Tonsillectomy: Reducing Length of Stay and Increasing Day Surgery Rate « Contents
Authors
John Guirguis Anatomy Demonstrator/Surgical Trust Doctor
Jonathan Hobson Consultant ENT Surgeon
Department of Otolaryngology, University Hospital of South Manchester
Contact details:
John Guirguis Newcastle University, Framlington Place NE2 4HH
Email: johnguirguis@doctors.org.uk
Keywords: Tonsillectomy, Adenotonsillectomy, Day, Day case, Surgery, Rate
Abstract
Aims: 85% of tonsillectomies should be completed as day case operations. This rate was 33% in the University Hospital of South Manchester (UHSM) in April 2015.This study will focus on identifying factors that could be contributing to this low rate, in order to decrease length of stay following tonsillectomy.
Methods: Tonsillectomies were accessed from April 2015, October 2014 and April 2014, with patient details recorded. The case notes were then requested and a pro forma made to include a variety of information regarding the patient and operation.
Results: A total of 62 patients had tonsillectomies completed across the 3 months of the study. 8 were not included. The day case rate was 31% in April 2015, 50% in October 2014, and 65% in April 2014. In total, 27 patients were managed as day cases (50%).
Patients under the age of 6 had a low day case rate of 29%. 68% of bilateral tonsillectomies were completed as day cases, in contrast to 21% of adenotonsillectomies.
64% of operations done in the morning were completed as day cases, in comparison to 22% performed in the afternoon. Operations done as day-case averaged 25.6 minutes, while overnight stay averaged 31.4 minutes. 10% of patients with sleep apnoea, and 20% of patients with complications, were managed as day cases.
Conclusion: The day case rate of tonsillectomies performed at UHSM are significantly below the required standards of 85%. Several contributing factors were identified: younger patients, afternoon operations, type of procedure (adeno-tonsillectomy), prolonged duration of surgery, sleep apnoea, and complications.
Introduction
Day surgery is best described as 'the admission of selected patients to hospital for a planned surgical procedure, returning home on the same day' (1).
The British Association of Day Surgery (BADS) has produced a Directory of Procedures recommended to be done as day-case operations, with over 200 operations covered (4). The desired day case rates of each procedure are also included - with tonsillectomies given a target rate of 85% (2,4). The figure below outlines the benefits of day surgery over an inpatient stay (3).
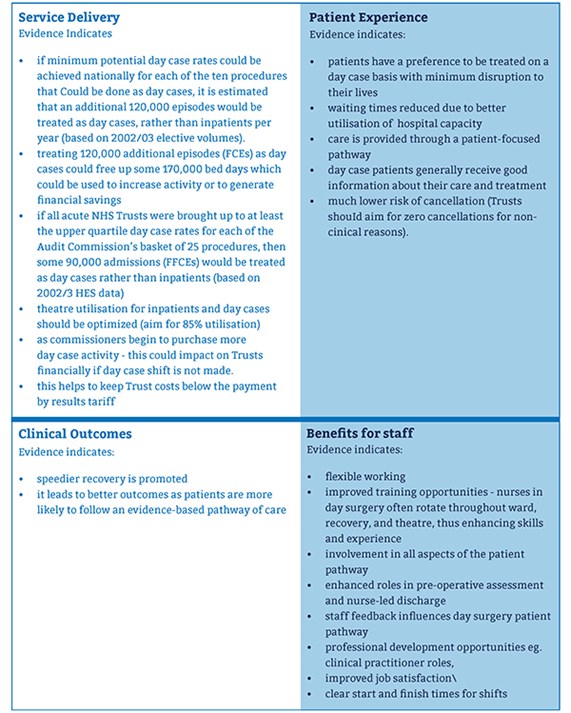
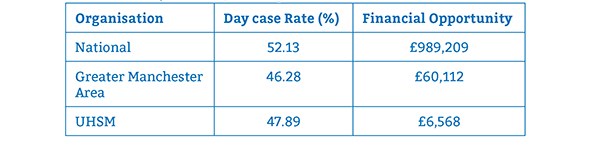
Table 1 shows the average day case rate of tonsillectomy across the UK, the Greater Manchester Area, and UHSM, over the year 2014/2015. As shown by the figures, each organisation is well below the 85% target rate, proving there is room for improvement. The financial opportunity indicates how much money could be saved if the trust(s) achieved a day case rate in line with the percentile for the top quarter of the year. If 85% was achieved, potentially even more could be saved for each organisation. £11,206 could be saved at UHSM if rates of 90% were achieved (2).
TABLE 1: The average day case rate of tonsillectomy across the Nation, the Greater Manchester Area, and
UHSM, over the year 2014/2015.
Tonsillectomy is one of the most common operations completed in the UK. Although the number of these procedures performed has decreased significantly since the 1930s - where 100,000 tonsillectomies were performed on school children, the incidence has started to rise again since the 1990s (5). In 2012, around 31,000 tonsillectomies were performed; 18,000 of these were done on children. This resulted in a cost of £51m across England. There is a lot of variation in the numbers across the UK (6). In the UK, there are more than 35 million work or school days lost annually (5).
The objective of this study is to look into decreasing the length of stay for patients who undergo tonsillectomy. Tonsillectomy should be done as a day case operation, meaning the patient should be discharged home on the same day of the surgery. The British Association of Day Surgery has set a target of 85% of tonsillectomies to be completed in this manner4. The day case rates in the University Hospital of South Manchester (UHSM) have dropped from 60% in April 2014 to 33% in April 2015.
To ascertain why this is the case, 3 separate months ranging from April 2014 to April 2015 will be looked at, focusing on how many tonsillectomies were completed and how many were managed as day case operations. This will allow clarification of these proportions and investigate why the rate has been falling.
Methods
Permission was given to access all the operations completed in ENT theatres on the computer. The procedures completed in the three months of the study were looked at; recording each tonsillectomy done, the date of the operation, and the name and hospital number of the patient receiving the surgery. Information was also collected regarding the surgeon and the duration of the surgery.
The search returned a total of 62 patients who underwent tonsillectomies over the three months - 16 patients from April 2015, 28 from October 2014, and 18 from April 2014. After recording the basic information of each operation, each individual patient was looked at in more detail to find out if the surgery was completed as a day case, and if any reasons were provided in the event of an inpatient stay.
In order to retrieve the patient cases, ENT secretaries kindly requested the data needed. The patient notes were then accessed and worked through one month at a time, recording a variety of fields relevant to the study. This information was maintained on a spreadsheet accordingly. The data kept note of is as follows:
- Demographics: age, gender, weight (kg), BMI
- First half of postcode
- Procedure (adeno- or tonsillectomy), any additional procedures
- Surgeon and duration of operation
- Details of operation: date, day, time
- Details of discharge: date, time
- Problems during/after operation (e.g. failure to pass urine)
- Relevant PMH
- Day case?
The information was analysed in each field in order to find out whether there was any association in a particular field with the procedure being completed as a day case. Each patient case was also analysed in detail to see if there was a specific reason for an overnight stay.
Some patient notes could not be acquired as they were being used for other reasons at the time. After recording the information required for each patient, 8 patients had still not been looked at - 3 for April 2015, 4 for October 2014, and 1 for April 2014. Unfortunately, we were unable to acquire the remaining patient cases over the duration of the study.
Descriptive statistics and demographics were reported as figures and percentages. Categorical variables were compared using Fisher's Exact Test with two-sided probability and Mann-Whitney U Test as appropriate, using Past3 (Palaeontologica Electronica, Oslo) statistical software for analysis. Significance was set at P<=0.05.
This method had both advantages and disadvantages. The advantages include:
- The hospital information required was achieved in reasonable time due to the electronic database of operations, and the kind help of the ENT secretaries.
- Low cost as data was collected within the hospital.
- The patient cases are well organised and allowed the information to be collected following the same pattern.
The disadvantages are:
- 8 patient details are missing for the report.
- Lack of documentation in some case notes.
Results
A total of 62 patients have had tonsillectomies over the 3 months of the study - 16 in April 2014, 28 in October 2014, and 18 in April 2014. Data is missing for 8 of the patients, therefore, the results will focus on 54 patients with the remaining 8 to be added at a later date.
As discussed earlier, a target of 85% of tonsillectomies should be completed as day cases. UHSM provided details of the falling day case rate at the hospital: 33% in April 2015, 50% in October 2014, and 60% in April 2014. Table 2 represents the number and percentage of procedures done as day cases. In total, 27 of the 54 operations were completed as day cases - 50%.
TABLE 2: Day surgery rates across the three months included in the study. Shown as numbers and percentages.
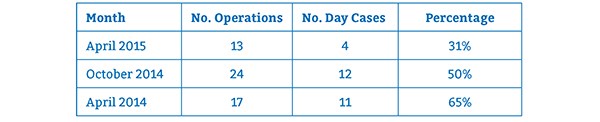
Table 3 considers the patient's age in relation to the day case rate. It demonstrates a high proportion of patients under the age of 6 were admitted and required inpatient stay. It is important to state that within the trust, day case operations are unsuitable for patients under 15kg in weight, or with BMI <5th or >95th percentiles. 4 patients from this age group were under 15kg and therefore unsuitable for day surgery. However, 1 was managed as a day case and went home the same day.
The day case rate increased at the 6-12-year-old group, but drops from 78% to 38% at the 12-18-year-old group. If considering all of the paediatric patients together (those under the age of 18), the day case rate was 42%, lower than the figure of 69% for adults.
TABLE 3: Day surgery rates across the three months included in the study. Shown as
numbers and percentages.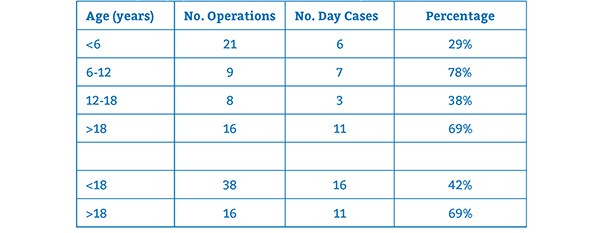
35 of the 54 tonsillectomies were performed on females, which resulted in 20 being completed as day cases (57%). From the remaining procedures done on males, 7 were day cases - a percentage of 37%.
Data was collected on the BMI and weight of each patient; however, this will not be discussed in this study. There was no connection between the postcode of the patient and day case rate at UHSM. Across each postcode area recorded: Manchester, Cheshire, Stockport, Warrington; there was a mixture of tonsillectomies completed as day cases and requiring inpatient stay.
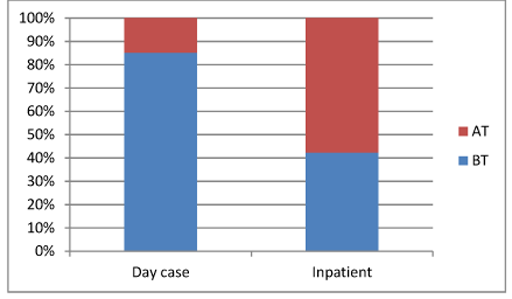
The results show that out of the 54 tonsillectomies performed, 34 were bilateral tonsillectomies (BT), 19 were adenotonsillectomies (AT), and one unilateral tonsillectomy was performed on the left side. Adenotonsillectomy is the same as a tonsillectomy with the addition of the adenoids (pharyngeal tonsils) extracted. Adenoidectomy and tonsillectomy are some of the most frequently performed operations suitable for day surgery, and are completed together in around one third of patients4,5.
Of the 34 bilateral tonsillectomies, 23 were completed as day cases - a percentage of 68%; however, just 4 adenotonsillectomies - 21% - were managed in this way. These variables were compared using Fisher's Exact Test with two-sided probability. The results represent a significant difference, with P value 0.002 (significance P<=0.05). The left tonsillectomy required admission, but this may have been due to a neck lump excision on the right side being completed at the same time.
Figure 2 shows the management of the two procedures weighed up against each other. The day case rate of BTs stands out against ATs.
FIGURE 2: The outcome of bilateral tonsillectomies (BT) against adenotonsillectomies (AT).
This shows the proportion of both operations done as day cases against the proportion that required
inpatient stay.
In some cases, additional procedures were also performed during the same anaesthetic for the tonsillectomy. These ranged from grommets to various endoscopies. 11 tonsillectomies had an extra procedure done. Only 3 of these were completed as day cases (27%). These patients were therefore more likely to be kept overnight.
It was difficult to draw any conclusions on day surgery rates relating to the operating surgeon. The numbers being discussed for each surgeon were generally too few to be reliable. The majority of operation notes state for the patient to go home the same day if well.
The duration of operation for patients managed as day cases and those managed as inpatients was considered. The average duration for day case operations was 25.58 minutes, while operations that resulted in overnight stay averaged 31.44 minutes. Every operation performed was listed and ranked within the two groups and compared using a Mann-Whitney U Test. This provided a z score of -0.99 and a P value of 0.32 (significance P<=0.05), showing no significant difference in day case rate according to the operation time.
In order to find out if the timing of the operation affected the day case rate, the day of the procedure was looked at, in addition to whether it was performed in the morning or afternoon.
8 tonsillectomies were done on Monday, 3 on Tuesday, 12 on Wednesday, 23 on Thursday, and 8 on Friday. No significant trend was found to the results.
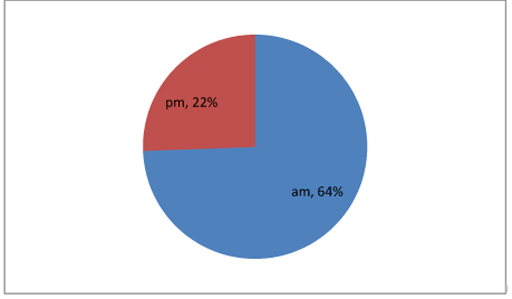
Focusing on when the operation was done, the number of procedures done in the morning and afternoon were counted before calculating what proportion of them were completed as day cases.
36 tonsillectomies were done in the morning, with 23 of them managed as day cases - 64%. On the other hand, just 4 out of 18 tonsillectomies done in the afternoon were managed as day cases - 22%. Using Fisher's Exact Test, these figures represent a P value of 0.008 (significance P<=0.05), confirming a significant difference in day case rates depending on the time of day. Figure 3 displays these percentages in a pie chart.
FIGURE 3: Day surgery rate in relation to the timing of the operation - morning against afternoon.
As mentioned previously, the trust will consider admitting patients who undergo tonsillectomies with a background of sleep apnoea. To see if this was the case, the management of each patient with a history of sleep apnoea was looked at, excluding patients with sleep disordered breathing. The results showed that 10 patients had a history of sleep apnoea, and just one of these was managed as a day case - 10%.
2 patients had a history of heart problems - 1 with an AVSD associated with Down's Syndrome, and the other with CHD and a bicuspid aortic valve. Both of these patients were kept overnight.
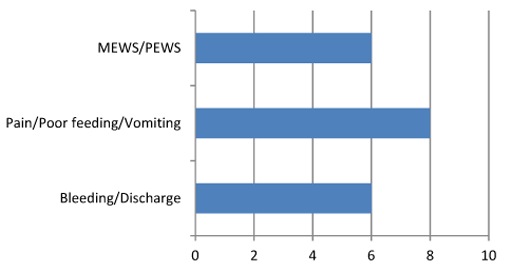
Any problems experienced by the patients were well documented by the nurses, including both surgical and non-surgical problems. Non-surgical problems recorded included any bleeding or discharge, refusal to take in fluids or food, nausea and vomiting, excessive pain, and any changes to the patient's MEWS/PEWS score.
20 patients had one or more of these problems documented with 4 going home on the day of the operation - 20%. Figure 4 looks at the surgical problems encountered.
FIGURE 4: Post-op complications. 4 of these 20 patients went home the same day.
7 patients presented at later dates due to complications - 13%. 5 of these were managed as day cases. Of the 7 patients, 2 were admitted within 24 hours of the operation. 4 patients were admitted due to post-op bleeding (7.4%), with 2 being taken to theatre for surgical arrest of the bleeding (3.7%). The remaining 3 patients suffered post-operative infections causing a sore throat, fever, and vomiting. These patients were managed with antibiotics.
As shown earlier, the most recent month of April 2015 had a day case rate of 31%. We aim to determine if the factors identified above that contribute to a low day case rate, were more prominent within this month. 13 tonsillectomies were done in April 2015, with 4 completed as day cases.
4 were performed on patients under the age of 6, all being managed as inpatients; and 2 in the 12-18-year-old bracket, with both being staying overnight. 5 of the 13 operations were adenotonsillectomies, all resulting in inpatient stay. 3 patients also had additional procedures done, resulting in admission for the night.
The average duration of the operation over the month was 28.69 minutes - dropping to 26 minutes for the day cases, but rising to 29.88 for the inpatients. 6 out of 7 of the tonsillectomies done in the afternoon resulted in an overnight stay, whereas out of the 6 procedures done in the morning, half were managed as day cases.
Out of the 13 patients, 6 had 'problems' documented by nurses, and 3 had a history of sleep apnoea. All of these patients were managed as day cases. No patients were readmitted in this month due to any complications.
Discussion
The British Association of Day Surgery has identified a target of 85% of tonsillectomies to be completed as day cases (4). In April 2015, UHSM completed 33% of tonsillectomies as day cases. The results reflect reasons of why some procedures were not completed as day cases and areas in which the day case rate could be improved.
The age of the patient represents one of these areas. 29% of tonsillectomies done on children under the age of 6 were completed as day cases, much lower than the percentages shown for the other age groups. Identifying these patients and planning accordingly could increase the number of procedures done as a day case.
There is a significant difference in the day case rates regarding the type of operation done. 68% of patients who underwent bilateral tonsillectomies were discharged the same day, compared to 21% for those who had adenotonsillectomies. Both of these figures are short of the target, however, with adenotonsillectomies, there is huge room for improvement and by identifying patients undergoing this procedure, better planning can be made in order to improve the day case rate.
Additional procedures done during the same anaesthetic as the tonsillectomy also result in a larger proportion of inpatient stays for patients. Focusing on these patients and providing appropriate care may also help improve the day case rate.
Another factor influencing the day case rate is the time of the operation. The results show that tonsillectomies done in the morning are much more likely to be completed as day cases than tonsillectomies done in the afternoon. The corresponding day case rates are 64% and 22% respectively. By planning ahead and aiming to complete more tonsillectomies in the morning, the day case rate could be improved.
The study does not take into account each individual surgeon's rate of day case surgery, as the number of cases carried out by each surgeon are too small to provide any significant conclusion. Therefore, a study looking into this further may be needed.
For the 10 patients with a history sleep apnoea, just 1 managed to go home the same day of the operation. The guidelines are not clear on how these patients should be managed, but this could be looked at further in order to increase day case rates.
One study looked into the safety of day case tonsillectomy in patients with sleep apnoea (7). In 165 patients with sleep apnoea and no other co-morbidities, there were 37 complications. These were grouped into surgical (bleeding), medical (dropped saturations) and social (pain and poor feeding). Surgical and social rates were similar to those in patients without sleep apnoea. 10 patients had complications specific to sleep apnoea (desaturations) - 6.1%.
This study concluded that patients with sleep apnoea and no other co-morbidities can be safely managed as day cases. It suggests the patient should be monitored for desaturations for 6 hours postoperatively before being discharged the same day7. However, further studies within UHSM looking into sleep apnoea are required before creating safe Trust guidelines.
Patients with documented problems while in recovery and following the surgery were more likely to be kept in as inpatients. One study shows that patients undergoing day case surgery had better sleep, oral intake, and less pain during the first postoperative night (8). However, this study also indicates that the patients kept overnight would have found day case surgery less tolerable. Following a questionnaire 2 weeks post-op, 92% of patients revealed they preferred tonsillectomy completed as a day case8.
Social and non-surgical factors for the reduction in day case rates were not investigated in this study as the case notes did not provide this information. A separate study into these reasons may be beneficial to further improve the day case rate.
The results of this study showed no significant difference in relation to the duration of the surgery. It is difficult to discuss how to improve the day case rates in patients with documented problems, as it is subjective. However, with reassurance and good quality care, the day case rate could possibly be improved further.
Many papers have looked into the safety of tonsillectomies being performed as day cases and encouraged it due to complication and readmission rates being low in general (9). Postoperative haemorrhage rates have ranged from 0.14 to 8.5% in a variety of papers (10). 7.4% of the patients in this study were readmitted due to haemorrhage.
Conclusions
Day surgery has several benefits. The majority of patients have positive experiences as they spend the night at home in a more comfortable environment, while staff also benefit from the clear pathway in place. Day surgery provides healthcare with the opportunity to save money in bed occupancy and nursing care. At UHSM, £6,568 could be saved by increasing the day case rate to 75%, with potentially more being saved if the target of 85% was met. Day surgery is a safe way to provide high quality care in the most cost-efficient way, improving clinical outcomes.
This study showed that we are significantly below the required standards, and day-case rates have been falling over the past few years. Several factors that could well be contributing to this were identified. Those factors are as follows:
- Age of the patient
- Time of the operation
- Type of procedure
- Additional procedures done
- Surgeon performing the surgery
- Background of sleep apnoea
- Complications
Each factor requires further investigation using a larger number of patients to identify ways in improving each factor separately. By focusing on each factor, it may be possible to increase the day case rate and achieve the 85% target in the future.
References
- NHS Institute for Innovation and Improvement. Treating Day Surgery as the Norm. http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/day_surgery_-_treat_day_surgery_as_the_norm.html (accessed 10/06/2015)
- NHS Institute for Innovation and Improvement. Better Care, Better Value Indicators. http://www.productivity.nhs.uk (accessed 10/06/2015)
- Department of Health NHS Modernisation Agency. 10 High Impact Changes for Service Improvement and Delivery, 2004. http://www.ogc.gov.uk/documents/ Health_High_Impact_Changes.pdf (accessed 10 ⁄ 06 ⁄ 2015)
- British Association of Day Surgery. BADS Directory of Procedures, 3rd edn. London: BADS, 2009.
- Lock, C; Wilson, J; Steen, N; Eccles, M; Mason, H; Carrie, S; Clarke, R; Kubba, H; Raine, C; Zarod, A; Brittain, K; Vanoli, A; Bond, J. North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel nonrandomised preference study, Health Technol Assess. March 2010;14(13):1-164
- Commissioning Guide: Tonsillectomy, 2013, ENTUK, RCS Advancing Surgical Standards. https://www.rcseng.ac.uk/healthcare-bodies/docs/published-guides/tonsillectomy (accessed 13/06/2015)
- Youshani, A, S; Thomas, L; Sharma, R, K. Day case tonsillectomy for the treatment of obstructive sleep apnoea syndrome in children: Alder Hey experience. Int J Pediatric Otorhinolaryngology, Feb 2011; 75(2):207-10
- Soreide, A, K; Olofsson, J; Tonsillectomy - day surgery or hospitalization? Tiddsskr Nor Laegeforen. 1999 April 20;119(10):1423-7
- Ahmad, Z; de Silva, N; Morton, R, P; Wood, A. Safety of day-stay tonsillectomy. J. Otolaryngol. Head Neck Surg. April-June 2010 62(2):158-161
- Verma, A; Nabhani, S, A; Al-Khabori. Adult tonsillectomy and day case surgery. J. Otolaryngol. Head Neck Surg. October-December 2007 59, 341-345
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2018-journal/jods-283-september-2018/tonsillectomy-reducing-length-of-stay-and-increasing-day-surgery-rate/
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6010/guirguis.pdf