Does high body mass index impact surgical outcomes and hospital cost for day case laparoscopic cholecystectomy? « Contents
Authors
Reeya Patel, Nida Mushtaq, Huzaifah Haq, Rupaly Pande, & Chaminda Sellahewa
Russells Hall Hospital, Dudley, West Midlands
Corresponding Author: Ms Reeya Patel Flat 16 Jewel Court,, 29 Legge Lane, Jewellery Quarter,, Birmingham, B1 3LE
Tel: 07908 333186 . Email: reeya.patel@nhs.net
Keywords: Laparoscopic cholecystectomy, obesity, day case, operative outcomes
Abstract
Introduction: Obesity is a known risk factor for the formation of gallstones [1] and has a prevalence of 27% in the UK [2]. High body mass index (BMI) has been associated with poorer perioperative outcomes such as increased operative time and a higher incidence of conversion to open surgery though this risk may be an overestimation [3]. The purpose of this study is to evaluate the outcomes and costs associated with day case laparoscopic cholecystectomy (DCLC) in morbidly obese patients.
Methods: A retrospective analysis of patients who underwent DCLC between December 2015 and November 2017 was performed. Anaesthetic and operating times, pre-operative complications, 30-day readmissions and average costs were compared among WHO classifications for BMI.
Results: There were 332 patients who were listed for DCLC. Morbidly obese patients had a longer anaesthetic and operative time of 4 and 8 minutes respectively compared to healthy patients (24 vs 20, p<0.005; 60 vs 52 p<0.001) There was no significant difference in postoperative complications (2 vs 1, p=0.392) cost (£161.96 vs £162.40 p=0.364) or readmissions (8 vs 2, p=0.149) between morbidly obese and healthy patients. There was no difference in length of stay postoperative (0 vs 0, p=0.371) or proportion of successful DCLC (66 vs 62%, p=0.655).
Conclusions: With rising prevalence of obesity in the UK and chronic bed shortages, indications for inpatient admissions in under scrutiny. This study has shown that morbid obesity is not a contraindication to DCLC and is neither associated with worse outcomes or higher costs.
Introduction
In 1980s the UK had an average day case rate of <15% [4] however twenty years later in the year 2000, the Department of Health identified the number one high impact change for Service Improvement and Delivery as ‘treat day surgery (rather than inpatient surgery) as the norm for elective surgery’ [5]. In 2017, day case surgery represents about 70% of all surgery in the United Kingdom [6] with the major drive promoting day case surgery being the advantages of no impatient stay and therefore reduced costs to the National Health Service (NHS) [4]. The Department of Health have developed a benchmarking tool, which is specific to day case laparoscopic cholecystectomy (DCLC); they have advised that 46.8% should be performed as a day case procedure [6].
Day case surgery can be considered for a cohort of patients who have a relatively good physiological baseline where they can undergo a surgical procedure and be discharged home on the same day. Patient assessment for day case surgery falls into three categories: medical, surgical and social factors with obesity categorised as a medical factor [7].
Although many surgeons believe that operating on patients with a body mass index (BMI) greater than 30 is more technically challenging and associated with increased operative complications, this perception is not supported by the literature [8, 9]. The relationship between obesity and operative outcomes remains controversial. Given that obesity is a major risk factor for gallstone disease it appears that a large proportion of patients undergoing DCLC fall into a high BMI category enabling us to explore this relationship [10].
On the contrary, operating on patients with a higher BMI has been associated with an increased operative time and a higher incidence of conversion to open for laparoscopic cholecystectomy [11]. Additionally a high BMI poses a greater risk on post-operative complications such as surgical site infections and post-operative ileus [11].
Despite the healthcare striving towards a shared goal of improving productivity within the NHS, obesity has consistently shown to increase operating time for a laparoscopic cholecystectomy [12,13].
In 2016-2017 the NHS spent a total on £4.5bn [14] on day case surgery where patients are expected to be discharged on the same day. A further £17bn was spent on non-elective inpatient stay which includes patients who are kept in hospital following a planned day case procedure and these figures are rising year on year. When analysing the outcomes of obese patients who underwent a DCLC it is important for us to consider whether we have observed an increase in hospital stay in this category and whether this translates into an increased cost to the NHS.
In our study, we looked at perioperative and postoperative outcomes including mean anaesthetic time, mean operative time, operative complications, postoperative inpatient stay, causes of postoperative inpatient stay, average cost of inpatient stay and rate of successful DCLC for the 5 BMI patient groups (underweight <18.5kg/m2, healthy weight (18.5- 24.9kg/m2, overweight 25.0-29.95kg/m2, obese 30.0-39.9kg/m2 and morbidly obese (>40.0kg/m2).
The study analysed data for 332 patients undergoing DCLC with a BMI range 16.6 kg/m2 to 53.9 kg/m2. The aim of this study is to determine whether operating on a cohort of patients with a higher BMI translates into higher healthcare costs and therefore negatively impact on health expenditure. This would then raise the question whether we need to reassess how we operate on this cohort of patients and do we need to devise more specific guidelines with regards to DCLC and patient selection.
Methods
Patient eligibility
Data from 332 patients who underwent an elective laparoscopic cholecystectomy performed by one of the upper gastrointestinal consultant surgeons at a single district general hospital were analysed. Retrospective data included: age, gender, BMI, American Society of Anaesthesiologists (ASA) score, operative time, intraoperative complications, duration of inpatient stay, cost of inpatient stay and readmission. The inpatient stay was the number of inpatient days purely associated with a postoperative day case admission and the readmission rate was calculated using the number of patients readmitted with a postoperative complication within the 30-day post-operative period.
Data was collected from clinical notes in addition to computerised operative notes, which were prospectively maintained between December 2015 and November 2017.
Local eligibility criteria for day case laparoscopic cholecystectomy included symptomatic gallstone disease and an ASA of ≤3, fitness for day case general anaesthesia, performance status ≤2 and an accompanying adult to escort the patient home attend to the patient in the first 24 hours post-operatively.
Operative technique
All laparoscopic cholecystectomies were performed using a standardised surgical approach. All laparoscopies were performed using the 4-port technique with infiltration of 5mls 0.5% bupivacaine prior to each incision.
The patients were positioned supine with an assistant to the right and the senior surgeon to their left. A supra- or infraumbilical incision was made for the optical port and a pneumoperitoneum was created using the open Hasson technique. Once a 30- degree 10mm telescope was introduced via the umbilical port, the remaining epigastric and two right subcostal ports were inserted under direct vision.
The patient was then positioned in a reverse Trendelenberg and left lateral tilt. Dissection started in the Calot’s triangle and completed once the cystic duct, cystic artery and cystic-CBD junction was visualised. The cystic artery was then clipped and divided. A trans-cystic cholangiogram was obtained for each patient and after applying a Rhoder’s knot, the cystic duct was also clipped and divided.
The gallbladder was dissected from the liver bed and retrieved via the umbilical port in a Bert’s bag. Once haemostasis achieved, all ports were removed under direct vision and 10mls of 0.5% levobupivacaine were used to infiltrate the liver bed.
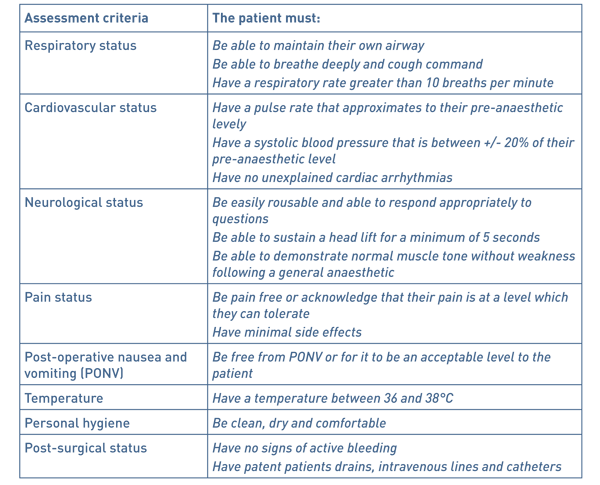
An anaesthetist accompanied patients to day case theatre recovery and once they met local day case theatre recovery discharge criteria (see Table 1) they were discharged home. If there were any post-operative complications or they did not meet recovery discharge criteria the patient was admitted to the surgical ward.
Table 1 Local day case recovery discharge criteria.
Patient data was divided into 5 groups: underweight (<18.5kg/m2), healthy weight (18.5- 24.9kg/m2), overweight (25.0-29.95kg/m2), obese (30.0-39.9kg/m2) and morbidly obese (>40.0kg/m2).
Post-operatively data was collected retrospectively to determine whether patients were deemed unfit for discharge from day case recovery or whether patients were re-admitted within 30 days with post-operative complications.
Data was stored in SPSS software where the Mann Whitney-U statistical tests was run on the anaesthetic time, operative time and hospital cost data sets and the Chi-squared test was run on the gender, postoperative admission and readmission data sets.
Results
Data for 332 patients who underwent a day case laparoscopic cholecystectomy between December 2015 and November 2017 was collected.
Demographic data included age of patients, male to female ratio and average ASA grades within the five BMI patient groups (see Table 2). The mean age of patients was 51.8 years (range 17-84 years). 245 out of the 332 patients were female (72.92%) and there were significantly more females than males in various patient groups: firstly, the obese BMI patient group in comparison to the healthy BMI patient group (p=0.019) and the morbidly obese BMI patient group in comparison to the healthy BMI and overweight BMI patient groups (p= 0.001 and 0.033 respectively).
Table 2 Demographic data of 332 patients undergoing day case laparoscopic cholecystectomy
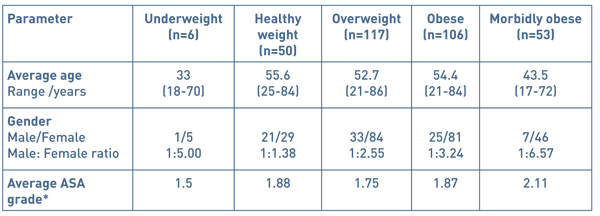
* American Society of Anaesthesiologists physical status classification system:
ASA 1- a normal healthy patient
ASA 2- a patient with mild systemic disease
ASA 3- a patient with severe systemic disease
ASA 4- severe systemic disease that is a constant threat to life
ASA 5- a moribund patient that is not expected to survive 24 hours with or without an operation
Table 3 Indication for day case laparoscopic cholecystectomy
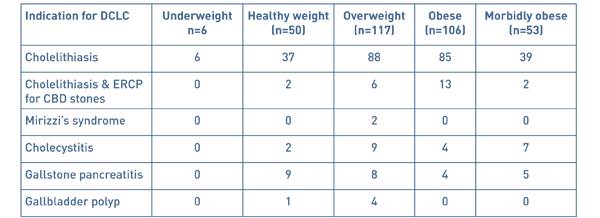
There were several indications for a laparoscopic cholecystectomy, the most common being biliary colic and the rest more severe complications of gallstone disease (see Table 3).
Perioperative and postoperative outcomes included mean anaesthetic time, mean operative time, operative complications, postoperative inpatient stay, causes of postoperative inpatient stay, average cost of inpatient stay and rate of successful DCLC for the 5 BMI patient groups (see Table 4).
Table 4 Perioperative and postoperative outcomes of 332 patients undergoing day case
laparoscopic cholecystectomy.
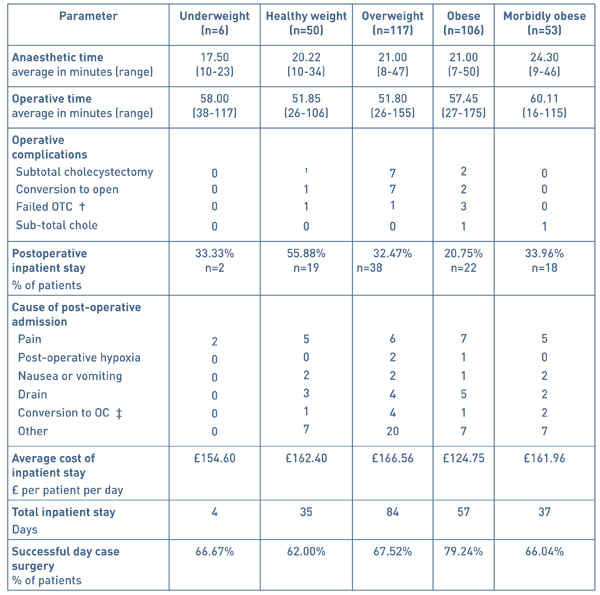
†: on table cholangiogram ‡: open cholecystectomy
Anaesthetic time data was analysed using the Mann Whitney-U test and ranged from 7 to 50 minutes. Patients who were morbidly obese (BMI ≥40) took significantly longer to anaesthetise in comparison to the underweight, healthy weight, overweight and obese patients (p=0.015, 0.001, 0.004 and 0.001 respectively).
The operating time was measured as knife-to-skin to the completion of the laparoscopic cholecystectomy and ranged from 26 to 175 minutes. Data for operating times were analysed using the Mann Whitney-U test and resulted in significant differences amongst the various BMI groups. The operative times for morbidly obese patients were significantly higher compared to the patient s from the BMI groups: healthy weight, overweight and obese (p= 0.001, 0.001 and 0.046 respectively). In addition, the operative time for patients in the obese weight patient group was significantly greater than the patients in the overweight patient group p= 0.009. The most frequent operative complication was a conversion to an open cholecystectomy and occurred mostly in the overweight BMI group with 6% being converted to an open procedure.
Day case laparoscopic was successful in 70.2% of patients with 233 out of 332 patients being discharged home on the same day of their operation and the remaining 99 requiring a post-operative hospital admission.
The cost of an inpatient stay per night accounted to £232.00 and means were calculated per BMI group using the total number of days of admission for each group. The BMI group, which on average cost the hospital the greatest, was the overweight group (£166.56 per patient per day, n=117) due to a total of 84 days of hospital admission in the immediate post-operative period. The patients from the healthy weight BMI group cost significantly more than from the obese weight BMI group with a mean difference of £37.65 per patient per day.
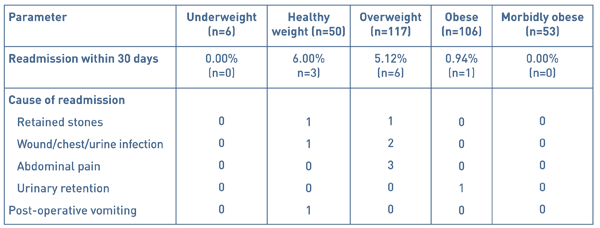
10 patients out of 332 were readmitted to hospital within the 30-day post-operative period (see Table 5). Of these, none were readmitted from the underweight BMI group and the majority (6 patients) from the healthy BMI patient group with a readmission rate of 6%. There was no significance between the readmission rates amongst the five patient BMI groups.
Table 5 Hospital readmissions and cause of readmission within the 30-day post-operative period
Discussion
Worldwide obesity has tripled since 1975 with recent data from the World Health Organisation showing a staggering 1.9 billion adults classified as overweight and of these 650 million obese in 2016[15]. In view of the exponential increases in obesity worldwide, particularly in the United Kingdom, does an increasing overweight population pose additional stress on the deficient NHS budget?
In view of health economics, several studies have looked into the cost impact of obesity on healthcare costs. Sturm et al. found that within the United States, obese adults have on average 36% higher annual medical costs in comparison to those of a healthy weight [16] with Cawley et al. estimating the surplus at approximately $2,741 per person [17].
The Department of Health highlights day case surgery as a means to improve efficiency within the NHS to firstly reduce bed days and secondly reduce other complications associated with inpatient stay such as nosocomial infections and venous thromboembolic disease. Although patient selection for day case surgery has been outlined in national guidelines [4], no numerical cut-off for BMI has been specified leaving us with the crucial question is operating on obese patients less cost and time efficient? Although several studies have proved that operating on obese and morbidly obese patients can lead to longer operating times and higher postoperative complications, we are the first study to look into the cost impact of these on the hospital expenditure.
As the Office for Budgetary Responsibility has projected in their latest Fiscal Sustainability Report health spending is likely to rise significantly as a proportion of gross domestic product over the coming decades, as a result of demographic pressures but also growing technology costs and rising demand [18]. Therefore, examining the cost of operating on this cohort of patients becomes of paramount importance given the current economic climate.
The following perioperative and postoperative outcomes for patient cohorts of varying BMIs will be discussed and whether performing elective DCLC on obese and morbidly obese patients bears any significance on medical costs.
Anaesthetic time
Anaesthesia of the obese and morbidly population can prove technically challenging due to a large tongue, excessive pharyngeal tissue, a high anterior larynx and restricted atlanto-occipital flexion and extension [19]. Of particular concern, patients with features suggestive of obstructive sleep apnoea syndrome, more common in the obese population, can imply potential airway obstruction once the patient has been rendered unconscious [20]. As can be relayed from this study’s results, patients in the morbidly obese BMI groups (BMI ≥40) have taken significantly longer to anaesthetise than patients in the underweight, healthy weight, overweight and obese BMI groups (p= 0.015, 0.001, 0.004 and 0.001 respectively). Morbidly obese patients are likely to present considerable airway difficulties due to the anatomical difficulties mentioned above, with 15% quoted in the literature as difficult intubations [21]. Interestingly, Brodski et al. studied the intubation of 100 morbidly obese patients to identify the factors that complicate tracheal intubation and found that increasing neck circumference and a Mallampati score of ≥3 led to a problematic intubation [22]. Although statistical differences in anaesthetising morbidly obese patients in comparison to patients with a BMI<40, a difference of 2-3 minutes does not bear substantial clinical significance and in practice does not affect the efficiency of day case theatre.
Operative time
Morbid obesity can be considered a significant risk factor for day case laparoscopic cholecystectomy due to a well-known association with increases in operative time [11], however this is the first study to assess whether these endpoints translate into greater healthcare costs.
Operative time results are comparable to other studies published in the literature with significantly higher operative times in the obese (mean operative time 57.45 minutes) and morbidly obese (mean operative time 60.11 minutes) patient groups compared with the overweight BMI patient group (mean operative time 51.80 minutes, p=0 .009 and < .001 respectively) [23]. These are likely due to a difficulty gaining access to the abdomen secondary to an increased amount of subcutaneous fat and difficult dissection of the gallbladder secondary to a greater amount of omental fat [23]. In reality, the difference in the mean operating time of 8.26 minutes between the morbidly obese and healthy weight patient groups is unlikely to cause significant disruption to an elective day case list due to other influencing factors such as anaesthetic time and pre-operative preparation time. Despite this discrepancy of operative time between the patient groups, literature suggest that converting to an open procedure for obese patients does not improve operating times nor patient recovery post-operatively and in fact, the laparoscopic approach is favourable for these patients [24, 25].
Operative complications
The overall conversion rate to open for this study was 3.01% that is on par with the conversion rate of 3.9-6.0 % cited in recent literature [23, 26]. Out of the 10 patients where laparoscopic surgery was converted to open, 7 were from the overweight patient group.
Postoperative admissions
This study highlighted that there is no significant increase in overnight stay post-operatively in the obese and morbidly obese patients. In fact our study showed a significantly higher admission rate for the healthy weight group when compared to the obese patient group (p=0.224). As one may predict, the majority of patients required an inpatient stay due to post-operative pain particularly after a conversion to open cholecystectomy and post-operative nausea and vomiting.
Admission cost
Admission costs were calculated using the total number on days of hospital stay per BMI group and the highest costing group was the overweight group with an average cost of £166.56 per patient per day. Surprisingly, the average cost of postoperative inpatient stay from the healthy weight BMI group was significantly greater than the obese weight BMI group (p=0.049). These results are contrary to the findings of an extensive systematic review carried out by Tsai et al. who estimated incremental medical costs of overweight as approximately $266 higher, and of obesity $1,723 higher, than that of normal weight persons [27]. However comorbidities associated with obesity such as hypertension and diabetes are more likely causes of these higher medical costs as opposed to elective surgical procedures. What our study concludes is that performing an elective DCLC is no more costly on patients with a BMI of >30 in comparison to those of a healthy weight.
Readmissions
In the post-operative period patients were followed up for a readmission within 30 days and of the 332 patients, 10 patients were readmitted giving a readmission rate of 3.01%. Most patients were from the overweight BMI patient group (n=6): 3 patients were readmitted due to post-operative pain, 2 due a surgical site infection and 1 patient due to a retained common bile duct stone. Of the remaining 4 patients; 1 patient was admitted with post-operative vomiting, 1 with acute urinary retention, 1 with a retained common bile duct stone and lastly 1 with a surgical site infection.
There were no significant difference between readmission rates amongst the 5 BMI patient groups and interestingly no patients from the morbidly obese patient group were readmitted. These results however do not take into account any post-operative complications that may present within the community and treated without an admission.
Despite this, our study shows that although 47.89% of patients who underwent a DCLC had a BMI of ≥30, there was no impact on overall costs of treating these patients when taking into account postoperative admissions into hospital.
These findings demonstrate that morbid obesity is not a hindrance to elective day case surgery lists and that with adequate preparation, operating on these patients is as efficient as patients with a healthy BMI.
Article continues after ad.
Conclusions
DCLC should be performed in patients with a higher BMI. Obesity can have an impact on the anaesthetic and operating times of a day case laparoscopic cholecystectomy however this in turn makes no significant difference to the rate of postoperative admissions, readmissions and most importantly cost. Our study suggests that as surgeons we should disregard the hesitancy towards performing elective day case procedures on high BMI patient as they do not lead to poorer surgical outcomes and crucially, they do not incur higher medical cost. The fundamental point to take away from this study is that although there is an evident increase in the prevalence of obesity it bears no influence on efficiency within the NHS with regards to the hospital costs of elective DCLC.
References
- Erlinger S. Gallstones in obesity and weight loss. Eur J Gastroenterol Hepatol 2000; 12: 1347–1352
- NHS Digital. Statistics on obesity, physical and activity [Internet]. National Statistics; 2017 [cited 2017March30]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/613532/obes-phys-acti-diet-eng-2017-rep.pdf
- Vaughan J, Gurusamy KS, Davidson BR. Day-surgery versus overnight stay surgery for laparoscopic cholecystectomy. Cochrane Database Syst Rev 2013; 7: CD006798.
- Day surgery development and practice: key factors for a successful pathway. Continuing Education in Anaesthesia Critical Care & Pain, 2014, 14 (6):256–261
- Quemby DJ, Stocker ME, Day Surgery Development and practice: key factors for a successful pathway. Continuing Education in Anaesthesia Critical Care & Pain, Volume 14, Issue 6, 1 December 2014:256–261
- NHS England. 10 High Impact Changes for Service Improvement and Delivery [Internet]. NHS Modernisation Agency; 2004 [cited 2018Mar29]. Available from: https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/10-High-Impact-Changes.pdf
- Verma R, Alladi R, Jackson I, Johnston I, Kumar C, PageR, Smith I, Stocker M, Tickner C, Williams S, Young R. Day case and short stay surgery: 2, Anaesthesia 2011; 66: pages 417-434
- Reeves BC, Ascione R, Chamberlain MH, Angelini GD. Effect of body mass index on early outcomes in patients undergoing coronary artery bypass surgery. J Am Coll Cardiol 2003;42:668–76
- Dindo D,Muller MK, Weber M. Obesity in general elective surgery. Lancet 2003;361:2032–5
- Bonfrate L, Wang DQ, Garruti G, Portincasa P. Obesity and the risk and prognosis of gallstone disease and pancreatitis. Best Pract Res Clin Gastroenterol. 2014 Aug;28(4):623-35
- He Y, Wang J, Bian, H, Deng X, Wang Z. BMI as a Predictor for Perioperative Outcome of Laparoscopic Colorectal 4. Laparoscopic cholecystectomy in obese and nonobese patients. Obes Surg. 1999 Oct;9(5):459-61
- Surgery: A Pooled Analysis of Comparative Studies. Diseases of the Colon & Rectum. 60. 433-445. 10.1097/DCR.
- Subhas G, Gupta A, Bhullar J et al. Prolonged (longer than 3 hours) laparoscopic cholecystectomy: reasons and results. Am Surg. 2011 Aug;77(8):981-4.
- NHS Improvement. Finance and use of Resources [Internet] NHS England 2017. [cited 2018Apr07]. Available from: https://improvement.nhs.uk/resources/reference-costs/
- World Health Organization. Obesity and overweight [Internet]. World Health Organization; 2018 [cited 2018Mar29]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/
- Sturm, R. The effects of obesity, smoking, and drinking on medical problems and costs. Obesity outranks both smoking and drinking in its deleterious effects on health and health costs. Health Aff (Millwood). 2002 Mar-Apr;21(2):245-53.
- Cawley J1, Meyerhoefer C. The medical care costs of obesity: An instrumental variables approach. J Health Econ. 2012 Jan;31(1):219-30.
- Office for Budget Responsibility. Fiscal Sustainability Report [Internet] OBR. 2017. [cited2018Apr07] Available from: http://cdn.obr.uk/FSR_Jan17.pdf
- Barash PG, Cullen BF, Stoelting RK. Anesthesia and obesity and gastrointestinal disorders. Clinical Anesthesia, 1992: 1169–83.
- Adams J, Murphy P. Obesity in anaesthesia and intensive care. British Journal of Anaesthesia, 2000 July(85): 91–108
- Buckley FP, Robinson NB, Simonowitz DA, Dellinger EP. Anaesthesia in the morbidly obese. A comparison of anaesthetic and analgesic regimens for upper abdominal surgery. Anaesthesia. 1983 Sep;38(9):840-51.
- Brodsky, Jay B. Lemmens, Harry J. M., Brock-Utne, John G., Vierra, Mark, Saidman, Lawrence J. Morbid Obesity and Tracheal Intubation. Anesthesia & Analgesia: March 2002 - Volume 94 - Issue 3 - p 732-736
- Malla BR1, Shrestha RK. Laparoscopic cholecystectomycomplication and conversion rate. Kathmandu Univ Med J (KUMJ). 2010 Oct-Dec;8(32):367-3369.
- Harju J, Juvonen P, Eskelinen M, Miettinen P, Pääkkönen M. Minilaparotomy cholecystectomyversus laparoscopic cholecystectomy: a randomized study with special reference to obesity. Surg Endosc. 2006 Apr;20(4):583-6
- Miles RH1, Carballo RE, Prinz RA, McMahon M, Pulawski G, Olen RN, Dahlinghaus DL. Laparoscopy: the preferred method of cholecystectomyin the morbidly obese. Surgery. 1992 Oct;112(4):818-22
- Harboe KM1, Bardram L. Nationwide quality improvement of cholecystectomy: results from a national database. Int J Qual Health Care. 2011 Oct;23(5):565-73.
- Tsai AG, Williamson DF, Glick HA. Direct medical cost of overweight and obesity in the United States: a quantitative systematic review. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12(1):50-61.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6108/291-patel.pdf
