Day Case GreenLight XPS Prostatectomy, A Single Centre Experience « Contents
Authors
Varnavas Michalis, Manash Debbarma, Ram Beekharry & Nirgan Gogoi
Department of Urology, Mid Yorkshire NHS Trust, Pinderfields General Hospital, Aberford Rd, Wakefield WF1 4DG.
Corresponding author
Michalis Varnavas
St James University hospital, Urology Department, Beckett St, Leeds LS9 7TF.
Email: michail11@hotmail.co.uk
Keywords: Greenlight XPS, prostatectomy, Day Case Surgery
Abstract
Introduction: Benign prostatic hyperplasia (BPH) describes an increase in the prostate size due to the proliferation of cells which may lead to bladder outflow obstruction. We present our experience of day surgery Greenlight XPS prostatectomy over a period of 4 years.
Methods: This is a retrospective analysis of the day case GreenLight XPS Prostatectomies performed between January 2013 and September 2016 at Mid Yorkshire NHS trust. We reviewed our electronic medical records and recorded the percentage of operations performed as day cases at a yearly interval. Also, we documented potential risk factors that may be associated with prolonged length of stay. These include age, ASA score and preoperative retention/ catheterization. We also recorded the rate of successful trials without catheter for each group.
Results: Between 2013 and 2016 we performed 448 GreenLight XPS prostatectomies. The percentage of these procedures performed as day case per year increased to reach 76%. There was statistical significance between patients with age >80, ASA equal or > 3, prior retention/ catheterisation and a longer duration of stay. The readmission rate at 30 days was 6.8% for the day cases and 10.5% for the patients with longer stays. Finally, 95% of the "day case" patients had a successful TWOC. For the patients that had a longer stay the rate of successful TWOC was 92%.
Conclusions: Green-light XPS prostatectomy can be performed effectively and safely as a day case for majority of the patients with appropriate service alterations.
Introduction
Benign prostatic hyperplasia (BPH) describes an increase in the prostate size due to the proliferation of cells. Gradually this will lead to bladder outflow obstruction which may manifest as obstructive lower urinary tract symptoms. The incidence of BPH is 50–60% in men aged 60–70 years and increases to 80–90% by ages 70–80 years. (1) Despite available pharmacotherapy to treat this condition a great proportion of men will progress to require surgical intervention to improve symptoms. Traditional TURP is the standard of care for BPH in Europe, with open prostatectomy and HOLMIUM laser enucleation reserved for patients with larger glands (prostate >80 mL). (2) Green light laser prostate vaporisation however has been gaining recognition and acceptance in treating BPH as is included in new NICE guidelines (3)
Since its introduction in 2005 the GreenLight console has been upgraded from an initial 80watt system to 120watts and subsequently to 180watts, which is the system currently in use. GreenLightXPS exerts its therapeutic effect by utilising photoselective vaporisation of prostatic tissue as the shorter wavelength light is absorbed by oxyhaemoglobin. During the procedure, a high-power 532 nm wavelength laser (MoXy) fibre is passed through a specialised cystoscope which is continually cooled using a flow of saline to improve the fibre durability.
With regards to GreenLight XPS, NICE (3) guidance published in 2016 suggests that this procedure is at least as effective in treating ’low risk’ patients as conventional transurethral resection of the prostate (TURP) and can more often be done as a day-case procedure. It suggested a plausible scenario of 70% of treatments being done as day cases with the cost saving being up to £3.2 million (assuming a free console). However, there is currently insufficient evidence to support its routine use in high-risk patients. These include patients with increased risk of bleeding i.e. on anticoagulants, large prostates of more than 100mls and patients with prior urinary retention and catheterisation.
We present our experience of day surgery Greenlight XPS prostatectomy which is one of the areas where a major improvement in patient treatment can be applied. Since 2013, there was a reconfiguration of our service in order to enable this operation to be performed as day case. Specifically, a service was created where patients would be discharged with a catheter and re-attend our Urology Investigation Unit for a (trial without catheter) TWOC after 3-4 day post operatively.
Methods
A retrospective case analysis for all GreenLightXPS Prostatectomies performed over a 45-month period at Mid Yorkshire NHS trust was undertaken. Day surgery was defined as discharge on the day of surgery. The patient anaesthetic notes, operative notes, discharge summaries and readmission details were reviewed from electronic medical records for all the operations carried out between January 2013 and September 2016.
A detailed analysis of patient length of stay, readmissions and complications were made. We look at numbers/percentage of operations performed as day cases at yearly intervals. Also, we reviewed potential risk factors that may be associated with prolonged length of stay. These included age, American Society of Anaesthesiologists (ASA) score and preoperative retention/ catheterization. Statistical analysis with A/B testing, z score calculation and p value was used to evaluate if there is statistical significance between each risk factor and longer duration of stay.
All GreenLight XPS prostatectomies performed during this period were booked as day cases by default unless there were specific anaesthetic or social concerns. All cases were admitted to a dedicated day case unit. At the end of surgery the final decision for discharge was initially undertaken by the operating surgeon and anaesthetist as well as the day case unit nursing staff at a later stage in the recovery area.
Results
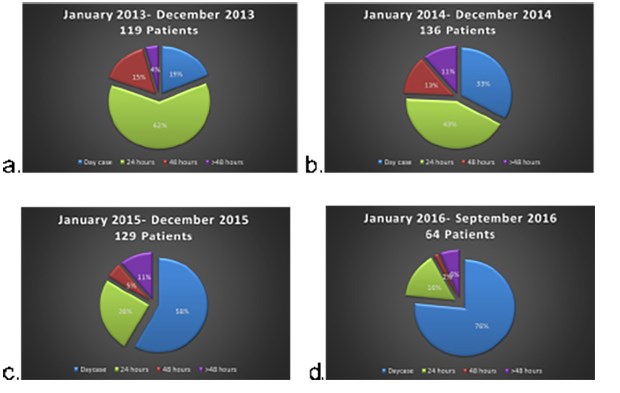
Between 2013 and 2016 we performed 448 GreenLight XPS prostatectomies. The average age was 73.7. All procedures were performed or supervised by one physician. The percentage of these procedures performed as day case per year steadily increased as our service matured to reach 76% (Figure 1).
Figure 1
Looking at risk factors than may lead to longer duration of stay we identified that overall there was statistical significance in patients with age >80, ASA equal or > 3 and prior retention/ catheterisation (Table 1).
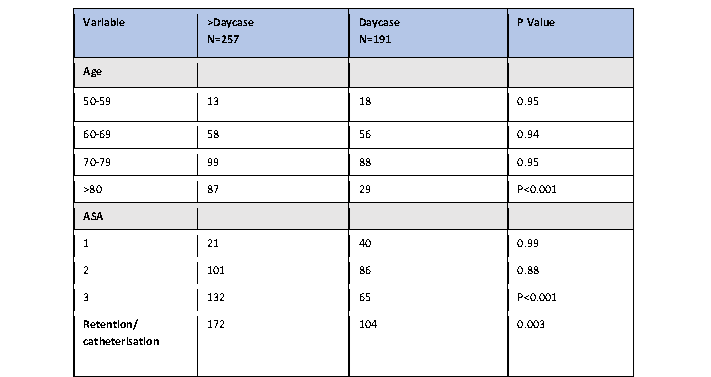
On looking on a yearly basis though it was apparent that the significance of age and ASA was obliterated at later years. Specifically the rate of day surgeries for the above 80 year olds was 10% in 2013, this increase gradually to 53% in 2016. Similarly for patients with ASA>/= 3 rate of day surgery was 7% in 2013 and increased to 62.5% in 2016. This dramatic improvement most likely correlates to the streamlining of the discharge process and the experience of the staff.
The readmission rate at 30 days was 6.8% for the day cases and 10.5% for the patients with longer stays. Although there is a lack of information regarding the readmission rates for elective urological surgery. Our results appear to be better than the rates reported for monopolar TURP reported in a recent study by Palmisano et al (2018) (4). In that study the readmission rate was 14.4%. The reasons for our patient readmissions is summarised below (table 2).
Finally, 95% of the "day case" patients had a successful TWOC. For the patients that had a longer stay the rate of successful TWOC was 92%. Results are outlined in table 3.
Discussion
British Day Surgery Association suggests that up to 75% of patients receiving treatment for bladder outflow obstruction can be managed on an ambulatory basis.(5) However most NHS trusts are far from achieving this target.
Emerging studies (6,7,8,9) have clearly demonstrated the possibility of early discharge of patients receiving treatment with the GreenLight XPS system across Europe due to lower rates of complications and morbidity seen with this technique. The most prominent of them is the GOLIATH, a randomised, multicentre, non-inferiority study. This study compared GreenLightXPS against standard monopolar TURP. Comparable outcomes were demonstrated across both modalities with regards to the International Prostate Symptom Score (IPSS), maximum urinary flow rate, and post-void residual urine at 6, 12 and 24 months. (6,7,8) No significant differences were observed when comparing complications, readmissions and need for further treatments. On looking however on the length of hospitalisation, length of catheterisation and time to stable health (defined as the ability to void without an indwelling catheter, a post-void residual urine of <100 mL) there was a clear advantage of the GreenLight XPS over TURP. These results were reflected in the UK subanalysis of the GOLIATH study (9), Indeed when comparing the two treatments, patients receiving treatment with the GreenLightXPS had a reduction in their hospital stay by one day and reduction in the duration of catheterisation. One of the downsides of the GOLIATH study was that patients had specific exclusion criteria. These included patients with large prostates >100g, patients with prior retention, age > 80 and patients with increased risk of bleeding diathesis or cardiovascular comorbidities.
Smaller studies (10,11) have since looked into the feasibility of performing day case GreenLight XPS prostatectomies in the high-risk group of patients, but still evidence is sparse. Namely West and Woo (2015) (10) found no difference in length of stay between GLL and TURP in high risk prostates stratified according to size. On the other hand, Chen et al (2013) (11) did identify a longer hospital stay and duration of catheterisation for patients receiving anticoagulants preoperatively.
Our study indeed comes to consolidate the results seen during the above studies with regards to efficacy of the GreenLightXPS and add more insight into the safety of the procedure in patients considered high risk. Indeed as our service matured and became more streamlined the majority of the patients (76%) were operated and discharged on the same day. Furthermore the rate of successful trials without catheter were comparable to that of standard TURPs. We did observe a longer length of stay in patients with ASA >3, age >80 and prior retention/catheterisation. However during the last two years of our data analysis the statistical significance in these groups of patients was no longer detected, thus these should not be considered as confounding factors to exclude an individual from having his operation as a day case. Indeed, we recommend that all cases should be pre-emptively considered for day surgery but with pre and post-operative individual circumstances and clinical condition taken into consideration before the final decision.
References
- Roehrborn CG. Benign prostatic hyperplasia: An overview. Rev Urol. 2005;7(Suppl 9):S3-S14.
- Tubaro A, de Nunzio C. Evolving techniques for surgical treatment of benign prostatic hyperplasia. EMJ Urol. 2015;3(2):119-22
- Nice guidance: GreenLight XPS for treating benign prostatic hyperplasia, Medical technologies guidance Published:14 June 2016
- Palmisano, F., Boeri, L., Fontana, M., Gallioli, A., De Lorenzis, E., Zanetti, S. P., … Montanari, E. (2018). Incidence and predictors of readmission within 30 days of transurethral resection of the prostate: a single center European experience. Scientific Reports, 8, 6575. http://doi.org/10.1038/s41598-018-25069-5
- British Association of Day Surgery BA of DS. BADS Directory of Procedures, 2011. Available at: https://www.aagbi. org/sites/default/files/Day%20Case%20 for%20web.pdf. Last accessed: 9 August 2016
- Bachmann A, Tubaro A,Barber N,d'Ancona F, Muir G, Witzsch U, Grimm MO, Benejam J, Stolzenburg JU, Riddick A, Pahernik S, Roelink H, Ameye F, Saussine C, Bruyère F, Loidl W, Larner T, Gogoi NK, Hindley R, Muschter R, Thorpe A, Shrotri N, Graham S, Hamann M, Miller K, Schostak M, Capitán C, Knispel H, Thomas JA. 180-W XPS GreenLight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European multicentre randomised trial--the GOLIATH study. Eur Urol. 2014;65(5):931-42
- Bachmann A, Tubaro A,Barber N,d'Ancona F, Muir G, Witzsch U, Grimm MO, Benejam J, Stolzenburg JU, Riddick A, Pahernik S, Roelink H, Ameye F, Saussine C, Bruyère F, Loidl W, Larner T, Gogoi NK, Hindley R, Muschter R, Thorpe A, Shrotri N, Graham S, Hamann M, Miller K, Schostak M, Capitán C, Knispel H, Thomas JA. A European multicenter randomized noninferiority trial comparing 180 W GreenLight XPS laser vaporization and transurethral resection of the prostate for the treatment of benign prostatic obstruction: 12-month results of the GOLIATH study. J Urol. 2015;193(2):570-8
- Thomas JA, Tubaro A,Barber N,d'Ancona F, Muir G, Witzsch U, Grimm MO, Benejam J, Stolzenburg JU, Riddick A, Pahernik S, Roelink H, Ameye F, Saussine C, Bruyère F, Loidl W, Larner T, Gogoi NK, Hindley R, Muschter R, Thorpe A, Shrotri N, Graham S, Hamann M, Miller K, Schostak M, Capitán C, Knispel H,Bachmann A. Functional results of a prospective randomized controlled study comparing GreenLight XPS to TURP demonstrate durable efficacy and safety at 24-months (GOLIATH): UK analysis. J Endourol. 2015;29(Suppl 1):A258
- Thomas JA, Zantek P, Bachmann A, Barber N, Muir G, Benejam J, Stoltenberg J-U, Bruyere F, Loidl W, Thorpe A, Morton R. Photoselective vaporization of the prostate by 180W GreenLight laser versus bipolar transurethral resection of the prostate: A subset analysis of the GOLIATH trial. J Urol. 2016;195(4):e513
- West KE, Woo HH. Does prostate size impact upon perioperative outcomes associated with photoselective vaporisation of the prostate using the 180-W lithium triborate laser. Urology Annals. 2015; 7(1):17-20
- Chen LJ, Mai H-X, Zhao L Qu N,Wang YL,Huang C, Li XC, Dong JK, Tang F, Chen B. Experience of treating high risk prostate hyperplasia patients with a HPS120 laser. BMC Urology. 2013; :64
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2018-journal/jods-284-december-2018/day-case-greenlight-xps-prostatectomy-a-single-centre-experience
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6050/284-michalis.pdf