Causes of failed discharges in day case Laparoscopic Inguinal Hernia Repair: Is there room for improvement? « Contents
Authors
Mehdi Raza Surgical Registrar, Maidstone and Tunbridge Wells NHS Trust
Aaron Kler Foundation Year Doctor, Maidstone and Tunbridge Wells NHS Trust
Ahmed Hamouda Upper GI Consultant, Maidstone and Tunbridge Wells NHS Trust
Correspondence author
Mehdi Raza Surgical Consultant, Darent Valley Hospital, Darenth Wood Road, Dartford, Kent A2 8DA
Email: mehdiraza@nhs.net
Keywords: Laparoscopic inguinal hernia surgery, transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP) repair, post-operative urinary retention (POUR).
Abstract
Introduction: Day care laparoscopic inguinal hernia surgery is now more commonly performed than a few years ago. Failure to safely discharge individuals the same day leads to pressure on hospital bed occupancy and adversely affects patient’s experience. This audit looks at the areas where we can potentially improve the patient journey through day case surgery.
Methods: This is an analysis of case records for 50 individuals booked for day case surgery that had to be admitted overnight after laparoscopic inguinal hernia surgery. A total of 287 procedures were done. Data for the individual, the type of surgery, anaesthesia and analgesia, post-operative management and causes of overnight stay were assessed.
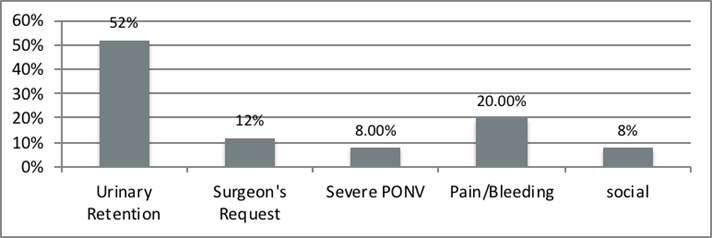
Results: The most common cause of overnight stay was found to be post-operative urinary retention. Not surprisingly, most were above the age of 60 but only three were known to have documented urinary problems in the past. Another factor was bilateral hernia surgery. Some patients were admitted for social reasons, post-operative nausea and vomiting, at the request of the surgeon and other uncommon causes. Nearly half of individuals were not administered local anaesthesia. 34 Individuals with bilateral hernia surgery stayed overnight on the ward.
Conclusion: The causes of failed discharges are multifactorial. Predictable delays in discharge for individuals above 60 years of age and those having bilateral surgery should probably have surgery early on the operating list. A protocol driven anaesthesia and pain control pathway should be followed. Social factors and fitness for laparoscopic surgery should be thoroughly assessed in the clinic to avoid unexpected admission.
Introduction
Inguinal hernia surgery is one of the most commonly performed procedures in the United Kingdom. Surgery is generally indicated in painful symptomatic hernias and to reduce the risk of future bowel obstruction or strangulation. It is perfectly reasonable to employ a ‘watchful wait’ policy in individuals that are asymptomatic though younger individuals are more frequently offered surgery than elderly asymptomatic ones. In a recent study it was suggested that 50% of watchful wait individuals crossed over to have surgery in a mean of 7 years. (1,2,3)
Open inguinal hernia repair with mesh, laparoscopic totally extra-peritoneal repair (TEP) or Trans-abdominal pre-peritoneal repair (TAPP) are the options of treatment. The type of approach depends on surgeons’ experience, patient choice, service provisions in the local hospital, technical and anaesthetic considerations. Laparoscopic surgery has become a standard of treatment for inguinal hernias. From the chronic pain perspective, earlier review of literature that compared laparoscopic with open surgery showed that laparoscopic inguinal hernia surgery (LIHR) is more advantageous. Advantages are generally lesser pain, quicker recovery, earlier return to work and patient satisfaction compared to open surgery. (4)
Due to pressure on elective surgery and the need to ring fence beds in acute wards, there is a growing need to perform more operations as day case procedures. Day case units need to be fully functional independent units with dedicated day care ward staff, doctors, surgeons and anaesthetists. The Royal College of Surgeons and British Association of Day Surgery (BADS) have provided guidelines on managing patients having day case surgery. (5)
Most commonly referrals are received from the local general practitioner. A thorough assessment of the history and fitness for surgery is carried out in the clinic. As our general population is more obese and many are above the age of 60, it is important to be aware of their social history. Appropriate provisions must be made for them at home or be admitted overnight if they live alone or have special needs. In our practice, a referral to the pre-assessment clinic is made on the day of the surgical review. Our anaesthetists review the medical records for all individuals that are referred by the pre-assessment nurse. Individuals with ASA III (American Society of Anaesthesiologists) or ASA IV and high BMI (body mass index) of above 42 are not fit for day case surgery. They are booked on our main theatre lists in Maidstone Hospital.
Methods
We perform most of our elective inguinal hernias as day case procedures. The aim of the audit was to ascertain how many patients stayed overnight despite being deemed fit for a day case procedure.
This is a retrospective audit of all patients from Jan 2014 to August 2015 receiving elective laparoscopic inguinal hernia repair that stayed past midnight on the day of surgery. 287 laparoscopic inguinal hernias were performed. 50 patients stayed overnight post operatively. This was due to numerous factors. The most common cause being post-operative urinary retention (POUR). Normally the urinary bladder has a capacity of a volume of 400-600ml but POUR can occur with even a residual post voiding volume of 150ml in the bladder 6. POUR is defined as the inability to spontaneously pass urine requiring urethral catheterisation. The decision to catheterise is nurse led on the day case ward. This is based on the inability to pass urine for more than 6 - 8 hours postoperatively and the use of a portable bladder scanner to check the pre and post micturition bladder volume.
We have a dedicated day surgical unit in Tunbridge Wells Hospital. We have our planned elective lists in Maidstone Hospital. The day case unit has its own dedicated ward called Short Stay Unit with its own nursing, anaesthetic, and surgical staff. They also have an adjacent theatre recovery area. The patients have a nurse led discharge and are assessed for pain, ability to mobilise, oral intake, ability to pass urine and if required, have their venous thromboprophylaxis injection. The discharge letter is done by the operating surgeon or a junior doctor with the necessary postoperative advice and medications. Patients are provided with literature with a direct access phone number for the ward during opening hours and are asked to attend the Accident and Emergency Unit after the day unit is closed.
Coding of patient procedure (T20 and Y75.2) was used to identify all the cases that had laparoscopic inguinal hernia surgery. The services of our medical records clerk helped us collect all the patients’ notes. Out of 287 individuals having laparoscopic inguinal hernia surgery, 50 patients met the inclusion criteria with an age range between 25 - 85. All the data was compiled into an excel sheet.
The patient data collected included age, previous medical history, type of surgical procedure, type of repair/mesh, local anaesthetic given, anaesthesia used, analgesics, antibiotics, days stayed in hospital and reason for overnight stay.
The Royal College of Surgeons guidelines were used to compare with our results. (5)
Results
There have been numerous papers that have evaluated POUR after inguinal hernia repair. (7,8,9,10) In this retrospective observational study we have looked into a wide range of causes of failed same day discharge.
We are seeing more patients above the age of 60 having day case surgery procedures. As far as age of our cohort of patients is concerned, 27 individuals out of the 50 overnight ward admissions were above 60 years of age. Despite not anticipating any risk factors of failed discharge when they were booked in for day care surgery, 15 of above 60 year old individuals had stayed overnight with POUR. Interestingly, only 3 were known to have benign prostatic hypertrophy or urethral surgical intervention in the past.
19 out of 50 patients having bilateral LIHR were above 60 years age. There were various reasons for failed discharge. The most common reason after POUR was social reasons, postoperative nausea and vomiting (PONV) and surgeon’s request. We were not able to look into the exact social causes that were specific to the individuals.
We performed bilateral LIHR on 34 individuals that failed to be treated as day case patients. It was observed that all patients had a combination of fentanyl, paracetamol, nonsteroidal anti-inflammatory agents (NSAIDS) intraoperatively by the anaesthetists. 19 of the bilateral LIHR were, in addition to these painkillers, administered morphine intraoperatively or in the anaesthetic recovery area. A prolonged procedure in bilateral cases and difficulty in controlling pain might have resulted in an overnight stay. Unfortunately, we did not assess operating times for every procedure.
Muscle relaxation was either rocuronium or atracurium in these patients.
All of our patients had a standard LIHR with a Prolene mesh repair that was secured in the midline with tacks. These were absorbable and non-absorbable according to individual choice of the surgeon.
There was documentary evidence of local anaesthesia infiltration in 26 patients. The remaining 24 did not receive any local anaesthesia.
The Royal College of Surgeons guidelines for inguinal hernia surgery suggest avoiding the use of antibiotics as prophylaxis against mesh infection due to the lack of evidence to support it. Our study showed that most of our patients (45) out of 50 were prescribed antibiotics.5
Patient and surgery data
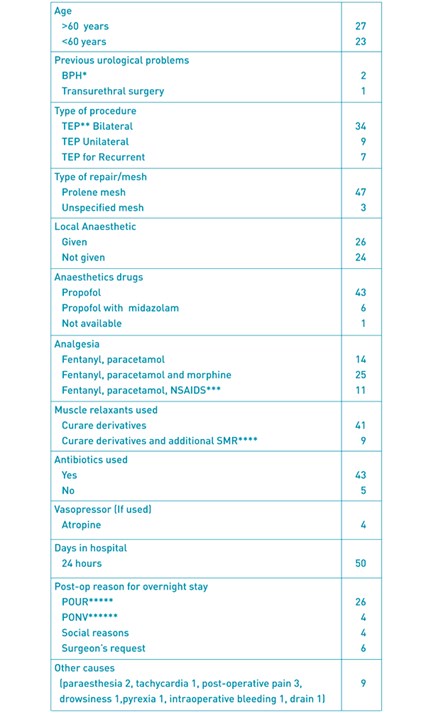
PH benign prostatic hypertrophy, **Totally extraperitoneal, ***Nonsteroidal anti-inflammtory drugs, ****skeletal muscle relaxation, *****post-operative urinary retention,******Post-operative nausea and vomiting
Figure 1: Bar chart for causes of overnight stay with relative frequencies
The audit was presented in our clinical governance meeting on the 14 January 2016.
The results were presented in the Association of Surgeons in Training meeting as a poster in 2016.
Discussion
Laparoscopic inguinal hernia surgery is being carried out as a day case procedure in the majority of regions in the United Kingdom and around the world. Assessment of fitness for day case surgery depends on numerous factors including surgical, medical, anaesthetic and social factors.
The British Association of Day Surgery recommends that 80% of inguinal hernia surgery is carried out as a day case operation11. Although all of our 287 patients were booked for a day case procedure, more than 80% were successfully treated and discharged the same day. There is a requirement for our day surgery unit to work closely with the primary care teams to avoid difficulty in postoperative rehabilitation. The individual is provided with a helpline number with 24 hours access after discharge.11 Our data does not take into account the failed discharges that were either admitted to accident and emergency or the acute ward after leaving the day unit. Many units that provide 24 hour access helplines advise callers to attend the accident and emergency department if the day case ward has closed for the day.
The POUR failed discharges of 9% are within the accepted figures of 1 to 22%81213. Many studies looked into the cause of acute urinary retention in laparoscopic inguinal hernia repairs. It has been proposed that excessive narcotic use over 6.8 mg of morphine or over could predispose to POUR. This was in a study of 28 individuals with POUR from a total of 346 having the surgery9. The study size we believe was not significant enough to provide conclusive evidence against the optimal dose of morphine.
Another study reviewed many variables to help predict the individuals with POUR. This was a retrospective review of cases that identified age above 60 years, history of previous BPH and total anaesthetic time to be risk factors for POUR on univariate and multivariate analyses. 12 individuals had benign prostatic hypertrophy, 6 with urine voiding problems in the past and 4 with prostatic cancer. Interestingly, 5 patients were discharged home without having passed urine and were admitted the next day for urinary catheterisation in this review of data.13
The use of intravenous fluid therapy intraoperatively and post operatively of one litre or above has shown an increase in risk of POUR. The confounding factor with intravenous fluid therapy was administration of opioid analgesia postoperatively.14 The bladder stretch from intravenous therapy was thought to reduce detrusor contraction. It is also hypothesized that surgery in close proximity to the bladder in laparoscopic surgery affects bladder activity. Koch et al mentioned in his study that the use of mesh fixation devices whether absorbable or non-absorbable increase the need of intraoperative narcotic analgesia and POUR. Eliminating the use of fixation devices were shown to reduce pain killer requirements and risk of POUR. Mesh fixation devices were used in all of our patients.15
A centre approached the issue of POUR with various interventions like prescribing an alpha 1 blocker preoperatively and post operatively. This has shown a reduction of POUR in high risk patients with lower urinary tract symptoms. The criticism is that this intervention was on open surgical procedures without a mesh (Bassini and Darn repair). We know laparoscopic surgery carries a higher risk of POUR compared to open surgery.16 In another centre it was shown that prevalence of lower urinary tract symptoms increases per decade increase in age and an alpha blocker can prevent POUR.17
Recently, a review of the pathophysiology, risks, complications and treatment of POUR were discussed with a thorough assessment of treatment options from urethral bladder catheterisation to prostatic surgery. It was stressed that POUR is a surgical emergency that can cause acute renal failure and postoperative diuresis.6
Optimisation of pain relief intraoperatively and post operatively can improve outcomes and early discharge. As day case surgery is evolving, medications are being used that have lesser adverse outcomes. As an example, it has been shown that remifentanil seems to have shown lesser adverse events for the day case patients than fentanil.18 Similarly Infiltration of local anaesthetic prior to starting the procedure has been shown to reduce the requirements of prolonged anaesthesia, intravenous analgesia, post-operative opioid use and hence early mobilisation.19
One interesting aspect that could improve day case experience is the continuity of care in healthcare. This is a concept of seeing the same named staff nurse and surgeon peri-operatively. This enhances the patient experience, confidence and understanding of the pathway by the patient and the healthcare staff. High patient turnover and staff shortages can hinder this but could be gradually implemented at certain designated levels like nursing and doctors.20
Better continuity of care and understanding of the postoperative pathway could lead to lesser overnight stay. This can better help avoid the unexpected admissions overnight for social reasons and a better understanding of the personal circumstances of the individual.
Unfortunately there are always going to be post-operative factors that will prevent early discharge. We admitted 9 individuals with various minor nonspecific postoperative complications like transient paraesthesia, presence of a drain, drowsiness, intra-operative bleeding, nonspecific tachycardia, post-operative pain and post-operative pyrexia.
We also had 6 unavoidable admissions on the operating surgeon’s request. These were due to technical difficulties in surgery and due to overrunning operating lists.
Numerous centres have gone one step forward and performed ‘one stop shop’ LIHR. The individual is seen, assessed anaesthetically, operated upon and discharged the same day. Although this would have huge implications on the organisation of the patient journey in a busy and high volume unit in the National Health Service, this could be a useful option to reduce waiting lists by choosing the more suitable patients for LIHR.21,22
Although many studies have looked at reasons for POUR but there is a lack of evidence looking into all general causes of failed discharge. This audit has its limitations as it was a retrospective review of our quality outcomes however, we have looked into all causes of failed discharge. It is the author’s experience that many individuals are booked as day case LIHR by doctors not experienced in LIHR. Additionally, some technical factors like previous surgery are not absolute contraindications but affect operating time and rarely may warrant overnight observation.
Slight variation in clinical practice exists amongst surgeons. On the day of the surgery an open repair might be converted to LIHR because of patient choice or incidental finding of bilateral hernias. Unfortunately, despite evolving practice, some individuals are still not given the options and are only booked for open surgery.
Article continues after ad.
Conclusions
This audit highlights the complexities of day care surgery and multifactorial issues surrounding optimising post-operative care. Factors like age above 60 years, bilateral LIHR and pain management need to be kept in mind in booking the surgery. Better awareness of the social circumstances and close work up with pre-assessment and clinical staff is required to avoid unnecessary post-operative failed discharges. A simple checklist for assessing the suitability for LIHR could guide junior doctors in booking cases appropriately in clinic.
References
- The Herniasurge Group, Simons MP, Smietanski M, et al. International guidelines for groin hernia management. Hernia. 2018.
- Gong W, Li J. Operation versus watchful waiting in asymptomatic or minimally symptomatic inguinal hernias: The meta-analysis results of randomized controlled trials. Int J Surg. 2018. doi:10.1016/j.ijsu.2018.02.030
- O’Dwyer PJ, Norrie J, Alani A, Walker A, Duffy F, Horgan P. Observation or operation for patients with an asymptomatic inguinal hernia: A randomized clinical trial. Ann Surg. 2006. doi:10.1097/01.sla.0000217637.69699.ef
- Kuhry E, Van Veen RN, Langeveld HR, Steyerberg EW, Jeekel J, Bonjer HJ. Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc Other Interv Tech. 2007. doi:10.1007/s00464-006-0167-4
- Sanders, David L KM. Commissioning guide: Groin hernia Commissioning guide 2013. Br Hernia Soc Groin Hernia Guidel. 2019;(October 2013):58.
- Kowalik U, Plante MK. Urinary Retention in Surgical Patients. Surg Clin North Am. 2016. doi:10.1016/j.suc.2016.02.004
- Sivasankaran M V, Pham T, Divino CM. Incidence and risk factors for urinary retention following laparoscopic inguinal hernia repair. Am J Surg. 2014. doi:10.1016/j.amjsurg.2013.06.005 [doi]
- Sivasankaran M V., Pham T, Divino CM, et al. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2013. doi:10.1007/s00464-013-3119-9
- Patel JA, Kaufman AS, Howard RS, Rodriguez CJ, Jessie EM. Risk factors for urinary retention after laparoscopic inguinal hernia repairs. Surg Endosc. 2015. doi:10.1007/s00464-014-4039-z
- Hudak KE, Frelich MJ, Rettenmaier CR, et al. Surgery duration predicts urinary retention after inguinal herniorrhaphy: a single institution review. Surg Endosc Other Interv Tech. 2015. doi:10.1007/s00464-015-4068-2
- Verma R, Alladi R, Jackson L, Al E. Day case and short stay surgery: 2. Anaesthesia. 2011. doi:10.1111/j.1365-2044.2011.06651.x
- Lau H, Patil NG, Yuen WK, Lee F. Urinary retention following endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc Other Interv Tech. 2002. doi:10.1007/s00464-001-8292-6
- Sivasankaran M V., Pham T, Divino CM. Incidence and risk factors for urinary retention following laparoscopic inguinal hernia repair. Am J Surg. 2014. doi:10.1016/j.amjsurg.2013.06.005
- Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2006. doi:S0002-9610(05)00921-9 [pii]
- Koch C a, Greenlee SM, Larson DR, Harrington JR, Farley DR. Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. JSLS. 2006.
- Mohammadi-Fallah M, Hamedanchi S, Tayyebi-Azar A. Preventive effect of tamsulosin on postoperative urinary retention. Korean J Urol. 2012. doi:10.4111/kju.2012.53.6.419
- Shaw MK, Pahari H. The role of peri-operative use of alpha-blocker in preventing lower urinary tract symptoms in high risk patients of urinary retention undergoing inguinal hernia repair in males above 50 years. J Indian Med Assoc. 2014.
- Palumbo P, Usai S, Amatucci C, et al. Inguinal hernia repair in day surgery: The role of MAC (Monitored Anesthesia Care) with remifentanil. G di Chir. 2017. doi:10.11138/gchir/2017.38.6.273
- Radwan RW, Gardner A, Jayamanne H, Stephenson BM. Benefits of pre-emptive analgesia by local infiltration at day-case general anaesthetic open inguinal hernioplasty. Ann R Coll Surg Engl. 2018. doi:https://dx.doi.org/10.1308/rcsann.2018.0059
- Suominen T, Turtiainen AM, Puukka P, Leino-Kilpi H. Continuity of care in day surgical care - perspective of patients. Scand J Caring Sci. 2014. doi:10.1111/scs.12099
- Jutte EH, Cense HA, Dur AHM, Hunfeld MAJM, Cramer B, Breederveld RS. A pilot study for one-stop endoscopic total extraperitoneal inguinal hernia repair. Surg Endosc Other Interv Tech. 2010. doi:10.1007/s00464-010-1035-9
- Voorbrood CEH, Burgmans JPJ, Clevers GJ, et al. One-stop endoscopic hernia surgery: efficient and satisfactory. Hernia. 2015. doi:10.1007/s10029-013-1151-2
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6048/284-raza.pdf