Outcomes and Satisfaction with Semi-elective Day Case Hand Trauma Surgery: Miss Felicity Page, Ms Mary McCarthy & Mr Darren Chester « Contents
Authors
Miss Felicity Pagea, Ms Mary McCarthya, Mr Darren Chestera
Miss Felicity Page Plastic Surgery Registrar
Ms Mary McCarthy Hand Unit Coordinator
Mr Darren Chester Hand and Plastic Surgery Consultant. Plastic Surgery Department and Birmingham Hand Centre, Queen Elizabeth Hospital, Mindelsohn Way, Edgbaston, Birmingham B15 2GW
Corresponding Author Miss Felicity Page Plastic Surgery Department, John Radcliffe Hospital, Headley Way, Oxford OX3 9DU
Email: felicitypage@doctors.org.uk Phone: 01865 741166
Abstract
Introduction In 2003, the University Hospital Birmingham introduced a day case emergency hand trauma operating system1. Appropriate patients are identified at assessment in accordance with strict selection criteria and return for their operation on dedicated hand trauma theatre lists. The service has been shown to improve efficiency and reduce patient complaints1.
Aims The aim of the study was to assess clinical outcomes and patient satisfaction with the service.
Methods Feedback questionnaires were distributed prospectively to patients on emergency hand trauma operating lists. Patients were contacted by telephone and case notes were reviewed at 30 days post operatively. Analysis included patient demographics, injury sustained, operative management, complications and satisfaction results.
Results Results were collected for 100 patients. Overall 93% would recommend the service. There were high levels of satisfaction with all aspects, including information provided (93%), pain management (83%) and comfort going home (86%). The vast majority did not need any further medical input prior to surgery.
99% were supplied with antibiotics in accordance with management protocols. 1.5% of patients with open injuries were treated for a post-operative infection. The mean time between assessment and operation was 2 days.
Conclusion This study has shown that semi-elective day case hand trauma surgery is safe and effective as demonstrated by the low infection rates and high levels of patient satisfaction.
Keywords: Hand, satisfaction, infection
Conflict of interest statement None
Funding declaration None
Introduction
In 2003, the Queen Elizabeth Hospital Birmingham (formerly Selly Oak Hospital) introduced a day case emergency hand trauma operating system.1 The service was designed to improve patient care in response to published data on inpatient hospital delays for those awaiting hand trauma surgery and prolonged overall hospital stay for these patients.2 Patients could often be kept nil by mouth for extended periods of time whilst awaiting their surgery on the joint emergency list, elective cases were also being cancelled due to high bed occupancy by hand trauma patients awaiting surgery. As a result service provision was transformed with patients being sent home and re-admitted semi-electively onto dedicated operating lists. This service was therefore a novel way of managing patients with open injuries and has revolutionised the care of these injuries. It has also reduced the number of cancelations of elective operations due to bed occupancy by hand trauma patients. Validation of the service is important as this approach is now being used in a number of units.
All hand trauma patients are assessed in the Emergency Department. Those considered appropriate for semi-elective day-case procedures are identified in accordance with strict selection criteria. Severe or complex injuries, open fractures, significantly contaminated wounds and bite wounds are not considered appropriate. Patients with significant comorbidities, deliberate harm injuries or those considered unreliable for example drunk patients are also not appropriate. Closed fractures, simple lacerations with suspected tendon or nerve divisions and fingertip injuries are suitable.
Following assessment, antibiotics are prescribed in accordance with the trust protocol and analgesic requirements are reviewed. Wounds are thoroughly washed out in the Emergency Department, frequently under local anaesthetic. Suitable patients are able to go home and return for their operation on a dedicated hand trauma theatre list. Hand unit coordinators (senior nurses) are crucial to the running of the service and are a point of contact for patients.
The hand trauma day surgery unit has been shown to improve efficiency, reduce patient complaints1, reduced in-patient delay and total stay.2
The aim of the study was to assess clinical outcomes and patient satisfaction with the service. Given that this service is novel and involves delayed surgery, the authors sought to specifically evaluate infection rates.
Methods
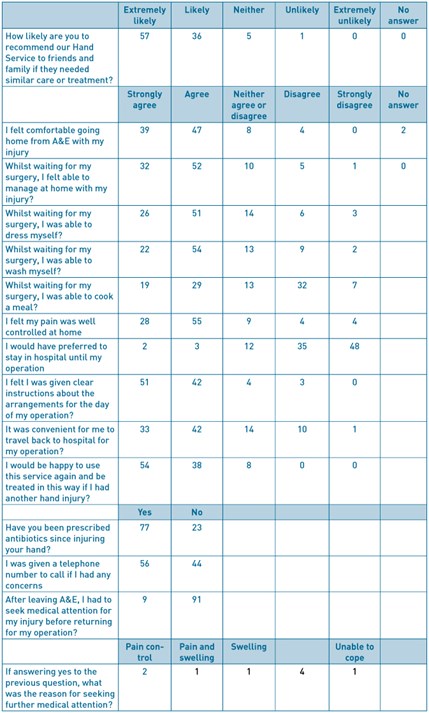
A feedback questionnaire was designed in collaboration with the Trust Audit and Research Department (Figure 1). The questionnaire was distributed prospectively to patients on emergency hand trauma operating lists.
Respondents to the questionnaire were contacted by telephone and a review of case notes was performed at 30 days post operatively. Infection postoperatively was diagnosed according to the Centre of Disease Control and Prevention (CDC) criteria.3 Analysis included patient demographics, injury sustained, operative management, complications and satisfaction results. Local ethics and audit procedures were complied with.
Results
Results were collected for 100 patients in total over 23 operating days. 126 patients were approached, 18 declined, 1 patient was excluded due to a language barrier and 7 patients did not undergo an operation. The mean age was 38 years and 10 months (range 16 years 10 months – 75 years 3 months), 80 patients were male and 20 female.
Overall 93% of patients would recommend the service. There were high levels of satisfaction with all aspects, including information provided (93%), pain management (83%) and comfort going home (86%)(Table 1). The vast majority did not need any further medical input prior to surgery (91%). Those that did, sought further medical attention for replacement of bandages (4%), pain and swelling (4%), and ‘feeling unable to cope’ (1%). No patients required admission prior to their planned operation date. Approximately half of patients could recall being given a telephone number to contact if they had any concerns at home (56%). The vast majority felt that they were given clear instructions for the arrangements on the day of their surgery (93%). 95% of patients would not have preferred to stay in hospital until their operation.
99% of patients were supplied with a course of antibiotics as per the antibiotic management protocol. 68 patients were followed to assess post-operative infection rate, these included all patients with open hand injuries who were contactable by telephone at 30 days post operatively. One patient (1.5%) was treated for a post-operative infection. This patient underwent K-wiring of a distal phalanx fracture and nail bed repair, there were no concerns at initial follow up in the hand surgery department and the patient had completed their prescribed antibiotic course. The post-operative infection was diagnosed by the General Practitioner and managed with further oral antibiotics.
For the 68 patients with open injuries, the mean time between injury and presentation was 0.6 days (range 0–6 days). The mean time between presentation and surgery was 2.1 days (range 1–5 days) and the overall mean time between injury and surgery was 2.7 days (range 1–9 days).
Discussion
This study has shown high patient satisfaction rates with all aspects of the day case hand trauma surgery service. With a unanimous agreement that patients would be happy to use the service again if required. This has been the first published review of patient satisfaction following the introduction of a dedicated hand trauma day-case unit for managing both open and closed injuries, which has now been adopted in a number of units across the country.
With 95% of patients preferring not to be admitted to hospital whilst awaiting their surgery, the service is clearly more convenient for the majority, who would have previously required hospital admission.
Pain management at home was generally good with 92% agreeing that their pain was well controlled. Those who did not feel their pain was controlled well (8%) all had analgesia prescribed when discharged following their initial assessment. These injuries included fingertip lacerations, a laceration with a suspected digital nerve injury and a distal phalanx closed fracture.
Generally patients felt well informed about the arrangements for their operation (97%). All patients are provided with an information leaflet with further details about what to expect, how to contact the department and how the service is run. A minority of patients did not find it convenient to travel back for their operation (11%), however if there are concerns that patients will not re-attend for their operation they are admitted following assessment, alternatively hospital transport can be arranged.
Although overall satisfaction was still very high, the questionnaire has enabled identification of areas for further improvement. These include the need to reiterate information to patients on what they should expect when they go home, the need to ensure patients are aware of the department contact telephone number and make sure they are supplied with written information to reinforce verbal information. The importance of ensuring a supply of analgesia was also highlighted. This feedback has been distributed throughout the department.
Antibiotic prescription was carried out in accordance with the clinical guidelines for 99% of patients. The infection rate was low (1.5%) when compared to other published infection rates for elective and hand surgery 4. Whilst it is possible that infections can be missed, we believe that our methodology kept this to a minimum by not only checking hospital medical records but also contacting patients at 90 days. This study therefore supports the concept that thorough wound washout and antibiotics will allow semi-elective hand surgery without increasing infection rates.
The mean time between assessment and undergoing surgery was 2.1 days. When taking into account the delay in patient presentation, time between injury and operation remained on average between 2-3 days, which is keeping with previously achieved timeframes2. This timeframe does not appear to have any detrimental effects on infection rates and was not highlighted as a concern by any patients within the satisfaction survey.
Success of the hand day-surgery unit is likely to be attributable to a number of factors including appropriate patient selection, adherence with antibiotic guidelines and the employment of dedicated senior nurse hand coordinators who help run the service and provide a point of contact for patients.
This study has shown that semi-elective day case hand trauma surgery is safe and effective as demonstrated by the low infection rates and high levels of patient satisfaction.
Figure 1 –feedback questionnaire completed by patients
References
- BSSH. Hand Surgery in the UK: manpower, resources, standards and training. 2007. Available at http://www.bssh.ac.uk/members/documents/ukhandsurgreport.pdf [accessed 22/11/2015]
- Dillon CK, Chester DL, Nightingale P, Titley OG. The evolution of a hand day-surgery unit. Annals of the Royal College of Surgeons of England. 2009;91(7):559.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, Hospital Infection Control Practices Advisory Committee. Guideline for prevention of surgical site infection, 1999. American journal of infection control. 1999;27(2):97-134.
- Aydin N, Uraloglu M, Burhanoglu AD, Sensöz Ö. A prospective trial on the use of antibiotics in hand surgery. Plastic and reconstructive surgery. 2010 Nov 1;126(5):1617–23.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6185/281-page.pdf