Colour-coded Operation Note Paper - A Time Saver: David MacDonald & Steven Lindley « Contents
Authors
Dr. David MacDonald Foundation Year 2 Doctor, Great Western Hospital – Surgical Department
Email: david.macdonald2@nhs.net
Mr. Steven Lindley General Surgical Registrar, Great Western Hospital – Surgical Department
Email: stevenlindley@nhs.net
Keywords: Surgical Ward Round; Operation note; Efficiency.
Abstract
Introduction: Finding a specific item in a patients’ medical records often requires patience. Searching for an operation note can be frustrating and time consuming. Colour-coded paper has long been used for handwritten proformas, but typed documents are often printed on plain white paper.
The hypothesis that colour-coded operation notes help identification and reduce the time to locate was explored to justify the money spent on paper bearing a pre-printed coloured edge.
Methods: Thirty health care professionals participated. Two sets of notes; 15cm and 2cm deep, each had a typed operation note with a coloured edge and one without, inserted, at random, into the notes. Health care professionals were timed to find each operation note in both set of notes.
Results: When comparing the 60 plain notes with the 60 coloured edge notes, a paired T-test revealed statistical significance (p=0.0001). The mean time to find the plain note was 82 seconds, and the note with the coloured edge 20 seconds. The mean difference was 62 seconds.
A paired T-test revealed that there was no statistical difference between the size of the notes when comparing the times to find plane or note paper with the coloured edge.
Conclusion: Identifiable paper saves time when searching through a set of notes. This intervention saves over 1-minute searching for specific items in the notes. This has a real, yet small impact on the efficiency of all healthcare professionals looking after the patient. Although marginal, the potential cumulative gains to patient safety should not be overlooked.
Introduction
The Royal College of Surgeons (RCS) published the Good surgical Practice Guidelines in 2008. These detailed the minimum information required of a surgical operation note, to enable continuity of care by another doctor (1). Legible and accurate documentation has been correlated with improved clinical care (2), facilitates audit and research and provides an important role in medico-legal conflicts (3). Consequently, the RCS guidelines were updated in 2014 to include that operation notes should be preferably typed for every procedure. It has been subsequently evidenced that an electronic operation note proforma markedly improves the quality of documentation (4,5).
Although written operation notes were traditionally printed on colour-edged paper, since the introduction of the electronic operation note, notes are often printed on plain white paper. The increased pressures on healthcare professionals are well documented, and locating a single document within patients’ notes is known to be a laborious and frustrating task.
We hypothesised that using a colour coded operation note with a red stripe down the right-hand side, would decrease time spent locating the operation note, and therefore improve communication and efficiency within the surgical team.
Method
A total of 30 health care professionals from Great Western Hospital NHS Foundation Trust participated. A plain white operation note was randomly included within a set of patient notes, and the participant was timed whilst they found it. The authors felt that random placement reflected common practice, or at least, a predictable position in the notes was not recognised as being reliable in our experience. This process was then repeated using an operation note with a red stripe down the right hand side. This experiment was performed using two sets of patient notes: one 2cm deep and another 15cm deep, to simulate patients with different volume of hospital records, reflecting the average patient.
Statistical Analysis:
Timings were compared using the same participants to find coloured and plain operation notes in each set of notes. Parametric data was analysed using paired Students’ T Test. Statistical significance was set at p < 0.05.
Article continues after ad.
Results
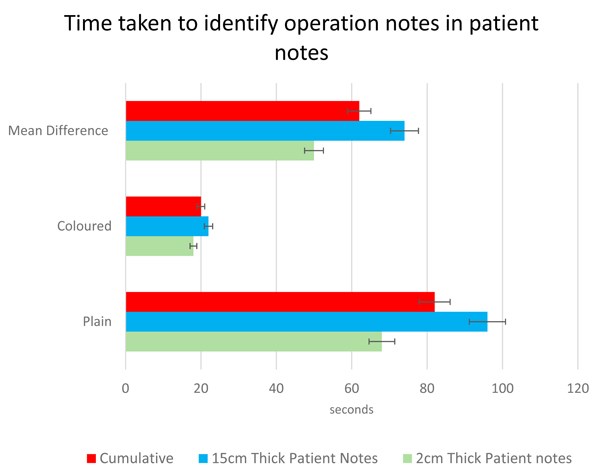
Times taken to find 60 plain operation notes were compared to the times taken to find 60 coloured edge notes. In the 2cm patient notes the mean time taken was 68 seconds for the plain notes versus 18 seconds with the coloured operation note (p=<0.0001) with a mean difference of 50 seconds. In the 15cm patient notes, it took a mean time of 96 seconds for plain notes compared with 22 seconds finding the coloured operation note (p=<0.005), with a mean difference of 74 seconds. Amalgamating the data across patient notes of different sizes, the mean time taken to locate the plain operation note was 82 seconds, and the coloured operation notes 20 seconds (p=0.0001, 95% CI 38.6 – 85.2). There was no statistical difference in the time taken to identify either operation note based purely on the size of the patient notes, plain (p=0.2154) and coloured (p=0.1595).
Table 1: Comparison between times taken to locate plain and colour-edged operation notes in
2 different sizes of patients’ records.
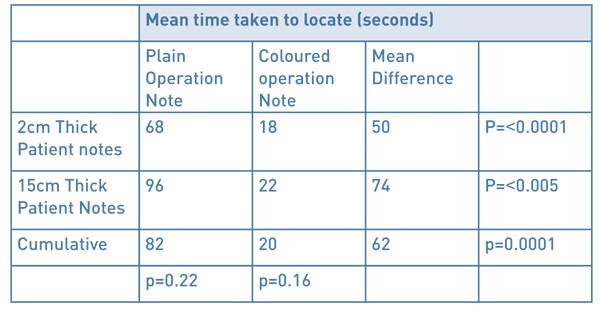
Figure 1: Comparison between times taken to locate plain and colour-edged operation notes
in 2 different sizes of patients’ records. Confidence intervals shown as whiskers.
Discussion
The operation note is an important document, frequently reviewed by many members of the multidisciplinary team. Improvements to Patient Administration Systems (PAS software) has allowed for a growing trend in the creation electronic operation notes. Until hospitals move over to being fully electronic, there is a need for contemporaneous operation notes to be printed and easily accessible in hard-copy form in the notes. With increasing demands on the NHS and the inpatient teams, the requirement for an efficient ward round has never been more important. A simple amendment to the electronic typed operation note, of a red stripe down the right-hand side, resulted in an average of over a minute less spent to identifying it in a set of patient notes. This efficiency is also appreciated by busy allied health professionals when accessing operation notes.
The authors acknowledge that ‘standardised note organisation’ has been a recognised standard agreed by the Academy of Medical Royal Colleges since 2008 (6). The AOMRC do not elaborate as to what taxonomy this standardisation should apply; on the same ward, across an NHS trust, NHS wide? The experience of the authors and the wider surgical team is that note standardisation differs between wards and hospitals. Where standardisation is recognised, the reliability of this is often poor (loose papers put in the front of the notes/ notes filed in chronological order for that admission/notes placed in correct speciality). As a result, our experience is that ‘no system’ is followed when looking for the operation note in the patients record, and thus, our methodology reflects wider practice. We accept that in a well organised institution where there is reliable note organisation, those members of staff whom recognise the standardised organisation, the benefit of colour coded notes on speed of localisation will be less significant. For patients who have had multiple operations, there will be an additional task of reading the date/time/title, in order to sort to the note you require. For many institutions, the accessible notes are the ‘acute’ records, and therefore multiple operation notes in these records will be a relatively rare finding. In this scenario, while it is likely that all of these operation notes are useful to locate quickly and read, the benefit of colour coded notes on efficiently finding the most recent note will be reduced.
Although these efficiency savings are modest, the accumulated effect on efficiency, productivity and therefore patient safety, should not be overlooked.
References
- The Royal College of Surgeons of England. RCSENG - Professional Standards and Regulation; 2014. Good Surgical Practice. https://www.rcseng.ac.uk/standards-and-research/gsp/domain-1/1-3-record-your-work-clearly-accurately-and-legibly/
- Lyons, T.F. and Payne, B.C. The relationship of physicians' medical recording performance to their medical care performance. Care. 1974; 12: 714–720
- Gomey, M. Accurate medical records your primary line of defence. Health Care Risk Rep. 1998; 10: 1
- Coughlan F, Ellanti P, Moriarty A, McAuley N, Hogan N. Improving the Standard of Orthopaedic Operation Documentation Using Typed Proforma Operation Notes: A Completed Audit Loop. 2017 Mar 7;9(3):e1084. doi: 10.7759/cureus.1084
- Int J Surg. 2014;12(5):30-2. doi: 10.1016/j.ijsu.2013.10.017. Epub 2013 Nov 14. 'Smart' electronic operation notes in surgery: an innovative way to improve patient care. Ghani Y1, Thakrar R, Kosuge D, Bates P.
- Academy of Medical Royal Colleges A Clinician’s Guide to Record Standards – Part 2: Standards for the structure and content of medical records and communications when patients are admitted to hospital 2008. https://www.rcoa.ac.uk/sites/default/files/FPM-clinicians-guide2.pdf
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2018-journal/jods-282-june-2018/colour-coded-operation-note-paper-a-time-saver-david-macdonald-steven-lindley
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6196/282-macdonald.pdf