Improving Care in Anaesthetics: A quality improvement project focusing on adherence to pre-operative testing guidelines in elective surgery patients « Contents
Authors
Amy Boalch – Final Year Medical Student, King’s College London (amy.boalch@kcl.ac.uk)
Laura Alger Final Year Medical Student, King’s College London
Alexander Johnston – Final Year Medical Student, King’s College London
Sejin Hwang Final Year Medical Student, King’s College London
Dr Emma Jackson Consultant Anaesthetist, University Hospital Lewisham
Dr Beenu Madhavan Consultant Anaesthetist, University Hospital Lewisham
Keywords: Quality Improvement; Pre-operative Testing; NICE Guideline NG45; Elective Surgery.
Abstract
Introduction: We focused on compliance with NICE guidelines NG45 for pre-operative testing at University Hospital Lewisham in elective surgery patients between October 2017 and February 2018. Aims included:
- Increasing the number of pre-operative tests performed appropriately.
- Reducing the number of tests performed unnecessarily.
Methods: Data was collected from 100 randomly-selected patients before intervention implementation and 93 patients afterwards, which comprised a poster displaying guidelines in a clear, staff-focused format. The intervention was identified through patient shadowing and root-cause analysis and improved through sequential Plan-Do-Study-Act cycles.
Results: Baseline data demonstrated 65.7% concordance. ECG concordance was greatest (73.0%) followed by U&Es (65.0%), clotting (63.8%) and FBC (61.0%). Post-intervention, overall concordance increased to 69.5%. ECG testing saw a 19.3% improvement (87.1%) whilst U&Es and FBC testing displayed reductions (63.0% and 59.2% respectively). Clotting increased to 68.5%. Concordance was greatest for major surgery (73.0%) and lowest for minor surgery (55.0%). ASA-3 grades showed notably high concordance (93.2%).
Conclusions: A 5.8% concordance increase was achieved. Concordance was greatest for high ASA or surgery grades as more tests are justified at greater risk levels. Where concordance was low, the cause was inappropriately completed tests indicating over-testing. This demonstrates an area of unnecessary financial expense. Additionally, the patient experience could be improved by reducing excessive testing. Further work is needed to educate staff on minor surgery guidelines and to emphasise the negative sequelae of over-testing. Clinicians should be encouraged to question why they are ordering tests and evaluate patient benefit.
Introduction
There are numerous studies which point to routine pre-operative testing being labour intensive, expensive and stressful for patients. Such assessment may also increase delays and morbidity due to false or unnecessary results which must then be acted upon1. It may also be true that testing only influences patient management in a small proportion of cases2.
With the number of elective surgeries rising by a factor of 1.6 between 2002/03 and 2012/13 to 10.6 million3; if even a tiny proportion of patients are subjected to unnecessary testing, the total number of patients being overexposed to the associated risks will be significantly high.
Nonetheless, it is of paramount importance that patients undergo rigorous assessment prior to any elective surgery. These tests are essential to define the risks of the surgery to the patient in question and guide healthcare professionals as to the best ways to mitigate these hazards, therefore optimizing patient care and outcomes4.
The National Institute of Health and Care Excellence (NICE) NG455 guideline outlines the requirements for elective pre-operative testing in the UK. It saw a significant update in 2003 (further updates have since occurred) in which it reduced testing requirements for healthy patients and emphasised the importance of general practitioners passing on test results to minimise unnecessary repetition6. These guidelines exist and are imperative, not only for patient safety, but moreover for efficiency.
With these factors in mind, the aim of this quality improvement process was to assess and improve pre-operative assessment compliance, specifically regarding full blood count (FBC), urea and electrolytes (U&Es), clotting and electrocardiogram (ECG) testing, with local guidance at University Hospital Lewisham (UHL). These criteria were drawn from the NICE guideline NG455, which was modified in line with local clinical needs; as agreed by anaesthetic and surgical department leads at UHL.
The project measured randomly selected patients who underwent elective surgery between October 2017 and February 2018 and aimed to increase the number of pre-operative tests performed appropriately, whilst reducing the number of tests performed unnecessarily.
Methods
This project was designed in close alliance with a host of healthcare professionals including anaesthetists, surgeons, nurses and healthcare assistants who recognized discrepancies in pre-operative testing and the guidelines set by NICE. Before embarking on an intervention to make improvements, a pilot study was run to collect data and identify whether such discrepancies truly existed. Data was collected from randomly-selected patient notes on surgical wards at UHL until 100 patients were reached. No identifiable information was recorded. ASA grades and surgery grades were collected as well as all the pre-operative testing received.
To identify the role that quality improvement could play, the patient journey was shadowed and reflected upon with all the influences upon pre-operative testing being recognised. An Ishikawa diagram was constructed illustrating all of these contributing factors. We used the Pareto Principle to establish the key factors largely contributing to the poor adherence. Through a process of multi-voting we concluded that the root cause was a lack of easy access to the NG45 guidelines.
Following the decision to focus on access to the guidelines, we engaged with pre-operative staff and developed a poster in a clear format that displayed the relevant information in a user-friendly layout. Through a series of Plan-Do-Study-Act (PDSA) cycles we continuously improved upon this poster and gained feedback from multiple healthcare professionals through various meetings and surveys. We displayed the final poster within the pre-operative assessment clinic and then re-collected further patient data in the same way to identify any changes.
All data was analysed retrospectively in relation to the information displayed on the interventional poster. Concordance was measured as the percentage of appropriately done tests. We analysed data relating only to four main tests: FBC, U&Es, clotting and ECG.
Results
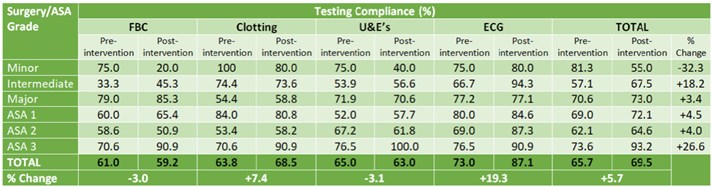
The pilot study involving 100 patients provided a baseline concordance of 65.7%. ECG concordance was greatest at 73.0% followed by U&Es, clotting and FBC with concordances of 65.0%, 63.8% and 61.0% respectively. Concordance varied with both ASA grades and surgery grades (Table 1); most notably minor surgeries had concordance rates of 81.3% compared to the 57.1% concordance rates seen with intermediate surgeries. Variation was less significant with ASA grades (ASA1 69.0%, ASA2 62.1%, ASA3 73.6%). It is pertinent to note that due to our small sample size, the distribution across ASA and surgery grades was not equal.
After displaying the interventional poster, concordance increased to 69.5%, a 5.8% improvement from the baseline. ECG testing presented the greatest change with a 19.3% improvement in concordance whilst conversely FBC and U&E testing displayed reductions in the number of appropriate tests. Concordance was greatest for major surgery (73.0%) and lowest for minor surgery (55.0%). ASA 3 grades showed notably high concordance levels of 93.2%.
TABLE 1: Compliance of individual pre-operative tests with pre-operative assessment guidelines at
UHL compared against surgery grades and American Society of Anaesthesiologists (ASA) grades
both pre- and post-intervention.
Discussion
The results indicate that testing was more aligned to recommendations when ASA or surgery grades were high, both pre- and post-intervention. This is likely because, as the risk of a procedure increases, more tests are justified and appropriate. Likewise, ECG concordance values remained higher than for other tests. We hypothesise that this is because blood tests are standard and frequently used investigations thus are consequently overused, whereas ECG is considered more specific to the clinical picture. Therefore, we theorise that perhaps clinicians more carefully consider the need for ECG testing than other investigations. Work must be done to emphasise that no testing should be considered standard practice and instead clinicians should always be thinking about why they are ordering each test.
Unnecessary pre-operative tests translate as unnecessary financial costs; the Lewisham and Greenwich Trust objectives for financial stability in 2017/18 include ‘making the best use of resources’ 7. This project demonstrates an area where resources are being wasted and can thus be targeted. Furthermore, on a national level, with elective operations on the rise2, even a single unnecessary test per patient can rapidly accumulate and add to the NHS’s financial burden.
Likewise, unnecessary tests act to inflate patient anxiety and distress8 which is true not only at UHL but is echoed across the UK. Ensuring that only essential tests are performed would improve the patient experience and accordingly improve outcomes9.
The project further demonstrated the resistance to change that can exist in healthcare systems and the consequent difficulty of quality improvement, especially when conducted by medical students. Four PDSA cycles were utilised throughout the project in which feedback was continuously received. This allowed the intervention to be improved upon but equally demonstrates the difficulty in finding solutions to meet the needs of everyone. That being said, only one intervention was focussed on during this six-month project and likewise only a small area of hospital testing was included.
Despite involving healthcare professionals, a great limitation of the project was a lack of uptake by staff members. Without the motivation to use the resource we created, the intervention was ineffective. Staff motivation should have been a greater priority in our project from the beginning in order to optimise participation, possibly by mode of a second educational intervention.
It is acknowledged that to ideally demonstrate an improvement in concordance with NG45, the intervention would be introduced over a much longer period of time than was possible within the scope of this project. In conjunction with this, running staff training sessions in parallel with the poster intervention would be a desirable adjunct that could help to improve motivation and awareness. Plotting a series of data points on a run chart over an extended period of time would allow any true changes to be seen, something that was not achieved during this initial project.
The difficulty lies in the art of continuing to improve and maintain high levels of concordance at Lewisham and Greenwich Trust, not least because the time and resources required for this would be significant. Additionally, to expand this project to improve pre-operative testing guideline adherence across a multitude of hospital trusts would likewise be a significant demand on NHS resources.
Conclusions
A 5.9% concordance increase was achieved. The intervention of designing an accessible format for the pre-operative guidelines at UHL resulted in this marginal increase, however this failed to meet our intended aim of 90% concordance. Concordance was greatest for high ASA or surgery grades as more tests are justified at greater risk levels. Where concordance was low, the cause was inappropriately completed tests indicating over-testing.
This over-testing demonstrates an area of unnecessary financial expense and potentially a negative patient experience. Further work is needed to educate staff, specifically on minor surgery guidelines, to emphasise the negative sequelae of over-testing. Clinicians should be encouraged to question why they are ordering tests and evaluate patient benefit in every case.
Our intervention offers a semi-permanent improvement as the resource is now a tool which will remain in clinics. To continue developing our intervention more time is needed to gather the necessary feedback and quantitative data and thus continue with PDSA cycles until a higher concordance is reached. Staff engagement is imperative to the success of the project and methods to achieve engagement need to be incorporated into further cycles.
References
- Klein, A. & Arrowsmith, J. (2010). Should routine pre‐operative testing be abandoned? Anaesthesia, 65(10), 974-976.
- O'Neill, F., Carter, E., Pink, N. & Smith, I. (2016). Routine preoperative tests for elective surgery: Summary of updated NICE guidance. BMJ: British Medical Journal (Online), 354.
- Bryson, G.L., Wyand, A. & Bragg, P.R. (2006). Preoperative testing is inconsistent with published guidelines and rarely changes management. Canadian Journal of Anesthesia, 53(3), 236-241.
- Garcia-Miguel, F.J., Serrano-Aguilar, P.G. & Lopez-Bastida, J. (2003). Preoperative assessment. The Lancet, 362(9397), 1749-1757.
- National Institute for Health and Care Excellence (April 2016) Routine preoperative tests for elective surgery. NICE guidelines (NG45) https://www.nice.org.uk/guidance/ng45.
- Torjesen, I. Healthy people need fewer preoperative tests for elective surgery, says NICE. BMJ: British Medical Journal (Online). 2016 Apr 5;353.
- Lewisham and Greenwich NHS Trust Annual Report 2016/17, page 28. https://www.lewishamandgreenwich.nhs.uk/important-documents, last accessed 06/03/2018.
- O’Neill F, Carter E, Pink N, Smith I. Routine preoperative tests for elective surgery: summary of updated NICE guidance. BMJ. 2016 Jul 14;354:i3292.
- Mavros, M.N., Athanasiou, S., Gkegkes, I.D., Polyzos, K.A., Peppas, G. & Falagas, M.E. (2011). Do psychological variables affect early surgical recovery?. PloS One, 25;6(5):e20306.
Ethical approval was not required and ethics committee approval was not sought. There are no conflicts of interest to declare. No sources of funding were accessed for this project.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6051/284-boalch.pdf