.
Figure 5. Reasons Given for Planned Inpatient Stay 2016.
In the re-audit period we found 9 patients needed planned inpatient stay, the reasons for this are illustrated in Figure 6. An improvement in documentation of reasons for inpatient planning was noted by 2017, with 33% (3/9) of patients having no clear reason documented in 2017 compared to 50% (8/16) for 2016. Where no clear reason was identifiable in the 3 out of 9 patients in 2107; 2 had bilateral mastectomies and one had no potential reason identifiable for inpatient stay.
Figure 6. Reasons Given for Planned Inpatient Stay 2017.
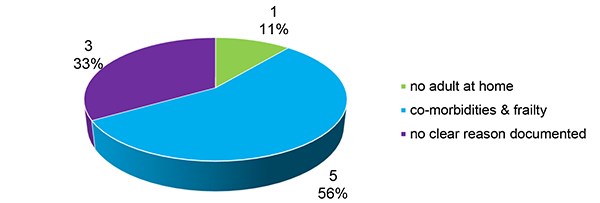
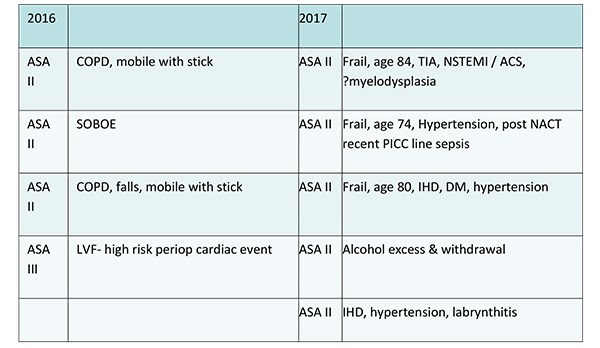
Table 1 details the reasons for planned inpatient stay for the patients who required admission due to co-morbidity & frailty.
Table 1. Co-morbidities necessitating planned admission.
Discussion
Historically there was a reluctance for early discharge home due to perceived gravity of cancer surgery and the need for specialist care post operatively. The clinician’s decision on whether to offer day case mastectomy to a patient in the modern era may be influenced by the availability of comprehensive oncoplastic services, patient motivation and the availability of robust out of hours’ services. To this end, a cornerstone to the success of modern day case breast surgery is the role of the specialist BCN in their peri-operative interactions with patients & carers to address their concerns and expectations regarding recovery at home, especially with drains in situ. (11) Recent studies with large patient cohorts have once again added to the wealth of available evidence confirming that whilst day case breast surgery has been shown to be safe, its success relies upon maximising close collaboration by all stakeholders including a well organised multi-professional team; at the same time as ensuring patients are reassured through education that the quality of their post-operative care will not be compromised by what they may have previously perceived as too early a discharge home. (12)
We have demonstrated here that in 2016 when coding errors are removed, over the period studied, Chesterfield Royal Hospital just achieved the target set by BADS for day case mastectomy.
When searching for ways to improve our day case mastectomy rate further we recognise some factors would be more readily modifiable than others.
It is difficult to improve on the unexpected events encountered leading to unplanned admission, despite perioperative optimisation as seen in the 2 out of 10 patients admitted in the 2016 group due to PONV despite use of regional block and anti-emetics, or low saturations in an asthmatic patient. In the 2017 group, only one patient had unplanned admission and this was due to persistently low respiration rate due to opiate effect. Our unit’s routine anaesthetic practice is to avoid perioperative opiate use and to administer a pectoral nerve block, where possible to avoid problems associated with opiate use. Without major input of increasingly fewer resources it is also difficult to improve the day case mastectomy rate in the case of the 8 patients out of 16 in 2016 who had either no carer, or lived a long distance from the hospital or had multiple significant co-morbidities.
However, an obvious area for improvement is in the 8 out of 16 patients’ group in the initial audit who had no clear documentation of indication for planned inpatient admission. Of these 4 had ANC (one of whom had a surgical drain inserted), 2 had bilateral mastectomies and for 2 patients it was inferred from the notes that the reason for planned admission was patient choice, though this was not clearly documented. Clear documentation of reasons for planned inpatient stay would also facilitate and improve consistency of admission planning across our unit.
Although there is no consensus on pre-assessment criteria, a patient’s choice, medical fitness, social support and requirement for immediate breast reconstruction are among the key factors for consideration when planning inpatient stay. (11,13) Whilst patient choice and non-availability of an adult carer post operatively are valid reasons for planned inpatient stay; in the modern perioperative care setting neither ANC (14) nor bilateral mastectomy alone mandate inpatient stay (13). In the United States the Healthcare Cost and Utilization Project (HCUP) data showed that between 2005 and 2013 the rate of bilateral mastectomies tripled. By 2013 whilst unilateral mastectomies were still commoner approximately one third of bilateral and half of unilateral mastectomies were performed in the outpatient setting. (15)
Although many units, ours included, have now dispensed with the routine placement of a surgical drain in cases of mastectomy alone without reconstruction; use of drains in ANC is variable. Mastectomy and ANC surgeries have been shown to have up to 91% seroma rate when no drain is used versus 85% with a drain. (16) Other studies have shown that whilst there may be some reduction in seroma rates with the use of axillary drainage (17), infection rates (17) and the overall duration of seroma fluid accumulation remains unaltered (18). Axillary drain placement is associated with a longer hospital stay. (17,19) Outpatient drain removal services are useful in preventing inpatient stay purely for drain management in instances where one is used. Discharge with drain in situ has long been shown to be a safe and cost effective strategy with high rates of patient satisfaction reported when supported by well-co-ordinated inpatient and outpatient services. (20,21,22) We note that utilisation of our unit’s outpatient drain removal pathway needs to be improved and flow through this is likely to be increased with further staff education and engagement. (23) Clinical pathways have been shown to be good educational tools; particularly for new staff, nurses and allied health professionals. (24,25) Revisiting our own local outpatient drain removal pathway at points of staff changeover and induction may maximise its effective implementation.
Better utilisation of our outpatient drain removal pathway may also improve overall patient flow through the hospital. Unit based pathways have been shown to not only impacts on the micro system of service provision in a single unit and its day case rates, for example, but also to affect, indirectly, the macro system of the hospital as a whole; not least by streamlining bed occupancy rates to ensure bed availability for those patients where admission is necessary. (26)
Our main focus in this study was to look at ways of improving our day case mastectomy rate by identifying modifiable factors in the pre-operative planning phase. We did not set out to review readmission rates as part of this study. Although very valuable to establishing the success of a day case mastectomy service; this separate line of enquiry may be considered the subject of a subsequent study. We recognise that this study represents a very small cohort of patients and the results of the achieved day case rates comparing 2016 & 2017 lack statistical significance (χ2 analysis p value > 0.05). However, it highlights key areas for improvement in the service we provide to our patients. We need robust documentation of and consistency in admission planning for different types of surgery as ANC and bilateral mastectomies alone do not necessitate inpatient stay. Studies have shown that patient flow can be optimised by addressing organisational boundaries at various points along the patients’ care journey. (26) Therefore, whilst we looked at ways of maximising ward staff awareness of our outpatient drain removal pathway, we also reviewed our use of drains in ANC. The outpatient drain removal pathway was then used in the minority that require a drain post ANC.
We liaised with the clinical coding department to minimise future costly coding inaccuracies. We re-audited our practice and by placing patient safety and satisfaction as well as staff education at the core of team practice, following implementation of the changes recommended by the initial audit we were able to improve our performance.
The findings of our initial audit were disseminated locally and presented at the BADS annual meeting 2017. Change was implement based on the recommendations regarding the identified modifiable variables. The audit was repeated one year later to assess the effect of these implementations.
In completing the audit loop in 2017 over the same 4 month period, we demonstrated a marked improvement in the day case mastectomy rate at Chesterfield Royal Hospital from 31% to 47%. As a team indoctrinating the philosophy that day surgery is the default position for non-reconstructive mastectomy with or without axillary surgery into our practice and promoting this to our patients our documentation of the reasons for planning inpatient stay has also improved from 50% to 66%. In the patients without any clearly discernible reason for inpatient planning in both the audits a possible explanation may have been simply patient choice, though this needs documenting.
We plan to continue to seek out further areas of development in an effort to increase our day case mastectomy rate further.
References
- British Association of Day Surgery. (2016). BADS Directory of Procedures. 5th Edition. BADS, London.
- Productivity.nhs.uk. (2017). Better Care, Better Values. [online] Available at: http://productivity.nhs.uk/PCT_Dashboard/DetailedView? practiceCode=RFS&pctCode=Q55&percentileId=2 &yearQtrId=29&indicatorId=609&indicatorTypeId=1&component Name=Simple%20mastectomy%20(with%20and%20w ithout%20axillary%20surgery)&treatment=selected&componentId=3004#performance [Accessed 31/03/2017
- Cancer Research UK (2017]), Breast Cancer Statistics, Cancer Research UK. [On line] Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer [accessed 31/ March 2017
- National Cancer Intelligence Network and Cancer Research UK. Major resections by cancer site, in England; 2006 to 2010 workbook (Version 2.0 - reissued June 2015) (link is external). London: NCIN; 2015.
- Department of Health: In Day Surgery: Operational Guide. 2002, Department of Health, London.
- Kopp, S. L. and Horlocker, T. T. (2010), Regional anaesthesia in day-stay and short-stay surgery. Anaesthesia, 65: 84–96. doi:10.1111/j.1365-2044.2009.06204.x
- Verma R, Alladi R, Jackson I, Johnston I, Kumar C, Page R, Smith I, Stocker M, Tickner C, Williams S and Young R: Day Surgery and short stay Surgery: 2. Anaesthesia. 66,2011, 417-434
- Jeevan R, Cromwell D, Browne J, et al. National Mastectomy and Breast Reconstruction Audit 2010. Third Annual Report, vol. IC28050110, 2010.
- Canet J, Raeder J, Rasmussen LS, Enlund M, Kuipers HM, Hanning CD, Jolles J, Korttila K, Siersma VD, Dodds C, Abildstrom H, Sneyd JR, Vila P, Johnson T, Muñoz Corsini L, Silverstein JH, Nielsen IK, Moller JT; ISPOCD2 investigators. Cognitive dysfunction after minor surgery in the elderly. Acta Anaesthesiologica Scandinavica. 2003 Nov; 47(10):1204-10
- National Institute for Health and Clinical Excellence (2012). Ambulatory breast cancer surgical care: day case and one night stay. In: NHS Evidence: Quality and Productivity Study. Available at: http://publications.nice.org.uk/pmg6. [Accessed 31/03/2017]
- Marla S, Stallard S. Systematic review of day surgery for breast cancer..Int J Surg. 2009 Aug;7(4):318-23. doi: 10.1016/j.ijsu.2009.04.015. Epub 2009 May 8
- Ballardini B, Cavalli M, Manfredi GF, Sangalli C, Galimberti V, Intra M, Rossi EM, Seco J, Campanelli G, Veronesi P. Surgical treatment of breast lesions at a Day Centre: Experience of the European Institute of Oncology.Breast. 2016 Jun;27:169-74. doi: 10.1016/j.breast.2016.04.002. Epub 2016 Apr 25. P7.
- Yvonne Ying Ru Ng, Patrick Mun Yew Chan, Juliana Jia Chuan Chen, Melanie Dee Wern Seah, Christine Teo, and Ern Yu Tan. Adopting Ambulatory Breast Cancer Surgery as the Standard of Care in an Asian Population. International Journal of Breast Cancer, vol. 2014, Article ID 672743, 8 pages, 2014. doi:10.1155/2014/672743
- Athey N, Gilliam AD, Sinha P, Kurup VJ, Hennessey C, Leaper DJ. Day-case breast cancer axillary surgery. Ann R Coll Surg Engl. 2005 Mar;87(2):96-8.
- Steiner CA, Weiss AJ, Barrett ML, Fingar KR, Davis PH. Trends in Bilateral and Unilateral Mastectomies in Hospital Inpatient and Ambulatory Settings, 2005-2013. HCUP Statistical Brief #201. February 2016. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb201-Mastectomies-Inpatient-Outpatient.pdf.
- Troost MS, Kempees CJ, de Roos MA. Breast cancer surgery without drains: no influence on seroma formation. Int J Surg. 2015 Jan;13:170-4. doi: 10.1016/j.ijsu.2014.11.050. Epub 2014 Dec 6..
- Thomson DR, Sadideen H, Furniss D. Wound drainage after axillary dissection for carcinoma of the breast. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No.: CD006823. DOI: 10.1002/14651858.CD006823.pub2.
- Talbot ML, Magarey CJ. Reduced use of drains following axillary lymphadenectomy for breast cancer. ANZ Journal of Surgery 2002;72(7):488-90. [PUBMED: 12123509]
- He XD, Guo ZH, Tian JH, Yang KH, Xie XD. Whether drainage should be used after surgery for breast cancer? A systematic review of randomized controlled trials. Med Oncol. 2011 Dec;28 Suppl 1:S22-30. doi: 10.1007/s12032-010-9673-2. Epub 2010 Sep 9.
- Holcombe C, West N, Mansel RE, Horgan K. The satisfaction and savings of early discharge with drain in situ following axillary lymphadenectomy in the treatment of breast cancer. Eur J Surg Oncol. 1995;21:604–606.
- Burke CC, Zabka CL, McCarver KJ, Singletary SE. Patient satisfaction with 23-hour "short-stay" observation following breast cancer surgery. Oncol Nurs Forum. 1997;24:645–651.
- Chadha NK, Cumming S, O'Connor R, Burke M. . Is discharge home with drains after breast surgery producing satisfactory outcomes? Ann R Coll Surg Engl. 2004 Sep;86(5):353-7
- Allen D, Gillen E. Systematic review of the effectiveness of integrated care pathways: what works, for whom, in which circumstances? Int j evid based healthc. 2009 jun;7(2):61-74. doi: 10.1111/j.1744-1609.2009.00127. x.
- Bryson A and Browning J (1999) Clinical audit and quality using integrated pathways of care. Report No.: CA96/01, Edinburgh: CRAG, Clinical Resource and Audit
- Roberts P1, Boldy D, Robertson J. . Use and development of clinical pathways by registered nurses in an acute paediatric setting. Collegian. 2005 Oct;12(4):22-8
- The Health Foundation – Inspiring Improvement (2013). Improving Patient Flow - How two trusts focused on flow to improve the quality of care and use available capacity effectively. [online] Available at: http://www.health.org.uk/sites/health/files/ImprovingPatientFlow_fullversion.pdf. [Accessed 13/11/2017]
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2019-journal/jods-293-august-2019/improving-day-case-mastectomy-rate-a-uk-hospital-experience
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/29260/khan.pdf