HOW DOES CHRONIC PAIN AFFECT DAY SURGERY OUTCOMES? A DISTRICT GENERAL HOSPITAL AUDIT Navreen Chima & Jane Montgomery « Contents
Authors
Navreen Chima Clinical Fellow in Anaesthesia, Department of Anaesthesia, Royal United Hospitals Bath NHS Foundation Trust, Royal United Hospital, Combe Park Bath BA1 3NG.
Tel: 07951709820 . Email:navreenchima@nhs.net
Jane Montgomery Consultant Anaesthetist, Department of Anaesthesia, Torbay Hospital, Torquay.
Key Words: Perioperative pain, day surgery, audit.
Abstract
Introduction Increasing numbers of patients are living with chronic pain conditions and are regularly utilising opioid based analgesics.1, 2, 3 These patients have been identified as at risk of severe postoperative pain.4, 5, 6, 7 We have reviewed the effect of preoperative pain on progression through the day surgery pathway, and on compliance with national targets in day surgery as proposed by the Royal College of Anaesthetists.
Methods We conducted a one-year retrospective analysis of all patients treated through our day surgery unit. 12 620 patient records were reviewed. 84 were deemed to be high risk of peri-operative pain based on a four-question screening tool previously validated for patients undergoing inpatient surgical procedures.8
Results There were no unplanned admissions related to pain in this high-risk group. Only two patients had severe pain at 24 hours and required further medical input, which is well within agreed national standards. Six had a numerical pain score greater than zero upon discharge from primary recovery and had all undergone orthopaedic procedures. All patients had positive satisfaction ratings following their experience.
Conclusion . This audit suggests that chronic pain should not be a barrier to day case surgery and that standards of care remain mostly compliant with national targets in this challenging patient population.
Introduction
It is well described that both the prevalence of chronic pain and the use of long term opiates is increasing amongst our population.1, 2, 3 This presents a potential problem for how we plan perioperative care for this patient subgroup. There is a suggestion that these patients are at risk of worst postoperative pain experiences and that they require additional input from specialised services such as the acute pain team.4,5,6,7 This difference would suggest that they are more likely to require inpatient care to successfully manage their pain.
At Torbay Hospital patients are screened at preoperative assessment for risk factors indicative of an increased risk of difficultly controlling pain during the postoperative period. This is assessed utilising a four question screening tool previously validated for inpatient surgery at this hospital.7 These risk factors are; a history of chronic pain syndrome, anxiety related to postoperative pain, previous poor postoperative pain control, and double weighting is given to the use of long term opiates. The presence of two or more of these factors was shown to be directly related to both higher postoperative pain scores and increasing input from the acute pain services. A positively weighted result from the screening tool triggers referral to the acute pain services but does not prevent the patient being referred to and undergoing ambulatory surgery.
Aims
We set out to identify whether patient outcomes in this high-risk group are falling outside agreed standards of care for day surgery and, therefore, whether these patients should be referred for inpatient surgery to optimise their perioperative experience.
Standards
The Royal College of Anaesthetists (RCOA) has proposed standards of care related to ambulatory surgery.8 It is stated that:
- The admission rate following day surgery should be locally agreed but targeted to less than 2%.
- Fewer than 5% of patients should report severe pain within the first 48 hours of discharge.
- At least 85% of patients undergoing day surgery should have ‘none’ or ‘mild’ pain following discharge.
- At least 85% of patients should be ‘satisfied’ with their management of pain in day surgery.
Methods
To assess whether this patient population were meeting the described standards of care for day surgery, we carried out a retrospective review of 12 620 patients who passed through the day surgery unit at Torbay Hospital. Patients were captured through visits to the preoperative assessment unit from January to December 2016.
Patient risk factors for postoperative pain were documented on PICIS © preoperative manager. We selected all those patients with positively weighted preoperative screening results. This totalled 84 patients who had a presence of two or more risk factors for difficulty in managing postoperative pain.
Data was collected on postoperative outcomes from our theatre system Galaxy (DXC.technology). This included primary recovery pain scores, discharge analgesia and patient outcomes elicited from a telephone call on day one after surgery.
Results
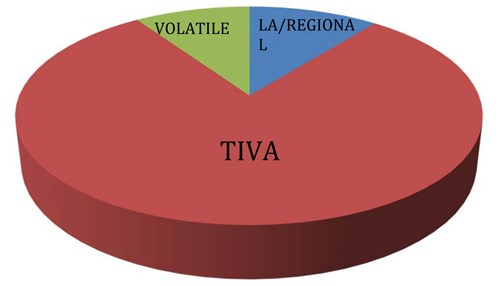
The procedures carried out spanned a range of surgical subspecialties and were representative of a district general hospital (Figure 1). The anaesthetic techniques used intraoperatively were representative of those commonly used in the day surgery unit at Torbay Hospital (Figure 2).
Figure 1: Subspecialty surgeries carried out in Torbay Hospital for patients at risk of difficult postoperative
pain control during 2016.
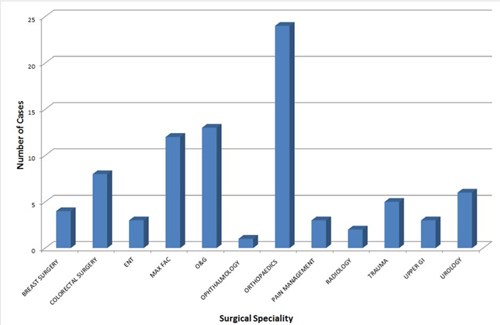
Figure 2: Anaesthetic techniques uses in Torbay Hospital day surgery unit for patients at risk
of difficult postoperative pain control during 2016.
Only one patient needed hospital admission overnight. This was required due to mobility difficulties and was independent of pain. This is well within the 2% admission rate thought to be acceptable by the RCOA and falls at 1.2%.
Pain scores at discharge from the primary recovery were only available for 51% of patients. 95% of these patients reported none or mild pain at this point in their journey (Figure 3). All but six patients were discharged home with a pain score of zero. These six patients had all undergone orthopaedic surgery but continued to successfully complete the pathway without adverse outcomes.
The discharge analgesia patients receive is automatically formulated based on procedure. The data showed that only four patients in the high risk pain group had this analgesia modified.
Follow-up contact is routinely made as part of our day surgery service at Torbay Hospital and 65% of this high risk patient group responded to contact within the 24 hour postoperative period. They answered questions regarding their well being which provided more information on the perioperative pain experience (Figure 3).
Figure 3: Verbal pain rating score reported at time of discharge from primary recovery and at
24-hour follow-up by patients at risk of difficult postoperative pain control during 2016 in Torbay Hospital
day surgery unit.
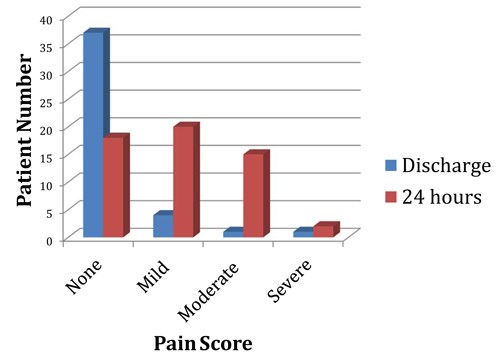
During follow-up only two patients reported severe pain that required further medical input. This falls at a rate of 2.4% and meets the set criteria of less than 5% of patients verbally reporting adverse pain scores. Despite this positive result, severe pain was reported greater than six times more frequently than the entire years patient group, which fell at a rate of 0.4%. Both patients reporting severe pain at follow-up underwent laparoscopic gynaecological surgery. Severe pain did not appear to be related to this specific procedure as eleven other patients also had Obstetric/Gynaecological procedures and up to 40% of the group underwent laparoscopic surgery and did not report severe postoperative pain.
The follow up phone call also revealed that 38 of the 55 responders reported ‘none’ or ‘mild’ pain on the verbal rating scale. This is just 69% of those contacted and falls outside the targeted 85% of patients having low pain ratings following discharge.
Satisfaction with the service was greater than expectations set by the RCOA. 100% of responders described being satisfied or very satisfied with their overall experience of day surgery and their care.
In addition to the parameters suggested by the RCOA, we also looked into the utilisation of the pain services. This had previously been shown to be high in this patient population.7 However, in the context of ambulatory surgery, none of the patients required input from specialised services prior to discharge home and the acute pain team were not recruited to assist with immediate postoperative care in any of the cases.
Discussion
This audit suggests that chronic pain does not adversely affect the progression through the day surgery pathway and produces positive patient experiences. There is also a suggestion that postoperative pain predictors do not hold the same validity in the ambulatory setting where patients are encouraged to be in control of their own analgesia, or may be undergoing less invasive surgery.
The admission rate of 1.2% within the group occurred independently of pain. This fell lower than the year’s overall admission rate of 1.8% based on data collected from 12 120 patients. Of this year’s sample, 28 of the admissions were related to pain despite having no significant patient risk factors for adverse pain outcomes. This demonstrates that patients in whom we predict difficulty in controlling postoperative pain may actually go on to have better pain control postoperatively compared with our general patient population.
From our results more patients in our high-risk population described ‘moderate’ pain after discharge. This may mean they need increased support to reach the targeted day surgery standards. However, the follow-up in Torbay is completed the day after surgery rather than the 48 hour time frame suggested by the RCOA. This would have impacted on the pain levels reported and may negatively skew outcomes. We also know that these patients suffer with pain preoperatively and it may be that this ‘moderate pain’ is their everyday experience. Unfortunately we do not have their preoperative pain scores. It may be worthwhile in future work to compare the preoperative and postoperative pain scores to establish whether these patients are in need of further support.
We accept that the telephone response rate provides incomplete data on follow-up pain scores. The limited response may skew data in that those in pain may not have been able to access the phone, but equally those who did not answer the phone may have been comfortable enough to leave their house. Given this, it is likely that the responders represent a cross-section of the high-risk group. A prospective study could be considered in future work to overcome this limitation and gain a more comprehensive picture of pain levels at 24 to 48 hours. Though not an RCOA proposed standard, a prospective study would also overcome the incomplete data capture within the recovery setting. This is likely to be incomplete due to high clinical workload. This workload may have included addressing pain issues that were not captured in our data set, potentially skewing the pain score at this point in the patient journey.
The follow-up pain scores occurred in the context of 95% of the patients being discharged with a standardised analgesia prescription, unmodified for their risk factors for difficult to control pain. It is worth noting that that this data was derived from the electronic record upon immediately leaving theatre and so discharge analgesia may have been altered at a later point based on recovery experiences. Considering all of this, there may be a benefit in prescribing rescue discharge analgesia to aide comfort in the patient group, and to provide more explicit advice for help with pain management.
This audit also encourages re-consideration of discharge analgesia for this patient subgroup when having specific types of surgery, namely gynaecological and orthopaedic surgery. This audit data does not give an understanding of intraoperative modifications of anaesthetic technique that may alter outcomes such as a greater tendency for regional blocks or local anaesthetic use. Despite this, it is evident that those with multiple risk factors for postoperative pain and having orthopaedic or gynaecological surgery are most likely to need additional analgesic measures upon discharge.
Our audit also has implications for acute pain services in Torbay Hospital and implies that we should not be routinely referring chronic pain sufferers to the acute pain team. This would reduce their work load burden considerably and is a planned change within our department.
These results have helped to encourage both surgical and anaesthetic teams in Torbay Hospital to undertake day surgery in this patient group. A patient information leaflet for chronic pain suffers will support this. This will advise these patients more specifically on their medication management, pain expectations and guidance for help.
Currently the preoperative visit summary alerts the Anaesthetist to the patient with multiple risk factors for poor postoperative pain experience but there is still scope to set up an alert on the electronic discharge prescription to encourage rescue analgesia for improved home pain management.
Conclusion
This audit of a district general hospital day surgery unit suggests that the presence of chronic pain should not be a barrier to day case surgery. These patients generally meet nationally recommended targets and show high satisfaction levels when undergoing ambulatory surgery, perhaps due to their greater autonomy over pain management.
References
- Fayaz A, Croft P, Langford R M, Donaldson L J, Jones G T, Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies, BMJopen, 2016, 6(6). Available from: http://bmjopen.bmj.com/content/6/6/e010364 [accessed 14th February 2018]
- Cartagena Farias J, Porter L, McManus S, Strang J, Hickman M, Reed K, Smith N. Prescribing patterns of dependence forming medicines - analysis using the Clinical Practice Research Database, 2017. Available from: http://phrc.lshtm.ac.uk/papers/PHRC_014_Final_Report.pdf [accessed 14th February 2018]
- NHS England, 2018, Available from: https://digital.nhs.uk/article/4214/Prescribing [accessed 14th February 2018]
- Lewis L, Williams J, Acute pain management in patients receiving opioids for chronic and cancer pain, Continuing Education in Anaesthesia Critical Care and Pain, 2005, 5(4):127-129
- Gramke H F, De Rijke J M,Van Kleef M, Kessels A G, Peters M L, Sommer M, Marcus M A, Predictive factors of postoperative pain after day-case surgery, The Clinical Journal of Pain, 2009, 25(6), 455-60
- Sommer M,De Rijke J M, Van Kleef M, Kessels A G, Peters M L, Geurts J W, Patijn J, Gramke H F, Marcus M A, Predictors of acute postoperative pain after elective surgery, The Clinical Journal of Pain, 2010, 26(2), 87-94
- Magides A, Carter S, Day R, Natusch D, Do pre-operative screening questions on pain predict a worse post-operative pain experience? An exploratory audit, British Journal of Pain; 2013, 7(2 Suppl):5–76
- Royal College of Anaesthetists, 2012, Raising the Standard, a compendium of audit recipes, Available from: https://www.rcoa.ac.uk/system/files/CSQ-ARB-2012_0.pdf [accessed 19th February 2018]
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6184/281-chima.pdf