Buried Bumper Syndrome: A New Technique of Management « Contents
Sherif Monib1, Andrew Ritchie1 Ahmed Hamad2, & Mohamed Elbeshlawy3
1 General Surgery Department, West Hertfordshire Trust, Hertfordshire, UK.
2 General Surgery Department, The Heart of England Trust, Birmingham, UK.
3 Gastroenterology Department, Mouwasat Hospital, Qatif, Saudi Arabia.
Corresponding author: Sherif Monib MSC MRCS FEBS Email: sherif.monib@whht.nhs.uk
Ethical Approval
No ethical approval was needed for this study as it is a retrospective analysis of slandered practice
Patient’s consent
Written informed consent was obtained from the patient to include images in the article.
Abstract
Percutaneous endoscopic gastrostomy (PEG) has gained wide acceptance as a relatively safe and efficient method for long-term enteral nutrition. A rather unusual complication of PEG is the buried bumper syndrome (BBS) which was first reported in 1988. A buried bumper is associated with very serious complications, such as perforation of the stomach, peritonitis and in reported cases, death.
Endoscopic methods such as the needle knife technique and the push-pull T-technique have been described, but these both require advanced endoscopic skills and are often unsuccessful. Subsequently, the buried inner bumpers are removed surgically, either by making an external incision over the PEG site under local anesthesia or at laparotomy. These approaches can be associated with pain, wound infection, or a gastro-cutaneous fistula. External traction has been suggested. However, this can cause an enormous shearing force and may result in tearing at the PEG site.
We describe the Water Jet technique, a novel method to manage a BBS. It requires simple general endoscopic skills and materials that are readily available at the endoscopy suite or operating room.
We believe this technique has a valid role to play in the management of this condition reducing the need for surgery and also improving patient’s outcome.
Keywords: PEG, Buried bumper syndrome, Water jet.
Introduction
We describe the Water Jet technique, a novel method to manage a BBS. It requires simple general endoscopic skills and materials that are readily available at the endoscopy suite or operating room.
We believe this technique has a valid role to play in the management of this condition reducing the need for surgery and also improving patient’s outcome.
Methods
With the old Percutaneous endoscopic gastrostomy (PEG) tube kept in place, a Computer tomography (CT) scan of the abdomen and pelvis is carried out to rule out anterior abdominal wall collection or intraperitoneal sepsis.
If there is no intraperitoneal sepsis, the patient is then prepared for endoscopy which is usually done by the endoscopist in the endoscopy unit with a surgeon ready with a minor set.
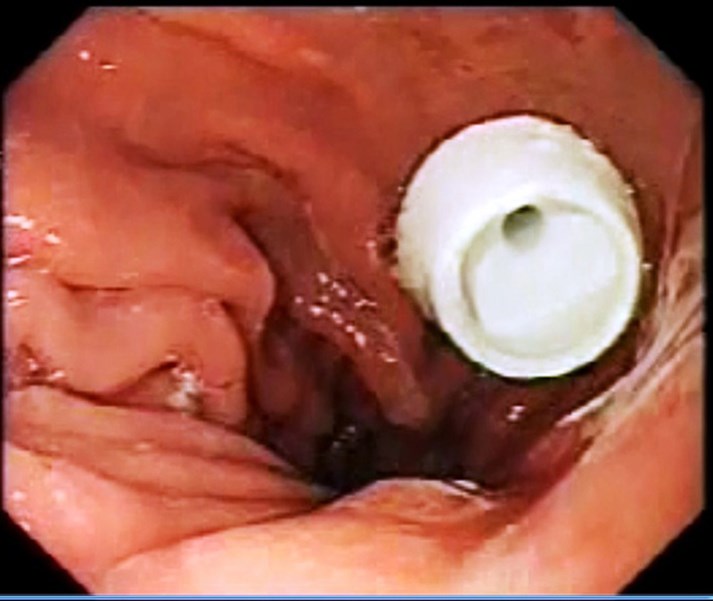
Intravenous antibiotic is given before starting the procedure, with the patient sedated, the abdomen is painted with antiseptic solution and draped, local anesthetic is infiltrated around the PEG tube, endoscopy is carried out, gastrostomy is identified if possible (Fig1), if not, normal saline is injected by the surgeon through the PEG tube and the gastrostomy is identified (Fig 2), the guide wire is passed by the surgeon through the old PEG tube which might need to be shortened. The guide wire is then visualized in the stomach and pulled by the endoscopist (Fig 3) who attaches it to the distal end of a new PEG tube. The surgeon pulls the wire back pulling the new PEG tube which will now replace the old PEG tube which will not be discarded. (Fig4). The team should keep in mind not to put too much pressure on the gastric wall. The PEG tube new is fixed in the usual way.
Figure 1: Endoscopic view identifying the gastrostomy.
Figure 2: Endoscopic view delineating Injection of normal saline by the surgeon through the PEG tube to aid identification of the gastrostomy.

Figure 3: Visualization of the gastrostomy by the endoscopist.

Figure 4: The surgeon pulls the wire back and the old PEG tube is replaced by a new one.
Discussion
PEG has gained wide acceptance as a relatively safe and efficient method for long-term enteral nutrition. A rather unusual complication of PEG is the buried bumper syndrome (BBS) which was first reported in 1988 and described by Klein et al in 1990.[1-3] It is believed to occur in 0.3 – 2.4 % of patients.[4] Excessive tension, leading to ischemia of the mucosa sandwiched between the inner and outer bumpers causes ulceration at the bumper site.[5] The internal bumper becomes lodged along the gastrostomy tract between the gastric wall and skin. Subsequent healing causes overgrowth of gastric mucosa over the inner bumper of the tube leading to mechanical failure of feed delivery, rendering the tube useless. Presenting features1990; 85:448bumper syndrome can include peritubular leakage, occlusion of PEG feeding, external stoma skin erythema or induration, or abdominal pain. [6-13] A buried bumper is associated with very serious complications, such as perforation of the stomach, peritonitis and in reported cases, death.[14]
There are various internal and external techniques for removal of the buried bumper described in the literature. There are a number of known endoscopic techniques. Firstly, the use of needle knife papillotome to expose the internal bumper followed by retrieval with an endoscopic snare after external cutting of the PEG tube.[15,16,17] Secondly, the push and pull “T” technique with a tube fragment grasped by a snare.[18] Thirdly, extraction using the tapered tip of a new PEG tube or extraction using Savary dilator over a guide wire to push the PEG tube towards the lumen of the stomach.[19,20] Finally, an oesophageal balloon dilator is maximally inflated while it is in the tube to make extraction through the stomach possible.[21]
Additionally, successful simple external traction removal was reported with certain externally removable PEG tubes as they have a soft collapsible internal bumper.[21,23] A radiological technique removing the buried bumper was recently described using an angioplasty balloon dilator and radiological guidance.[24] Surgical treatment is required in some cases by mini-laparotomy or a laparoscopic approach.[8,25]
Conclusion
Water Jet technique is a safe easy technique which can be used use for management of cases of BBS not complicated by intra-abdominal sepsis
References
- Shallman RW, Norfleet RG, Hardache JM. Percutaneous endoscopic gastrostomy feeding tube migration and impaction in the abdominal wall. Gastrointest Endosc 1988; 34 367–68.
- Gluck M, Levant JA, Drennan F. Retraction of Sacks-Vine gastrostomy tubes into the gastric wall: a report of seven cases. Gastrointest Endosc 1988; 34 215.
- Klein S, Heare BR, Soloway RD. The ?buried bumper syndrome?: a complication of percutaneous endoscopic gastrostomy. Am J Gastroenterol 1990; 5: 448-51.
- Venu RP, Brown RD. Pastika BJ Erickson LW. The buried bumper syndrome: a simple management approach in two patients. Gastrointest Endosc 2002; 56: 582-584.
- E. Leung, L. Chung, A. Hamouda and A. H. M. Nassar: A new endoscopic technique for the buried bumper syndrome. Surgical Endoscopy Volume 21, Number 9, 1671-1673, DOI: 10.1007/s00464-007-9224-x
- Schwartz HI, Goldberg RI, Barkin JS, Phil lips RS, Land A, Hecht M. PEG feeding tube migration impaction in the abdominal wall. Gastrointest Endosc 1988;35:134.
- Gluck M, Lev ant JA, Drennan F. Retraction of Sacks-Vine gastrostomy tube into the gastric wall: report of seven cases. Gastrointest Endosc 1988;34:215.
- Kaplan DS, Fried MW: Migration of PEG tubes. Am J Gastroenterol 1989;84:1590-1.
- Klein S, Heare BR, Soloway RD. The “Buried Bumper Syndrome”: a complication of percutaneous endoscopic gastrostomy. Am J Gastroenterol 1990;85:448-51.
- Patel PH, Hunter W, Willis M. Upper gastrointestinal hemorrhage secondary to gastric ulcer complicating percutaneous endoscopic gastrostomy. Gastrointest Endosc 1988; 34:288.
- Nelson AM. PEG feeding tube migration and erosion into the abdominal wall. Gastrointest Endosc 1989;35: 133.
- Lee MP. Impaction of gastrostomy tube in the abdominal wall. J Am Geriatr Soc 1990;38:956.
- Boyd JW, Delegge MH, Shamburek RD. The buried bumper syndrome: a new technique for safe, endoscopic PEG removal. Gastrointest Endosc 1995;41:508-11.
- Anagnostopoulos GK, Kostopoulos P, Arvanitidis DM. Buried bumper syndrome with a fatal outcome, presenting early as gastrointestinal bleeding after percutaneous endoscopic gastrostomy placement. J Postgrad Med 2003; 49: 325-7.
- Braden B, Brandstaetter M, Caspary WF, Seifert H. Buried bumper syndrome: treatment guided by catheter probe US. Gastrointest Endosc 2003; 57: 747-751.
- Charles KF. Buried bumper syndrome: Old problem, new tricks. J Gastroenterol Hepatol 2002; 17: 1125-1128.
- Ma MM, Semlacher EA, Fedorak RN, Lalor EA, Duerksen DR, Sherbaniuk RW, Chalpelsky CE, Sadowski DC. The buried gastrostomy bumper syndrome: prevention and endoscopic approaches to removal. Gastrointest Endosc 1995; 41: 505-508.
- Boyd JW, DeLegge MH, Shamburek RD, Kirby DF. The buried bumper syndrome: a new technique for safe endoscopic PEG removal. Gastrointest Endosc 1995; 41: 508-511.
- Venu RP, Brown RD. Pastika BJ Erickson LW. The buried bumper syndrome: a simple management approach in two patients. Gastrointest Endosc 2002; 56: 582-584.
- Reider B, Pfeiffer A. Endoscopic treatment of the buried bumper syndrome. Gastrointest Endosc 2005; 61(5): AB180.
- Strock P, Weber J. Buried bumper syndrome: endoscopic management using a balloon dilator. Endoscopy 2005; 37: 279.
- Frascio F, Giacosa A, Piero P, Sukkar SG, Pugliese V, Munizzi F. Another approach to the buried bumper syndrome. Gastrointest Endosc 1996; 43: 263.
- Lu RG, Koc D, Tozun N. The buried bumper syndrome: migration of internal bumper of percutaneous endoscopic gastrostomy tube into the abdominal wall. Gastroenterology 2003; 38:1077-1080.
- Crowley JJ, Vora D, Becker CJ, Harris LS. Radiologic removal of buried gastrostomy bumpers in paediatric patients. Am J Roentgenol 2001; 176: 766-768.
- Boreham B, Ammori BJ. Laparoscopic percutaneous endoscopic gastrostomy removal in a patient with buried bumper syndrome: a new approach. Surg Laparosc Endosc Percutan Tech 2002; 12: 356-358
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2019-journal/jods-292-may-2019/buried-bumper-syndrome-a-new-technique-of-management
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/26186/292-monib.pdf