Audit on Adherence of Patient Operation Notes to Royal College of Surgeons in England Guidelines « Contents
Authors
Dr William Ward FY1 Doctor
Email: will.ward@nhs.net
Mr David Bunting Consultant Upper GI Surgeon
Email: davidbunting@nhs.net
Abstract
Introduction: All patients undergoing a surgical procedure in the UK should have documentation of the operative details in the medical notes. The Royal College of Surgeons of England (RCSEng) “Good Surgical Practice” document details 21 standards that should be met. This audit aimed to measure how accurately these guidelines are followed in our trust within a defined patient group.
Methods: We identified all patients undergoing day-case laparoscopic cholecystectomy between 1.11.2017 and 31.11.2017 from the electronic operative database ‘Theatreman’. Operative records filed in the patient notes were analysed to see how many of the 21 criteria described in the ‘Good Surgical Practice’ document were adhered to. For each criterion, adherence was deemed good if met in >50% patients and was deemed poor if met in <50% patients.
Results: 29 patients were identified. One set of notes could not be obtained, leaving 28 for the final analysis. One criterion was deemed not applicable in this patient group leaving 20 criteria against which we measured our performance. Adherence to the 20 criteria was deemed excellent in 9 (45%); good in 6 (30%) and poor in 5 (25%).
Conclusions: Standards for operative note documentation are not being consistently met. Results were presented to the departmental clinical governance meeting. The authors made the following recommendations and planned to perform a re-audit in 6 months’ time.
- all notes should be typed on a proforma that includes all RCSEng guidelines
- all surgeons should familiarise themselves with RCSEng guidelines
- a laminated copy of the guidelines should be displayed in every theatre.
Introduction
All patients undergoing a surgical procedure in the UK should have documentation of the operative details in the medical notes. The Royal College of Surgeons of England (RCSEng) “Good Surgical Practice” document details a number of standards/criteria that should be met (1), see Figure 1.
FIGURE 1: Criteria recommended by the Royal College of Surgeons of England for documentation in the operative note.
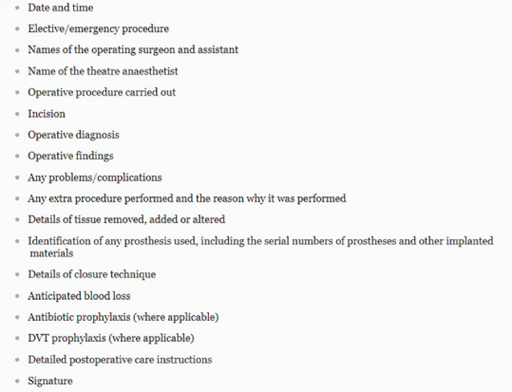
At North Devon District Hospital (NDDH), headed paper with a coloured corner tab is used to document the operative note. These proformas include headings such as ‘date’, ‘surgeon name’ and ‘anaesthetist’. They don’t, however, include headings for every detail that should be included. It has been observed that there is a wide variation in the standard of detail recorded in operative notes. This audit aimed to measure how accurately the guidelines are followed in our day-surgery unit within a defined patient group.
Methods
We identified all patients undergoing day-case laparoscopic cholecystectomy (Operation Procedure Code J18) between 1.11.2017 and 31.11.2017 from the electronic operative database ‘Theatreman. Approval was gained from the local Clinical Audit and Effectiveness department. Operative records filed in the patient notes were analysed to see how many of the criteria described in the ‘Good Surgical Practice’ document, were adhered to. The document lists 18 criteria (Table 1), however, it also states in separate text the importance of including patients’ details and notes being legible. In addition, we separated documentation of date and time, creating a total of 21 criteria to measure against. For each criterion, adherence was deemed excellent if met in 100% cases, good if met in >50% patients and poor if met in <50% patients. Results were tabulated and a cumulative score for each individual criterion was calculated. This enabled an analysis of performance against each of the recognized criteria in the guideline.
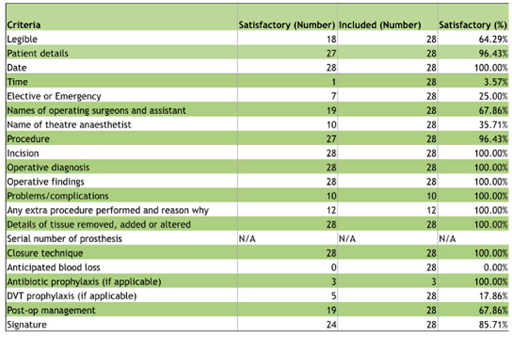
TABLE 1: Compliance of operative note records with guidelines for documentation of 21 criteria defined in the
Royal College of Surgeons of England ‘Good Surgical Practice’ document.
Results
A total of 29 patients identified from the database. One set of notes could not be obtained, leaving a sample size of 28 for the final analysis.
The operation we audited (laparoscopic cholecystectomy) does not require the insertion of any prosthetic material, therefore, the inclusion of this criterion was deemed not applicable for the purposes of this audit, leaving 20 audit standards to measure against, see Figure 2.
FIGURE 2: Proportion of operative note records (as percentage) compliant with guidelines for documentation of
21 criteria defined in the Royal College of Surgeons of England ‘Good Surgical Practice’ document.
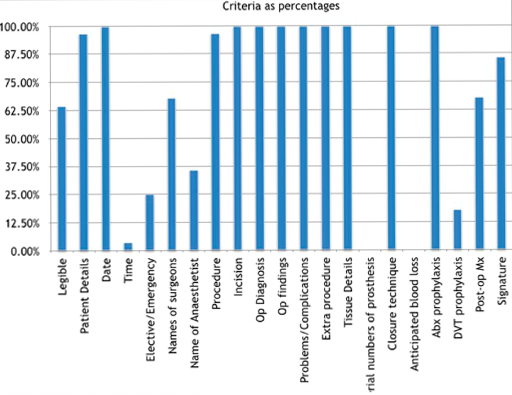
Of the 20 recommendations, adherence was deemed excellent in 9 (45%). These included date, incision, operative diagnosis, findings, problems/complications, extra procedures, closure technique, antibiotic prophylaxis, and details of tissue added, removed or altered. Adherence was good in 6 criteria (30%). These include legibility, patient details, names of surgeon and assistant, procedure, post-op management, and signature. Adherence was deemed poor in 5 criteria (25%). These were: documentation of time of day, elective or emergency status, name of theatre anaesthetist, anticipated blood loss, and DVT prophylaxis. Time of day and anticipated blood loss were particularly poorly documented with inclusion in 4% and 0% records respectively. No operative notes were compliant with all criteria.
Article continues after ad.
Discussion
This audit comparing the standard of documentation in operative notes with national guidelines showed adherence to guidelines was suboptimal for most criteria measured. No operative records were 100% compliant. Notable, those criteria that were particularly poorly documented, often did not have any heading on the proforma. Inclusion of these headings into the proforma would ensure better adherence to the guidelines. It was also noticed that there is a difference in headings on the standard operation note proforma and the day surgery operation note proforma. A universal proforma would help to improve documentation.
Typed notes demonstrated better adherence to the guidelines than handwritten notes. Types notes were used by individual surgeons having created their own templates. None of the typed notes, however, included a signature, rather the surgeon’s name was typed, which was deemed non-compliant with the guidelines.
With regards to legibility, our results may include error whereby some of the recommendations may have been included but illegible. Typed notes would eliminate this error.
Some criteria would only be included if required depending on particular operative factors such as the occurrence of any intraoperative complications. Where these are not stated it has been assumed no complication occurred and the documentation is accurate. It was noted that some surgeons documented specific details such as whether or not bile and/or stones were spilled during the procedure. It’s not clear whether the absence of such events should be specifically recorded, although this would ultimately be best practice and help with further auditing.
Quality improvement interventions
- Results have been presented to the directorate clinical governance meeting
- Laminated copies of the guidelines have been displayed in consultants’ offices and in each operating theatre
- Re-auditing is planned in 6 months.
Conclusions
This audit has shown that surgeons are frequently including the majority of the recommendations set out by the RCSEng for documentation of the operative note. However, there is significant room for improvement which could be achieved by adopting typing operation notes using a template with headings for each of the criteria recommended by the RCSEng. Similar results could be achieved by adopting the use of specific software applications used to generate operative notes based on templates, however, this is likely to require significant investment in computing hardware, software and training.
References
- Royal College of Surgeons of England (2014) Good Surgical Practice. Royal College of Surgeons of England. https://www.rcseng.ac.uk/-/media/files/rcs/standards-and-research/gsp/gsp-2014-web.pdf?la=en
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6009/ward.pdf