Evaluation of peri-operative care for hemi-thyroidectomy patients at Nottingham University Hospitals « Contents
Dr Nyssa Comber
Dr Rebecca Binks
Dr Vishal Thanawala, Consultant Anaesthetist
Nottingham University Hospitals NHS Trust
Corresponding author: Dr Nyssa Comber. Email: nyssa.comber@nhs.net
Keywords: Peri-operative care; hemi-thyroidectomy; length of stay
Abstract
Introduction: Shorter post-operative stay leads to improved patient satisfaction and experience, as well as saving revenue and inpatient beds for the trust.
According to Getting It Right First Time (GIRFT) data for Nottingham University Hospitals (NUH) from April 2017 to March 2018, the mean length of stay (LOS) after hemi-thyroidectomy was 1.75 days vs 1.21 days national average. If the national average were achieved at NUH, 41 bed days per year would be saved (£12,300).
The aim of the study was to identify reasons for prolonged length of stay in patients undergoing hemi-thyroidectomy at NUH, and target these as areas for improvement to reduce time spent in hospital.
Methods: Electronic records were used to collect retrospective data for patients operated across NUH from Jan 2018 to Dec 2019 (n=134). We calculated the overall mean LOS and analysed the reasons for delayed discharge in patients who stayed for 2-3 days post-operatively (n =46).
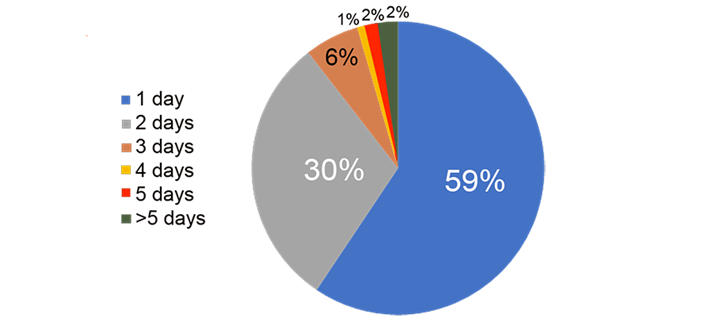
Results: The overall mean LOS was 1.72 days with median being 2 days. The breakdown for all hemi-thyroidectomies was as follows: LOS 1 day 59%, LOS 2 days 30%, LOS 3 days 6%, LOS > 3 days 5%.
No anaesthetic factors were identified as being contributory to extended length of inpatient stay and main reasons for delayed discharge were calcium monitoring and drain output.
Conclusions: Length of stay post hemi-thyroidectomy at NUH is longer than the national average with no anaesthetic reasons identified as being contributory. Calcium monitoring was appropriate as per British Association of Endocrine and Thyroid Surgeons guidelines. There is no strong evidence in the literature for drain insertion post-hemi-thyroidectomy. There is potential to reduce the LOS of patients who were in the hospital for 2-3 days.
Liaise with surgeons to review the use of drains and formulate an ERAS pathway for management of patients undergoing thyroid surgery.
Introduction
Shorter inpatient stay is financially beneficial to trusts and preferred by patients, leading to increased patient satisfaction and better experience. According to Getting It Right First Time (GIRFT) data for Nottingham University Hospitals (NUH) from April 2017 to March 2018, the mean length of stay after hemi-thyroidectomy at NUH was 1.75 days vs 1.21 days national average(1). If the national average were achieved at NUH, 41 bed days per year would be saved, saving £12,300(1).
Day case targets are poorly adhered to nationally(2,3), and as such this is clearly an area that warrants improvement. The BADS Directory of procedures (6th Ed. 2019) provides benchmarking targets for the percentage of patients in whom zero night stays and one night stays are achievable. The directory states a zero-night stay target of 30% and a one-night stay target of 70%. The associated BADS National Dataset (2015) states a day case rate of 35% was being achieved in 5% of trusts and a day case rate of 3% was being achieved in 3% of trusts.
There are currently no trust guidelines for peri-operative management of hemi-thyroidectomy patients at NUH, resulting in variability of management which is often surgeon dependent. In theory, unless there are intra- or post-operative complications, hemi-thyroidectomy should not require inpatient stay >1 day. The aim of the project was to identify reasons for a more prolonged length of stay for patients undergoing hemi-thyroidectomy at NUH, and target these as areas for improvement. We were primarily looking to identify anaesthetic factors that had contributed to delayed discharge.
Methods
Electronic records were used to collect retrospective data for patients who underwent hemi-thyroidectomy (including completion thyroidectomy) between January 2018 and December 2019 (n=134). Anything documented by the parent team which in their opinion prevented discharge was noted. Reasons included: calcium monitoring, ongoing drain output, patient request, post-operative HDU admission, desaturation and new oxygen requirement, post-operative wound infection, abdominal pain, gynaecology review, urinary tract infection, pyrexia, lower respiratory tract infection.
The Early Warning Score (EWS) was also noted, both initially in recovery and at 12 hours post-operatively, to assess whether ‘scoring’ on the EWS was a factor in preventing discharge. The notes were reviewed to identify whether pain or post-operative nausea and vomiting were contributory to ongoing admission.
Inclusion criteria were: elective surgery, hemi-thyroidectomy or completion thyroidectomy, patient operated at NUH (both sites were included), and total hospital stay of 2 or 3 days. We only looked at those patients with a 2 or 3 day length of stay, as we predicted that those were the patients in whom we would be able to improve length of stay the most.
Exclusion criteria were: emergency surgery, any thyroid surgery that wasn’t hemi-thyroidectomy or completion thyroidectomy, patient operated at any other trust, and total inpatient stay of 0, 1, or >3 days.
Since this project was a sample survey aimed at making improvements locally, the only statistical analysis performed was to identify the mean/median length of stay, and mean/median EWS.
Results
There were 134 patients in the cohort overall before the 0, 1, and >3 day stays were excluded. 47 patients were identified as fulfilling all the inclusion criteria. 1 patient was excluded as no clear reason had been documented for delayed discharge. Therefore n=46.
For the patients included, 11% were male, 89% were female [Figure 1: patient gender]. The mean age was 50.8 years. 21% of operations were performed at Nottingham City Hospital by endocrine general surgeons (apart from 1 case which was performed by thoracic surgeons). 79% of operations were performed at Queen’s Medical Centre by ENT surgeons [Figure 2: Hospital trust at which surgery was performed]. 70% of the operations were hemi-thyroidectomies, 30% were completion hemi-thyroidectomies [Figure 3: Surgery performed]. For 89% of cases the anaesthetic technique was TIVA; only 11% of cases were performed using volatile agents [Figure 4: anaesthetic technique].
Figure 1: Patient gender.
Figure 2: Hospital trust at which surgery was performed,
Queen’s Medical Centre (QMC) or Nottingham City Hospital (NCH).
Figure 3: Surgery performed.
Figure 4: Anaesthetic technique.
The length of stay for all hemi-thyroidectomies performed across NUH (n=134 i.e. whole cohort before exclusions) was as follows: LOS 1 day 59%, LOS 2 days 30%, LOS 3 days 6%, LOS 4 days 1%, LOS 5 days 2%, LOS >5 days 2% [Figure 5: Length of stay for all hemi-thyroidectomies at NUH for the period 1/1/18 – 31/12/19]. The mean LOS was 1.72 days, with median LOS 2 days.
Figure 5: Length of stay for all hemi-thyroidectomies at NUH for the period 1/1/18 – 31/12/19.
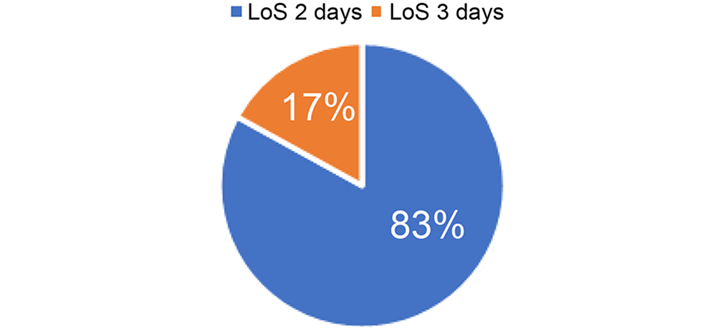
For those patients with LOS 2 or 3 days (n=46), 83% were inpatients for 2 days, 17% were inpatients for 3 days (all of whom were operated on at Queen’s Medical Centre) [Figure 6: length of stay 2 vs 3 days]. The mean LOS for these patients was 2.17 days, with median 2 days.
Figure 6: Length of stay 2 vs 3 days.
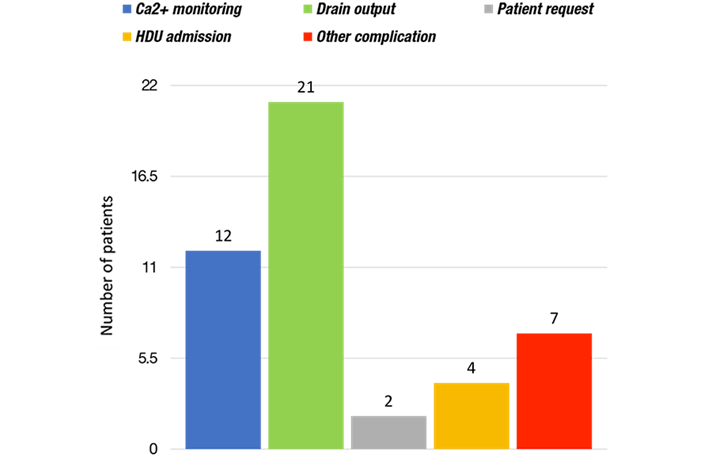
Reasons for delayed discharge were as follows: ongoing calcium monitoring required (26%), drain output too high for removal of drain (46%), patient request to stay in (4%), HDU admission required post-operatively (9%), other complication preventing discharge (15%) [Figure 7: Reasons for delayed discharge]. Other complications included desaturation and new oxygen requirement, post-operative wound infection, abdominal pain/gynaecology review, urinary tract infection, pyrexia, and lower respiratory tract infection.
Figure 7: Reasons for delayed discharge.
The mean Early Warning Score (EWS) in recovery was 0.76, with median 0. The mean EWS 12 hours post-operatively was 0.59, with median 0.
Intra- and post-operative analgesia was found to be appropriate and satisfactory, and there was no documentation of post-operative nausea and vomiting being a particular problem. No specific anaesthetic factors were found to have contributed to prolonged inpatient stay. The main reasons for delayed discharge were calcium monitoring and drain output.
Discussion
When reviewing all patients undergoing hemi-thyroidectomy at NUH from 1/1/18 – 31/12/19 (n=134), the length of stay is longer than the national average (1). The two most significant reasons identified during this project were calcium monitoring and drain output.
According to guidelines published by the British Association of Endocrine and Thyroid Surgeons (BAETS), calcium monitoring is not routinely indicated post-operatively for hemi-thyroidectomy, however it is indicated for completion hemi-thyroidectomy and total thyroidectomy(4). Within the scope of this project (n=46), all patients who were kept in for calcium monitoring had undergone completion hemi-thyroidectomy, and therefore this was appropriate as per BAETS recommendations.
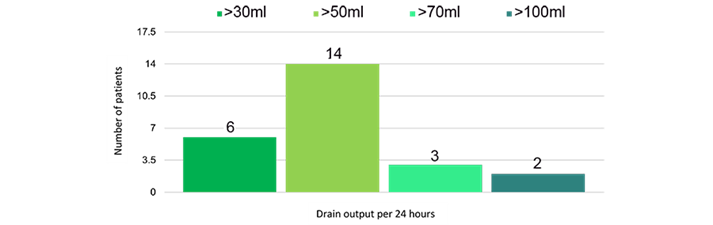
The theory behind drain insertion after thyroid surgery is to prevent haematoma formation, or accumulation of seroma (5). However, there is no strong evidence for this. Despite this, of the 46 patients included in this project, 25 had drains inserted (54%). There are no definitive guidelines at NUH about whether a drain should be used, or what volume of output is sufficiently low for the drain to be removed; as such, these decisions are often surgeon dependent. Generally, if the drain output was >30ml per 24 hours, the drain remained in situ and the patient stayed in hospital [Figure 8: Drain output per 24 hours].
Figure 8: Drain output per 24 hours for patients with inpatient stay of 2 or 3 days.
In one meta-analysis comparing drain vs no drain post thyroidectomy, there was no statistically significant difference between the two groups for haematoma, haemorrhage, hypoparathyroidism, recurrent laryngeal nerve palsy, or seroma(6). Drains have been linked to increased pain post-operatively; increased analgesic requirement, post-operative infection, and increased length of stay (5-8). Many studies have found no significant advantage of post-operative drain for thyroid surgery, including a Cochrane review, which found that there was no clear evidence that using drains in patients undergoing thyroid surgery significantly improves patient outcomes, but may be associated with increased length of hospital stay(8).
This project revealed that there were no zero-day stays in patients undergoing hemi-thyroidectomy for the time period studied i.e. no true day cases were performed. Whilst calcium monitoring was a relevant factor for delayed discharge in patients staying 2-3 days, this did not apply to patients staying 1 night who could have gone home on the day of surgery. Drain insertion prevented patients from going home on the day of surgery, however since this project was primarily investigating reasons for delayed discharge in patients staying for 2-3 days, the overall proportion of drains used for the entire cohort (n=134) was not specifically looked at and as such it was not noted how many of the 1 night stay patients had drains. Undoubtedly a significant factor in preventing zero-day stays is the fact that there is no day surgery pathway in place for patients undergoing hemi-thyroidectomy at NUH.
In view of the findings of this project, it would seem sensible to liaise with our surgical colleagues about the use of drains after thyroid surgery, and formulate an ERAS pathway for peri-operative management of patients undergoing thyroid surgery at NUH.
References
- Getting it right first time. Adult anaesthesia and perioperative medicine review. Nottingham University Hospitals NHS Trust. Provider level report. 6th February 2019.
- BADS Directory of Procedures (6th Edition, 2019).
- Skues, M. BADS Directory of Procedures: National Dataset Calendar Year 2015.
- British Association of Endocrine and Thyroid Surgeons. Guidelines. Available at https://www.baets.org.uk/guidelines/ accessed 10/10/20.
- Kalemera Ssenyondo E, Fualal J, Jombwe J, Galukande M. To drain or not to drain after thyroid surgery: a randomized controlled trial at a tertiary Hospital in East Africa. Afr Health Sci. 2013;13(3):748-755. doi:10.4314/ahs.v13i3.33.
- Tian J, Li L, Liu P, Wang X. Comparison of drain versus no-drain thyroidectomy: a meta-analysis. Eur Arch Otorhinolaryngol. 2017 Jan;274(1):567-577. doi: 10.1007/s00405-016-4213-0. Epub 2016 Jul 28. PMID: 27470116.
- Colak T, Akca T, Turkmenoglu O, et al. Drainage after total thyroidectomy or lobectomy for benign thyroidal disorders. J Zhejiang Univ Sci B. 2008;9(4):319-323. doi:10.1631/jzus.B0720257.
- Samraj K, Gurusamy KS. Wound drains following thyroid surgery. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD006099. doi: 10.1002/14651858.CD006099.pub2. PMID: 17943885.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/52847/313-epcht.pdf