Pain management and patient satisfaction following day case arthroscopic shoulder surgery « Contents
K Kennedy1, J Appiah-Ankam2, BVS Murthy3
1 Specialist Registrar in Anaesthetics, Royal Liverpool and Broadgreen University Hospitals, Liverpool
2 Consultant Anaesthetist, Royal Liverpool and Broadgreen University Hospitals, Liverpool
3 Consultant Anaesthetist, Royal Liverpool and Broadgreen University Hospitals NHS Trust, and Honorary Associate Professor of Health and Life Sciences, University of Liverpool, Liverpool
Corresponding author: Prof. BVS Murthy, Consultant Anaesthetist, Preoperative Assessment Unit, Broadgreen Hospital, Thomas Drive, Liverpool L14 3LB
Email: Burra.Murthy@rlbuht.nhs.uk
Abstract
Introduction: Shoulder surgery is known to be extremely painful and yet it has become successful as a day case procedure due to the routine use of brachial plexus blocks. Recent work has delineated that patients may be experiencing pain following discharge once the brachial plexus block has worn off. A service evaluation was undertaken to assess the incidence of post-operative pain in the first 48 hours and patient satisfaction in patients undergoing day case arthroscopic shoulder surgery.
Methods: This prospective qualitative service evaluation was conducted between January 2019 and June 2019 in patients undergoing day case arthroscopic shoulder surgery on Mondays and Wednesdays with a telephone follow-up interview on Wednesdays and Fridays.
Results: In the immediate post-operative period, out of 50 patients, 48 had good pain relief with no pain; 2 patients (4%) required additional analgesia in recovery or on the day-case unit. During the 48-hour follow up we found that 11 patients (30%) reported severe pain and 12 patients (33%) reported moderate pain at rest. Overall, the mean patient satisfaction score was 8.43. Satisfaction scores were higher for patients experiencing mild to moderate pain compared to severe pain at 48 hours post-operatively (P > 0.05).
Conclusion: We appreciate that patients’ experiences of pain could be improved. We hope to make our post-operative pain protocols more robust and to ensure all patients receive a comprehensive written patient education leaflet about their postoperative pain management.
Keywords: shoulder surgery; day surgery; pain; satisfaction
Introduction
Over the past 40 years, surgery has undergone significant developments leading to widespread change to day case (ambulatory) procedures. This has only been possible with the introduction of new surgical techniques, advances in anaesthesia, and the collection and publication of comparative data, with financial incentives for hospitals to do so.1 In 2013-14, 60.7% of finished consultant episodes involved some form of procedure or intervention, with 95.2% of day case episodes involving a procedure or intervention.1 As per the NHS quality and service improvement tools ‘the patient must be admitted and discharged on the same day, with day surgery as the intended management’: it should be the norm rather than the exception.2
The development of shoulder arthroscopy has bought it into the realms of day case surgery. Although shoulder surgery is known to be extremely painful, it has become successful as a day case procedure due to the routine use of brachial plexus blocks, allowing for reduced opiate doses.3 With increasing use of regional blocks and multimodal analgesia, day case shoulder surgery has been widely adopted across the NHS and has been the norm at our Trust since 2014. Even though it had become a norm for the staff, we wanted to identify the impact on patient related outcomes with this change. We therefore conducted a prospective qualitative service evaluation to understand the patients’ needs, views, expectations, and satisfaction on day case arthroscopic shoulder surgery.
Methods
At a large tertiary University Teaching Hospital in the Northwest of England, we conducted a service evaluation of patients undergoing day case arthroscopic shoulder surgery on Mondays and Wednesdays between January 2019 and June 2019. This service evaluation was approved by the hospital audit department, and no ethical approval was sought due to the non-interventional nature of the work. During their preoperative assessment, all patients were given a leaflet with the details of the various methods of postoperative pain relief that would be offered following shoulder surgery including interscalene brachial plexus block (ISB), oral analgesia etc. During the assessment on the day of surgery, all patients were consented to both anonymised data collection and a post-operative telephone follow up interview.
In the intraoperative phase, anaesthetists were requested to complete a data sheet about preoperative analgesics, ISB details (including time of the block, and volume and concentration of local anaesthetic), any other intraoperative analgesia given, antiemetics used and the volume of intravenous fluids administered. In the recovery ward and day case unit, staff were requested to complete the data sheet with the pain score on admission and at discharge, and any analgesia or antiemetics given. In our unit, we routinely provide one week supply of oral analgesics (codeine and paracetamol) for post-operative pain relief as take-home medication. Occasionally, if the patient is experiencing more pain, we tend to prescribe tramadol and / or non-steroidal anti-inflammatory medication.
After 48 hours i.e., on Wednesday and Friday, a telephone follow-up interview was conducted by the day case unit staff about the patients’ pain management, their experience, sleep disturbance, nausea and vomiting (PONV) and their satisfaction. The overall satisfaction with their pain management was assessed using a visual analogue scale (0 = not happy at all and 10 = extremely happy).
Results
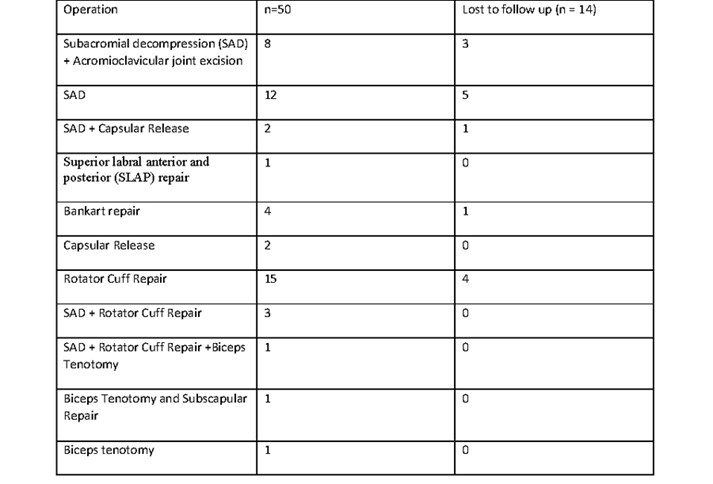
We were able to collect the data from 50 patients (32 males, 18 females) during their hospital stay. The patient ages ranged from 21-77 years (mean 52 years, and median 56 years). The details of various surgical procedures performed on the shoulder are listed in Table 1.
Table 1: The number patients having various surgical procedures and patients who were not contactable f
or a 48-hour postoperative follow up interview.
Intra-operative pain relief
94% of the ISB were performed with ultrasound and use of a peripheral nerve stimulator, the remaining cases were performed using ultrasound alone. The agent used for regional anaesthesia was levobupivacaine mainly with a strength of 0.375% (27 patients), however some anaesthetists used 0.25% (19 patients) or 0.5% (4 patients). The volume used ranged between 12-35 ml with a median of 20 ml. 45 patients received adjuvant dexamethasone (6.6 mg), of which 31 received it intravenously and the rest perineurally.
The range of intraoperative analgesics used was diverse with 34 patients receiving paracetamol, 19 had paracetamol combined with fentanyl or alfentanil, and 11 patients received alfentanil alone. Other analgesic techniques included a combination of those described with adjuncts of joint infiltration, magnesium or morphine/oxynorm. Only six patients received non-steroidal anti-inflammatory drugs (NSAIDs).
Post-operative pain relief
We noted a low incidence of immediate post-operative pain in our cohort with only 2 patients (4%) requiring additional analgesia in recovery or on the day case unit. Of these two patients, one had moderate pain following a subacromial decompression (SAD) and one had severe pain following a rotator cuff repair. The patient who had had a cuff repair and was in severe pain in recovery then complained of no pain on arrival to the ward following morphine 2 mg intravenously in recovery.
Table 2: Pain scores in first 48 hours following their surgery.
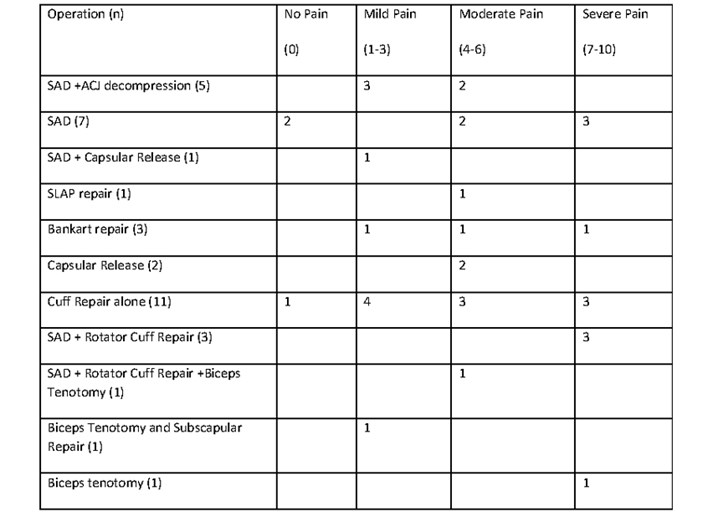
At our 48-hour post-operative follow up, we were able to contact 72% of patients (22 males + 14 females) to assess their experience, their post-operative pain relief, and their satisfaction. The mean duration of block in these patients was 20.5 hours (median 21 hours, mode 24 hours). As demonstrated in table 2, the pain experienced was variable and did not appear to correlate with the surgical procedure. However, cuff repairs did represent half of the patients in severe pain at 48 hours.
In this cohort, 11 patients (30%) reported severe pain and 12 patients (33%) reported moderate pain at rest within the first 48 hours (Table 2). Sleep disturbances were experienced by 25 patients on the day of operation due to pain, discomfort and pins and needles. During the follow up only 6 patients had problems with PONV, 3 were female.
Table 3: Mean, median and mode patient satisfaction scores about their pain relief at rest within first 48 hours of surgery.
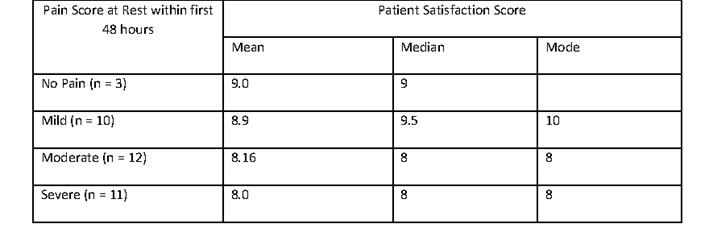
Patient satisfaction
Overall, the mean patient satisfaction score was 8.43 (range 5-10, median 8). Satisfaction scores were higher for patients experiencing mild to moderate pain compared to severe pain (P > 0.05) at 48 hours post-operatively (table 3). The patient who scored 5 had a block duration of 25 hours but severe pain at rest and on movement at 48 hours. She was discharged on paracetamol, NSAID and codeine, but was receiving gabapentin preoperatively. Thirty patients (80%) felt the length of stay was about right. All the additional comments provided by patients on their experience are listed in Table 4.
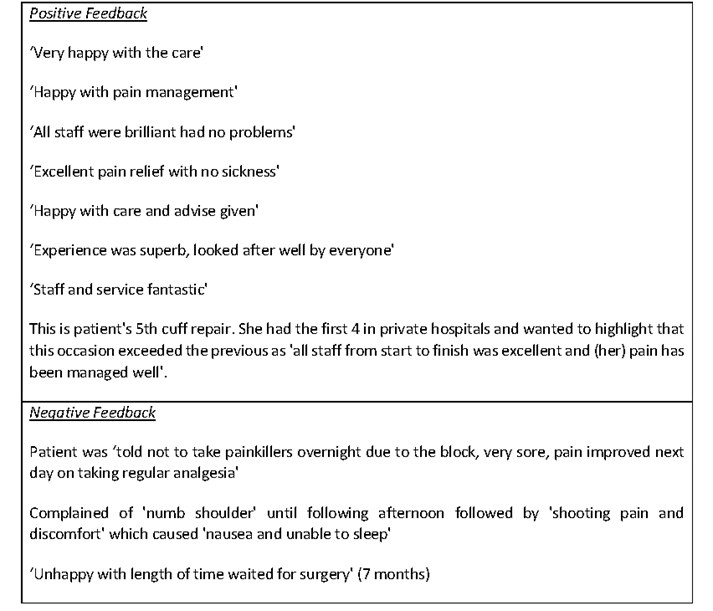
Table 4: Additional patients’ comments about their experience.
Discussion
With advances in surgical techniques and anaesthetic skills, increasingly arthroscopic shoulder surgery is becoming a day case procedure. Postoperative pain management after shoulder arthroscopy is a critical factor in recovery, rehabilitation, and patient satisfaction. Even with these advances, optimal pain relief remains a challenge due to considerable individual variations in the level of pain experienced.4
The success of ISB in 48 patients led to a low incidence of pain (96%) in the early postoperative period within the cohort. Of the two patients, one had moderate pain (SAD) and one had severe pain (cuff repair) in recovery, which settled quickly with a small dose of morphine (2 mg) which suggests it was unlikely to be related to block failure. The benefits of regional anaesthesia for facilitating day case surgery are widely described in the literature.5,6,7 We have not been able to accurately identify why some blocks lasted longer than others. However, we did find that three patients who did not receive any supplementary dexamethasone (intravenously or perineurally), due to other comorbid reasons, had short duration of blocks (8, 10, 17 hours respectively). It is well-established that duration of a single shot ISB can be prolonged by adjunct therapy with dexamethasone.8, 9
Follow up
Our audit has demonstrated that 20 hours of excellent postoperative analgesia may not be sufficient in some day case shoulder surgical procedures, as observed by Wilson et al.5 Regrettably we noted a 30% an incidence of severe pain at 48 hours which is higher than we have seen in previous service evaluations at our trust – 20% in 2015 and 11% in 2012 - when we conducted a follow up telephone interview at 24 hours. In a survey of postoperative analgesia following ambulatory surgery, Rawal et al found 35% of day surgery patients experienced moderate to severe pain during the first 48 hours at home in spite of analgesic medications.10 At present our routine protocol is to send patients’ home with paracetamol and codeine, but in selected cases with moderate to severe pain to send them home with additional analgesia such as tramadol or a NSAID as tolerated or indicated. In view of these audit findings, perhaps it is time to modify our protocol about take home medications.
Our patient reports of pain were diverse, and it is difficult to decipher any correlation between pain and the surgical procedure. However, cuff repairs did represent 6 of the 11 patients (54%) in severe pain in the first 48 hours despite paracetamol, codeine and NSAID, the regimen recommended in the PROSPECT guidelines for rotator cuff repair surgery.11 It is possible these are more painful procedures and would benefit from enhanced analgesia such as oramorph for 3-5 days after surgery.
Oral take home analgesia is currently the only option for day case surgery and single shot ISB only works for short periods. It is possible that our patients’ pain scores may be significantly improved if we were able to instigate a protocol to facilitate a brachial plexus catheter and continuous local anaesthetic infiltration at home. Russon and colleagues described the provision of continuous brachial plexus blocks at their Trust and noted it to produce good analgesia in 90% of their patients.12 Although this would require robust patient selection and coordination with district nursing teams, this looks to be a promising way to improve postoperative pain management and patient satisfaction.
Sleep
It is known that disturbed sleep post-operatively can negatively affect a patient’s recovery.13 In our cohort, pain satisfaction scores were affected by patient experience of poor sleep due to significant pain. How do we improve patient’s post-operative sleep? Perhaps the answer also lies in provision of regional anaesthetic catheters and home local anaesthetic infusions.
Post-operative Nausea and Vomiting
We have previously found an incidence of post-operative nausea and vomiting of 2.87% in patients undergoing any day case surgery at our unit.14 Within the cohort we followed, we noted a lower incidence of PONV (1.67%) that may be due to the lower emetogenic nature of orthopaedic surgery, the higher proportion of males in our cohort and frequent administration of dual antiemetic therapy.
Length of stay
We noted that most patients (80%) were happy with the length of stay which suggests that not only does day case surgery have an economic benefit to the NHS, but patients also prefer day case surgery.2
Patient Satisfaction
Patient satisfaction is a complex outcome to assess and is likely to be related to a number of variables within the patient journey. Some factors contributing to satisfaction in day case surgery are modifiable like managing pre-operative expectations and optimising patient experience of pain.15 Our pain satisfaction scores were not as low as may be expected for the prevalence of severe pain in our patient cohort. Obviously, patients with lower pain scores had higher satisfaction scores and vice versa; as demonstrated in Table 3, although there was no statistically significant difference in the means (P > 0.05).
Patients most frequently commented on pain and it is clearly a focus for patient satisfaction at our Trust (Table 4). While most patient comments in our study were positive and suggested a good patient experience, some were clearly dissatisfied with their pain experience. Overall, we feel the overriding patient positivity is attribute to our day case staff and demonstrates our protocols are benefiting patient satisfaction. Nevertheless, in view of some patients experiencing pain, it is clear we need to address any deficiencies in our protocols. As anaesthetists, our ability to influence surgical outcomes is limited. However, we are able to optimise analgesia for our patients and ensure plans are communicated to patients appropriately. If we are able to minimise the distress caused by post-operative pain, and manage patient expectations well preoperatively, we should be able to have a positive impact on overall satisfaction with day case shoulder surgery.15
Limitations & Conclusion
The provision of day case shoulder surgery at out Trust is well established and dependent on excellent team working between the pre-operative assessment team, anaesthetists, surgeons, and day-case ward nurses. As previously noted in the literature, we have identified that patient satisfaction appears to correlate extensively with patient experience of pain.15 While we appreciate patients’ experiences of pain could be improved, we are pleased to have found relatively high pain satisfaction scores and positive feedback from our patients. Taking into account our findings from this audit, we hope to make our post-operative pain protocols more robust and to ensure all patients receive a comprehensive written patient education leaflet about their postoperative pain management including instructions on taking oral pain killers before their block wears off. This will empower them to play their part in the recovery period and may enhance further patient satisfaction in our service.
Acknowledgements
We would like to thank all the patients, the anaesthetists, recovery, and day case staff for their assistance with data collection during the course of this service evaluation.
Conflicts of Interest: The authors have no potential conflicts of interest to declare.
References
- Appleby J. Day case surgery: a good news story for the NHS.BMJ. 2015 Jul 29;351:h4060. doi: 10.1136/bmj.h4060.
- Same day elective care – treat day surgery as the norm. Online library of Quality, Service Improvement and Redesign tools - NHS Improvement. https://improvement.nhs.uk/documents/2160/same-day-elective-care.pdf
- Conroy BP, Gray BC, Fischer RB, Del Campo LJ, Kenter K. Interscalene block for elective shoulder surgery.Orthopedics. 2003; 26(5):501-3.
- 4.White PF. Pain management after ambulatory surgery – where is the disconnect?Can J Anaesth 2008; 55(4): 201-207
- 5.Wilson AT, Nicholson E, Burton L, Wild C. Analgesia for day-case shoulder surgery.Br J Anaesth. 2004; 92:414-5.
- 6. Joshy, S., Menon, G. & Iossifidis, A. Inter-scalene block in day-case shoulder surgery. Eur J Orthop Surg Traumatol 2006;16: 327–329.
- 7.Sadashivaiah J, Ghatge S. 11. Interscalene Brachial Plexus Block for Post Shoulder Surgery Pain Relief in Day-Case Patients.Regional Anesthesia & Pain Medicine 2008; 33: e
- 8.Pehora C, Peason AME, Kaushal A, Crawford MW, Johnston B. Dexamethasone asan adjuvant to peripheral nerve block. Cochrane Database Syst Rev 2017 Nov 9; 11: CD011770. doi: 10.1002/14651858.CD011770.pub2
- 9.Cummings KC 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, Sessler DI. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine.Br J Anaesth 2011; 107(3):446-53.
- Rawal N, Hylander J, Nydahl PA, Olofsson I, Gupta A. Survey of postoperative analgesia following ambulatory surgery.Acta Anaesthesiol Scand1997; 41: 1017-22.
- Toma O, Persoons B, Pogatzki-Zahn E, Van de Velde M and Joshi GP. PROSPECT guidelines for rotator cuff repair surgery: systemic review and procedure specific postoperative pain management recommendations.Anaesthesia2019; 74: 1320-1331.
- RussonK, Sardesai AM, Ridgway S, Whitear J, Sildown D, Boswell S, Chakrabarti A, Denny NM, Postoperative shoulder surgery initiative (POSSI): an interim report of major shoulder surgery as a day case procedure. Br J Anaesth 2006; 97: 869-873.
- Su X, Wang DX. Improve postoperative sleep: what can we do?Curr Opin Anaesthesiol. 2018; 31: 83-88.
- Mayhew D, Swaraj S, Murthy BVS. Nausea and Vomiting in Daycase Surgery - a Quality Indicator. Journal of One Day Surgery 2017; 26(3): 9-17.
- Jaensson, M., Dahlberg, K. & Nilsson, U. Factors influencing day surgery patients’ quality of postoperative recovery and satisfaction with recovery: a narrative review. Perioper Med 2019; 8: 3. https://doi.org/10.1186/s13741-019-0115-1.
Table 1: The number patients having various surgical procedures and patients who were not contactable for a 48-hour postoperative follow up interview.
Table 2: Pain scores in first 48 hours following their surgery.
Table 3: Mean, median and mode patient satisfaction scores about their pain relief at rest within first 48 hours of surgery.
Table 4: Additional patients’ comments about their experience.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/49086/311-murthy.pdf