Day Case Mastectomy Target : Achievable and Sustainable for the Future of the NHS « Contents
Miss Gwen Bromley Specialist Registrar, Queen Elizabeth Hospital Gateshead
Dr Claudia Wilson Foundation Doctor, Queen Elizabeth Hospital
Miss Annie Chan Specialist Registrar, Queen Elizabeth Hospital Gateshead
Mr Mujahid Pervaz Consultant Oncoplastic Breast Surgeon, Queen Elizabeth Hospital Gateshead
Corresponding Author. Email: Gwen.bromley@nhs.net
Keywords: Mastectomy; Day Case; Target; Same Day Discharge
Acknowledgements Mr S Amonkar, Mr K Clarke, Ms T Fasih, Ms L Jalini, Mr R Milligan
Abstract
Introduction: Mastectomies are a common procedure in the management of breast cancer. National guidelines now recommend that we aim to carry out 50% of mastectomy procedures as day-cases. We evaluated all mastectomies carried out during a 6-month period after the introduction of a programme of education. Specifically investigated, was the frequency of day-case mastectomies highlighted as an area requiring considerable improvement following a previous study.
Methods: mRetrospective cohort analysis using electronic patient records for all patients who underwent mastectomy over a defined 6-month period.
Results: Data from 82 patients collected with an average age of 58. Overall rate of day-case mastectomy was 54.9%, including patients with immediate reconstruction and nodal procedures. 62% of patients who underwent simple mastectomy had their procedures performed as day-cases compared to 35% of patients in 2017. Mean length of stay decreased for all types of mastectomy over this period compared to previous.
Conclusion: The rate of day-case mastectomy improved significantly. This can be attributed to a drive-in managing patient expectation and re-education of staff. However, many factors still contribute to overnight stay such as post-operative intravenous antibiotics and the use of drains. Optimising theatre lists and careful planning will allow maximum recovery time for mastectomy patients and improve the chances of a day-case outcome.
Introduction
Mastectomies are carried out regularly in the UK for the treatment of breast cancer. These procedures historically required prolonged hospital stays post-operatively, however there is currently a drive towards carrying out most mastectomies as day-case procedures. Indeed, the British Association of Day Surgery (BADS) released national targets stating that 50% of simple mastectomies, with or without axillary procedures, should be performed as day-case procedures [1]. Most clinicians are keen to encourage day-case surgery both for improved patient satisfaction, but also to maximise financial benefits.
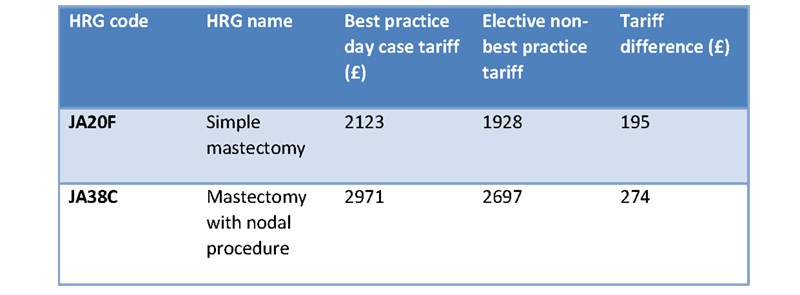
The financial incentives for day-case mastectomy surgery are considerable, both regarding tariffs and excess bed-day cost. If mastectomies are carried out as day-cases (under the payment by results system) the best practice tariff is received. For a simple mastectomy, the day case tariff is £2123 compared to the inpatient tariff of £1928, representing a saving of £195 per patient. Similarly, for a mastectomy with a nodal procedure the day-case tariff is £2971 compared to £2697, representing a saving of £274 per patient, see Table 1 [2]. Furthermore, the excess bed day cost is estimated to be £300 per patient per day. These savings are significant, especially given the frequency of mastectomy in breast surgery practice.
Table 1: Best Practice Day Case Tariff Rates for mastectomies [2]
A retrospective study was undertaken at our UK centre. We are a high-volume breast screening unit and therefore perform a moderate number of mastectomies each year. This study evaluated all mastectomies carried out over a 6-month period looking specifically at how many of these were performed as day-cases and specific reasons for those that resulted in a post-operative overnight stay.
Over the study period, 106 mastectomy cases were performed and of these, 35% were day-cases. This percentage was well below the 50% target set out by BADS. It is suggested that the top 5% of centres in the UK should achieve day-case mastectomy rates of 44% for simple mastectomies without axillary surgery and the top 25% of centres achieving a day-case rate of 12%. BADS also make a recommendation for mastectomy with axillary surgery; the top 5% of centres achieving rates of 42% for day-case procedures and similarly the top 25% having rates of 11% [1]. Therefore, our centre was performing within the top 25% of centres, however, was falling short of the top 5% of centres.
Reasons as to why we were falling short of the top 5% of performing centres nationally were discussed and efforts were made to educate the breast surgery department (clinicians and breast care specialist nurses) in the advantages of day case mastectomy for both patient satisfaction and the financial benefits for the trust. We focussed heavily on shifting patient expectations and ensuring that, where appropriate, patients would be counselled from the outset that their procedures would be carried out as day-case procedures and that this is now standard operating practice across the department. The two study periods were compared to see if improvements had been made, specifically in day case mastectomy rate.
Methods
Patient details were collected for all patients who were coded as having a ‘mastectomy’ procedure over a 6-month period and a retrospective analysis of these patients was carried out. We used electronic patient records to collect our data from operation notes and GP handover letters and collected the data in the same format as our initial study.
Results
Over the re-audited period, 90 patients were coded as ‘mastectomy’. Of these, 8 were excluded due to being incorrectly coded, for example some cases were ‘revision of mastectomy scar’. Therefore 82 patients were included in our data set, 80 of these were female and 2 were male. 24 patients had immediate reconstruction surgery. 43 patients had simultaneous sentinel lymph node biopsies (SNLB), 22 had axillary node clearances (ANC) and 18 had no nodal surgery. The average age of our patients in this cohort was 58 with 17 patients aged 75 or over.
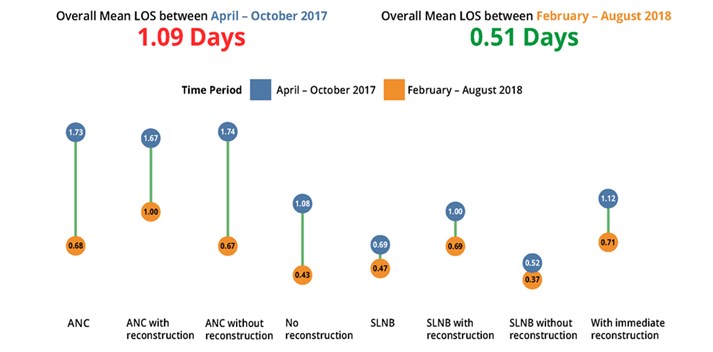
Of the 82 cases, 45 were carried out as day-cases. This gave an overall day-case rate for all mastectomy procedures of 54.9%. Indeed, the mean length of stay (LOS) for all types of mastectomy decreased from 1.09 to 0.51 over the two study periods. Of the cases which were ‘simple mastectomies’, 62% of these were carried out as day-cases.
Mean LOS improved for all mastectomy procedures, be that with nodal clearance or reconstruction, see Figure 1.
Figure 1: The Difference in Mean Length of Stay Between the Two Cohorts (according to type of procedure).
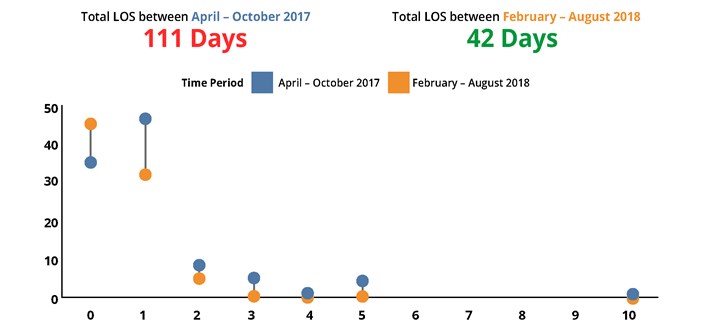
Most cases in the latest cohort were carried out with a one-day hospital stay or less. The longest in-patient stay in the later cohort was 2 days, this contrasts with the results from 2017 where a higher proportion of patients stayed for 3 days or more, as shown in figure 2.
Figure 2: Change in total Length of Stay.
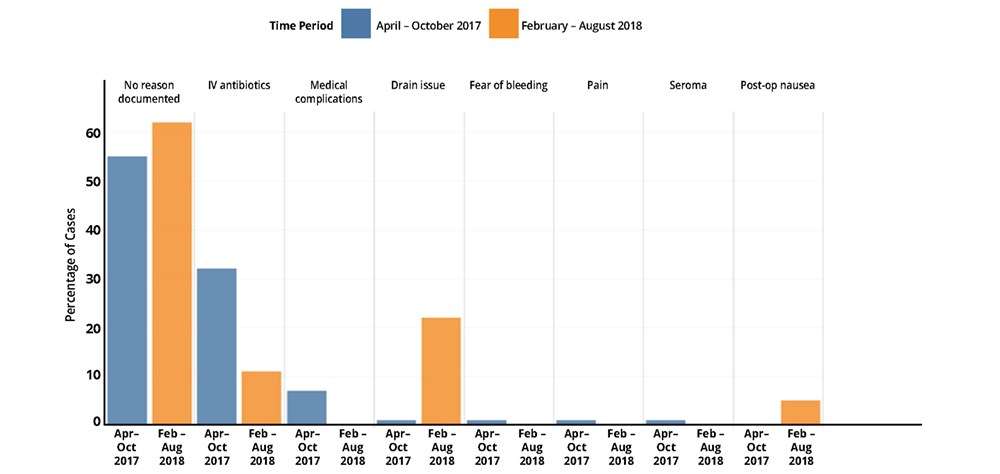
We also reviewed the reasons why patients were not discharged on the day of surgery. Unfortunately, analysis showed that in most cases these reasons are not recorded on the operation note or discharge documentation. However, the use of drains and IV antibiotics were consistently shown as reasons for patients to remain in hospital overnight. See figure 3 for a breakdown of these reasons in both cohorts.
Figure 3: Reasons Recorded for Increased Length of Stay.
Discussion
Mastectomies remain common procedures in the UK. It is an operation which is relatively short in duration with low levels of post-operative pain and minimal serious complication, therefore it is a good candidate for a day-case procedure. Indeed since 2007, as part of the Cancer Reform Strategy [3] work has been done to improve and streamline the breast cancer surgical pathway. It was noted that in doing so, length of stay could be reduced by 50% and therefore over 25% of unnecessary bed days could be released for 80% of major breast surgery [3]. The financial implications of this are remarkable. As noted earlier, the difference in tariff between the day-case and non-day case rate for a simple mastectomy is £195 [2]. With 43% of women who have surgery for breast cancer each year opting for mastectomy, this relatively small saving would lead to a monumental saving.
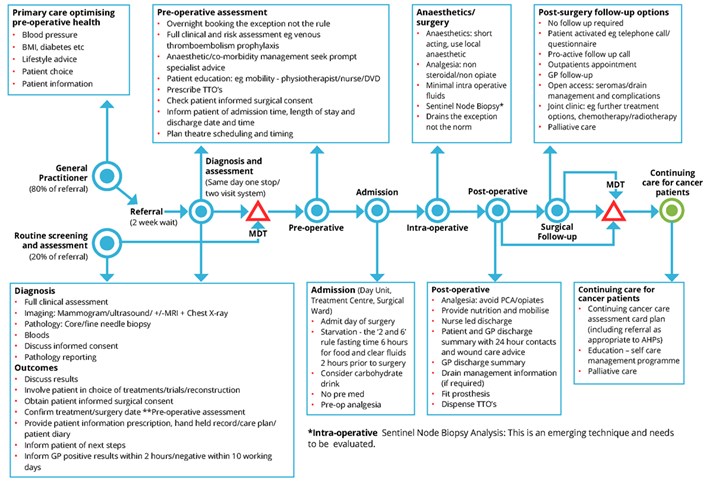
Improvements are being made on a national level. An NHS Improvement project into delivering day-case surgery safely revealed a 52% improvement in length-of-stay from 2007 to 2011. This was attributed mainly to improving the day case breast surgical pathway, as shown in figure 4.
Figure 4: Day Case Breast Surgical Pathway (excluding reconstruction) [3]
Our study observed that, although many patients who have a drain sited do still achieve a same day discharge, in a small percentage of patients the drain caused issues such as pain or significant amounts of fluid leakage which was documented as the reason for their overnight stay. The use of drains is a contentious issue with a large volume of published literature both in favour and against the use of drains. Indeed, many surgeons have adopted techniques such as quilting or tissue adhesives to avoid drain placement. In contrast, some clinicians feel that having a no-drain mastectomy is feasible and safe with no influence on seroma formation. Despite surgeon preference, no single technique has proven superiority, this remains a point for debate and further formal research is ongoing in multiple centres to provide some clarification on this for example the SAM trial [4].
Our data highlighted the prescribing of post-operative IV antibiotics as a reason for overnight stay post-mastectomy. Research into this shows that post-operative antibiotics are rarely indicated and, even in the presence of reconstructive surgery, guidelines are inconsistent and vague. This is an area where further research/clarification may assist in further reducing overnight stay post mastectomy [5].
When we discussed the results of this study, it was felt that further work should be done to look at whether the position of the mastectomy case on the list has any impact on whether the case is done as a day-case. There may be a correlation between cases done at the end of an afternoon list and a longer length of stay, simply due to observation time post-operatively. This is an area which we hope to look into more in future studies because there may be scope to prioritise mastectomies at the start of lists in order to increase the likelihood for the case to be done as a day-case.
The psychological benefit of day-case mastectomy surgery is important with many patients preferring to return to their own environment as soon as they are able. This is in addition to the other benefits of day-case surgery which are well documented such as earlier mobility and therefore decreased risk of DVT and lowered risk of hospital acquired infections [6].There is limited literature about how to best to psychologically prepare patients for breast cancer surgery and this is perhaps a field in which more work can be done.
Conclusion
This study has shown that the rate of day-case mastectomies has improved considerably at our centre and that the BADS targets are achievable. We feel that the main driving force behind our improvement in day case mastectomies comes from shifting patient expectations. We hope that by continuing to communicate more thoroughly with our patients about their anticipated journey through the mastectomy process these rates will only improve further. Inevitably some cases will require a prolonged hospital stay due to reasons beyond our control such as co-morbidities or unanticipated surgical complications leading to a deviation from the normal post-operative plan, however on the whole, day case mastectomy is an achievable and sustainable goal. It is important that improving day-case rates should not be prioritised over patient safety however where possible, day-case surgery is now the expectation and not the exception for our patients.
References
- British Association of Day Surgery (2019) Trust Performance. Available at https://daysurgeryuk.net/en/resources/trust-performance/ (Accessed June 2019)
- National Health Service (2018) National tariff payment system 2017/18 and 2018/19. Available at https://improvement.nhs.uk/resources/national-tariff-1719/ (Accessed May 29th 2019).
- National Health Service (2011) Delivering major breast surgery safely as a day case or one-night stay. Available at www.improvement.nhs.uk/cancer (accessed May 30th 2019)
- J. van Bastelaar, R. Granzier, L. M. van Roozendaal, G. Beets, C. D. Dirksen, and Y. Vissers (2018). ‘A multi-center, double blind Randomized Controlled Trial evaluating flap fixation after mastectomy using sutures or tissue glue versus conventional closure: protocol for the Seroma reduction After Mastectomy (SAM) trial.’ BMC Cancer (2018) 18:830
- Ariyan S1, Martin J, Lal A, Cheng D, Borah GL, Chung KC, Conly J, Havlik R, Lee WP, McGrath MH, Pribaz J, Young VL (2015). ‘Antibiotic prophylaxis for preventing surgical-site infection in plastic surgery: an evidence-based consensus conference statement from the American Association of Plastic Surgeons.’ Plastic Reconstruction Surgery 2015 Jun; 135(6):1723-39
- International Association of Ambulatory Surgery (YEAR/YEAR). Policy Brief- Day Surgery Making It Happen. Available at http://www.euro.who.int/__data/assets/pdf_file/0011/108965/E90295.pdf (Accessed May 30th 2019)
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2020-journal/jods-303-august-2020/day-case-mastectomy-target-achievable-and-sustainable-for-the-future-of-the-nhs
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40117/303-day-case-mastectomy-target-achievable-and-sustainable-for-the-future-of-the-nhs.pdf