Do Patients Having Day Surgery at The Rotherham Foundation Trust During the COVID-19 Pandemic Feel Safe? « Contents
Apurva Jain1, Rosalind Broe1, Frances C Nolan1, Kim Russon2
1 University of Sheffield
2 The Rotherham NHS Foundation Trust.
Corresponding author Apurva Jain Email: ajain4@sheffield.ac.uk
Key Words: Covid-19; Day Surgery; Patient Experience
Abstract
Introduction: The COVID-19 pandemic has brought unprecedented levels of strain to the NHS, alongside anxieties amongst both staff and patients. As day surgery has been reintroduced, new NICE guidelines¹ have been instituted to ensure patient and staff safety, aspiring to alleviate some of these concerns. We wished to discover the impact on patient experience in day surgery.
Method: Between 10th-17th December 2020, all patients who had attended the DSU at Rotherham Hospital were telephoned post-operatively to complete a brief questionnaire regarding COVID-19 safety measures for their surgery. Patients were asked if they had self-isolated prior to surgery and if social distancing was maintained during their time at the DSU. All patients gave consent for their responses to be included in this audit.
Results: We collected data from 73 patients. 97% of patients were asked to isolate for a minimum of 3 days prior to their surgery. 3% reported not being asked to isolate at all. 88% of patients were given some form of information regarding what isolation entailed, from various hospital sources. 99% of patients felt appropriately social distanced during their day surgery stay.
Conclusions: Overall, most patients felt adequately socially distanced in our DSU and appropriately informed about isolation. Investigation into why all patients do not receive the Trust guidance on isolation is required.
Introduction
The COVID-19 pandemic has brought unprecedented levels of strain to the National Health Service (NHS) 1, 2, alongside anxieties amongst both staff and patients3. With the reintroduction of day surgery, both National Institute for Health Care and Excellence (NICE)4 and the Public Health England 5 created guidelines to advise on the safety measures that hospitals should put in place. This aimed to ensure patient and staff safety, and to alleviate the concerns felt by these groups.
The NICE Guideline4 published in July 2020 regarding planned care recommends that for all planned procedures needing anaesthesia (general, regional and local) or sedation
Patients should be advised to: follow comprehensive social-distancing and hand-hygiene measures for 14 days before admission, to have a test for SARS-CoV-2 no more than 3 days before admission ensuring the results are available beforehand, and to self-isolate from the day of the test until admission.
This then fulfils low-risk criteria according to Public Health England (PHE) guidelines updated in June 20215, thus allowing the patient to follow a low risk covid pathway during their hospital admission. This involves 2m social distancing (or appropriate physical barriers e.g., curtains or screens) and wearing airborne personal protection equipment (PPE) including a face mask. All staff and other care workers must maintain social/physical distancing of 2 metres where possible (unless providing clinical or personal care and wearing PPE as per care pathway). Staff should wear a surgical fluid resistant mask (FRSM), gloves, apron and eye protection. In addition, both sets of guidance4, 5 recommend that visitors are kept to a minimum.
The Rotherham Foundation Trust (TRFT) has introduced guidance based on national guidance 4, 5. Initially, patients were a minimum of 2m distance apart. However, screens and plastic curtains have since been installed (Figure 1), allowing for greater utilisation of space within the Day Surgery Unit (DSU).
Figure 1: Photographs of the safety measures implemented at Rotherham General Hospital.

Patient numbers have been kept low to ensure appropriate social distancing and hygiene measures can be maintained. Initially patients were kept distanced by either waiting within an individual consulting room or at a DSU bedspace until it was time to go to theatre. Now they are able to sit in the waiting area separated by clear Perspex screens which have been agreed by infection control. Staff remained 2m distanced from patients but follow all hygiene and PPE measures when care within 1m is required, wearing an apron, FRSM, eye protection and gloves. There are currently no visitors permitted to the DSU routinely and patients are instead helped to and from their transport outside of the unit.
Prior to attending the DSU, all patients are given an appointment for a drive through COVID-19 test 72 hours before surgery and are told to self-isolate from the time of their covid 19 swab. Prior to the covid-19 pandemic, patients were all contacted the day before surgery to check no changes to their health sine their pre-assessment and to confirm attendance and remind them of their starvation guidance. They are now also asked about symptoms of COVID-19.
The aim of the service evaluation carried out is to explore if the measures described above had been implemented for all patients and ask if it patients felt safe.
Methods
Following approval from TRFT clinical effectiveness department, all patients who had day surgery through DSU at TRFT between 10th-17th December 2020 were telephoned post-operatively to complete a brief questionnaire regarding COVID-19 safety measures.
Patients were asked if they had self-isolated prior to surgery and what guidance, if any, they had received from TRFT in regards to self-isolation. Patients were also asked if social distancing was maintained during their time at the DSU and if they felt these social distancing were appropriate.
Approval was obtained from the Trust to perform the patient questionnaire. In addition, patients gave verbal consent to utilise their responses anonymously, as part of the service evaluation.
Results
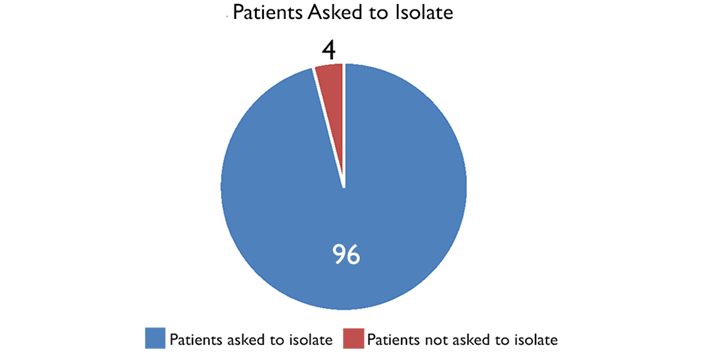
73 patients answered the telephone when we called. With regards to isolation, 70 patients (96%) were asked to isolate for a minimum of 3 days prior to their surgery (Figure 2). The other 3 patients (4%) reported not being asked to at all (Figure 2).
Figure 2: A pie chart showing the % patients asked to self-isolate for at least
3 days prior to their surgery.
64 patients (88%) reported receiving information of what isolation entailed (Figure 3). However, this information came from a variety of sources including the Day Surgery Unit receptionists, assessment nurses and booking administration staff. The surgical division circulated information around isolation to these different departments, but we cannot be sure how standardised the information given by different people was.
Figure 3: A pie chart showing the % patients given some information about
what self-isolation entailed, either in writing or verbally.
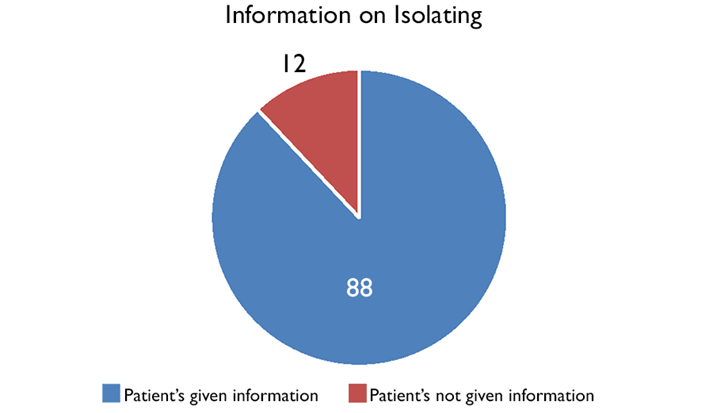
Furthermore, it did not sound like this information was standardised and came from a variety of sources, including the Day Surgery Unit receptionists, assessment nurses and booking administration staff.
All but one of the patients contacted (99%) reported that 2m social distance was maintained throughout their stay at the DSU and felt this was appropriate.
Discussion
The results of this service evaluation are encouraging with regards to the implementation of COVID-19 safety measures at The Rotherham Foundation Trust (TRFT) Day Surgery Unit (DSU). During the period in which this service evaluation took place, the Trust managed a 97% success rate with regards to informing patients of the NICE4 recommendation of 3 days patient isolation pre-operatively. However, this service evaluation assessed only whether patients had been asked to isolate and not whether they had actually isolated. Whether patients followed the advice given or not would be more difficult to assess and would rely on patients reporting honestly if they had failed to do so. To be admitted for surgery the patients needed to say that they had isolated.
Another area of success identified by this service evaluation was the use of 2m social distancing within the DSU. Only one of the 73 patients contacted did not feel this had been achieved during their time at the unit, describing how a member of the domestic services team had been cleaning in the unit without wearing a mask of maintaining a distance from others. As this was only reported by one patient, it may have been an isolated issue and the incidence was reported to senior day surgery staff. This has been reported to the DSU manager to investigate. A repeat service evaluation with a larger sample size is needed to ascertain if similar incidents have been occurring and if further staff training on the use of PPE and social distancing is required.
This service evaluation has identified that improvements to how and when patients are given information about what self-isolating entails are required. Despite the majority of patients being asked to isolate pre-operatively, only 88% reported being given information on what this involved. In order to ensure patients self-isolate effectively, information should be given on what they can and cannot do during self-isolation, and what support is available to them during this time. There is a Trust agreed document based on the national guidance. This has been re-circulated to schedulers and made available on the Trust’s intranet. This information is now also available on the Trust intranet and website.
Currently, patients report information on self-isolation being provided by a variety of staff members at varying times. A lack of clarity and repetition when providing this information may explain why some patients did not feel they received accurate explanations of what is required during self-isolation. This information is usually given by schedulers prior to pre-operative assessment to ensure that patients are taking the correct number of isolation days, using the correct method as stated in the Rotherham NHS foundation trust guidance. If there are new staff to these teams it is important that to ensure that these staff are aware of their responsibilities to provide this information.
In conclusion, this service evaluation has already resulted in some changes but there still may be room for some improvement while we need to continue with measures to reduce the risk of transmission of covid 19. The Rotherham Foundation Trust has been successful in providing a safe elective surgery service through the Day Surgery Unit since June 2020 despite a further wave of covid19. The implementation of current national guidance for maintaining patient safety during the COVID-19 pandemic has patients feeling safe during their admission. The impact of covid-19 is still changing all the time and with it the guidance. It is therefore important to review and up-date the guidance as necessary and consider repeating this service evaluation.
References
- Wielogórska N, Ekwobi C. COVID-19: What are the challenges for NHS surgery?. Current Problems in Surgery. 2020; 57(9): 100856.
- Iqbal M, Chaudhuri A. COVID-19: Results of a national survey of United Kingdom healthcare professionals’ perceptions of current management strategy – A cross-sectional questionnaire study. International Journal of Surgery. 2020; 79(1):156-161.
- Jeyabaladevan P. COVID-19: an FY1 on the frontline. Medical Education Online. 2020; 25(1):1759869.
- National Institute of Clinical Excellence. COVID-19 rapid guideline: arranging planned care in hospitals and diagnostic services. Published 27th July 2020. Available from: https://www.nice.org.uk/guidance/NG179 [Accessed 23rd January 2021].
- Public Health England. COVID-19: Guidance for maintaining services within health and care settings Infection prevention and control recommendations. Version 1.2 published 1st June 2021. Available from:
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/990923/20210602_Infection_Prevention_and_Control_Guidance_for_maintaining_services_with_H_and_C_settings__1_.pdf [Accessed 5th June 2021].
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/52854/313-do-patients-having-day-surgery.pdf