Achieving success in day case laparoscopic anti-reflux surgery using a standardised peri-operative protocol in a Cornish cohort « Contents
Mr David Griffith*, Ms Alexandra Millerǂ, Mr Michael Hutton†, Mr James Clark*, Mr Allwyn Cota*, Mr Ian Finlay*, Mr Paul Peyser* and Mr Michael Clarke*
*Consultant ǂCore Trainee †Staff Grade doctor
Upper GI Surgery Department, Royal Cornwall Hospital, Truro, Cornwall, TR1 3LJ, United Kingdom
Corresponding author: Email: davidgriffith1@nhs.net
Keywords GORD; Fundoplication; Day Case
Abstract
Background: Laparoscopic anti-reflux surgery is an effective treatment for gastro-oesophageal reflux disease (GORD). Recent publications have highlighted the low national day case rate for this procedure with wide variation in conversion and volume by centre. Our unit has performed this procedure as day case since 2014 and we report our outcomes.
Method: Patients were suitable for day case, unless they had a hiatus hernia containing more than half of stomach or no adequate home support. Patients underwent pre-operative endoscopy +/- oesophageal physiology studies. A standardised evidence-based peri-operative protocol was developed after reviewing our initial experience. Patient information leaflets were provided with counselling in clinic. Nissen and anterior fundoplications were performed across 2 sites by 5 surgeons. Patients were not randomised to treatment.
Results: Since 2014 there have been 202 primary fundoplications with equal sex distribution and median age 49 years. The day case rate was 86.6%. There were 97 Anterior and 105 Nissen fundoplications. Our 2 day readmission rate was 4.95% (n=10) and 30 day readmission 8.4%, with pain (4.5%) and dysphagia (3.5%) the most common reasons for readmission. 0 cases were converted to open and there were 0 mortalities. Patients had recurrent symptoms in 11.9% however the revision surgery rate was 4%. There were no significant differences in complications between anterior and Nissen fundoplication other than gas bloat (11 (6.9%) vs 3 (2.9%) Fisher’s Exact p=0.002).
Conclusion: Using a standardised peri-operative protocol, patient counselling and early telephone follow up, a day case rate of >80% for laparoscopic anti-reflux surgery is achievable. This is in keeping with the recently published Getting It Right First Time (GIRFT) document for General Surgery.
Introduction
Laparoscopic anti-reflux surgery is an effective treatment for gastro-oesophageal reflux disease (GORD) in those patients who fail or are unable to tolerate medical treatment1,2. Outcomes are similar for different laparoscopic fundoplication techniques3-6 with laparoscopy offering advantages over open surgery with regards reduced length of stay and decreased post-operative pain 7-9. A number of studies have also demonstrated the feasibility of performing anti-reflux surgery as a day case procedure10-15. This is in keeping with the recently published ‘Getting It Right First Time’ (GIRFT) document for General Surgery in the UK16, recommending increased uptake of anti-reflux surgery as a day case procedure. However, a recent review of 12,086 patients undergoing anti-reflux surgery in the UK highlighted a day case rate of only 15.1% 17. Previously published data from our institution demonstrated our initial success in achieving a 70% day case rate, with the most common barriers to discharge including post-operative pain and nausea18. This study was to assess the impact of introducing a new standardised protocol for day case anti reflux surgery and the iterative process to improve day case rates, address barriers to discharge and reduce readmission rates.
Methods
Data were collected prospectively and analysed retrospectively for all consecutive patients undergoing primary laparoscopic anti-reflux surgery (both Nissen and anterior fundoplication) between December 2014 and April 2019. Patients were offered fundoplication according to surgeon expertise and gave fully informed consent. Ethical approval was not required as treatment was decided between surgeon and patient as per routine practice. This retrospective data analysis was not registered as a trial. Data analyses were performed between anterior and Nissen groups using Chi-Squared test (χ2) and Fisher’s exact test when the frequencies were less than 5. All available medical records were used to reduce missing data. Data analyses were performed by one author not responsible for patient selection or inpatient observation.
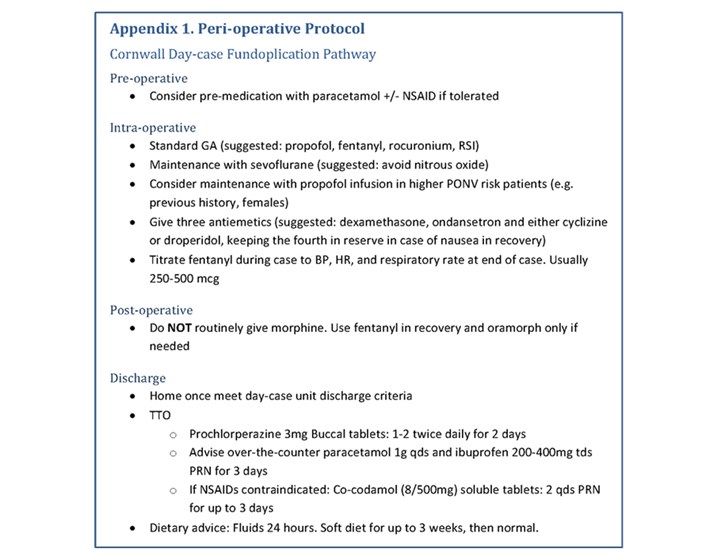
Following literature review, retrospective data analysis and collaborative consultation with the anaesthetists, a standardised peri-operative protocol was developed (Appendix 1).
Eligibility Criteria
Eligibility criteria included those patients deemed suitable for day case surgery, with GORD, American Society of Anesthesiologists (ASA)19 grade of I - III and adequate home support. Patients were not considered eligible if there was no responsible adult at home after surgery for the first 12 hours. Patients were excluded from day case surgery where a hiatus hernia was known to contain more than half of the stomach.
Pre-operative Management
All patients underwent upper gastrointestinal endoscopy pre-operatively. In patients without endoscopic evidence of GORD or HH oesophageal physiology studies including a combination of high resolution manometry, pH and impedance studies were undertaken. Patients were counselled in the outpatient clinic, provided with an information leaflet about day case anti-reflux surgery and scheduled at the start of the operating list, with all surgery performed within a facility able to discharge patients up to 22:00.
Intra-operative Management
Laparoscopic Nissen 360 degree or anterior fundoplication was performed according to surgeon preference, across two sites by five surgeons.
A standardised anaesthesia protocol was used as follows. Pre-medication with paracetamol +/- non-steroidal anti-inflammatory (if tolerated) was considered. A standard general anaesthesia was induced with propofol, fentanyl and rocuronium and maintained with sevoflurane, avoiding nitrous oxide. For those patients with documented higher post-operative nausea and vomiting risk anaesthesia was maintained with propofol. Three antiemetics were used where possible including dexamethasone, ondansetron and either cyclizine or droperidol, keeping the fourth in reserve in case of nausea in recovery. Intra-operative analgesia was fentanyl titrated to blood pressure, pulse, and respiratory rate.
Patients were placed in lithotomy position with table tilted head up. Laparoscopic anterior fundoplication was performed with standardised 4 port and liver retractor technique. A 10mm port placed superior to umbilicus for laparoscope, a 10mm left mid clavicular line sub costal port, left anterior axillary line 5mm port, right mid clavicular line 5mm port and epigastric 5mm port for Nathanson liver retractor (Cook Medical Technology, Bloomington, USA), Hiatal dissection was performed with combination of blunt and sharp dissection with ultrasonic energy device (Lotus, BOWA Medical, UK). The oesophagus was mobilised and encircled with a nylon tape, to allow minimum of 2.5cm of intra-abdominal length and visualisation of both hiatal pillars, preserving the vagus nerve. Posterior crural 2-0 Ethibond sutures (Johnson & Johnson, Belgium) were placed with the use of Teflon pledgets (Johnson & Johnson, Belgium). Tension free anterior 180° partial wrap was performed with 2-0 Ethibond sutures (Johnson & Johnson, Belgium). The right side of the fundus is sutured to the adjacent left side of the oesophagus with two interrupted sutures to accentuate the angle of His. A top suture is placed through the top of the fundus, the oesophagus immediately below the hiatus, and the apex of the hiatus. Next the fundus is sutured to the right lateral wall of the abdominal oesophagus and to the right hiatal pillar using two interrupted sutures.
Nissen fundoplication was performed with identical laparoscopic port positioning, initial dissection and crural repair. The short gastric vessels were not routinely divided. Posterior 360° complete, floppy, fundoplication was performed with 3 or 4 anterior securing 2-0 Ethibond sutures (Johnson & Johnson, Belgium). The cranial suture was gastro-gastric including a bite of anterior oesophageal wall and the inferior sutures gastro-gastric. This allows a 2-3cm floppy fundoplication anchored to oesophagus.
Routine post-operative intravenous morphine was avoided, using fentanyl in recovery and oral morphine only if needed (Appendix 1). 20ml of 0.5% levobupivacaine was infiltrated in the wounds at completion of surgery.
Post-operative Management
When patients satisfied the discharge criteria encompassing pain score, responsiveness, normal observations, and tolerance of liquids they were discharged with prochlorperazine 3mg buccal tablets: 1-2 twice daily for 2 days and advised over the counter soluble analgesia.
A standardised post-operative dietary plan was followed with further information contained in patient information leaflets. This included fluids for 24 hours, soft diet for three weeks then reintroduction of normal diet.
Specialist nurse telephone follow-up occurred on day 1, week 1 and patients had a follow up clinic appointment with the surgeon at 6 weeks to ensure patient safety. Any re-presentations over the 5-year period were recorded and patient notes reviewed for previous procedures.
Results
All data were prospectively maintained in a database. Between 2014 and 2019, 202 consecutive primary laparoscopic fundoplications were performed. The study period captured data over 5 years with patients having planned follow up as outlined previously. 86% (174/202) of patients were successfully discharged from clinic at 6 weeks follow up and were not referred back in the study period.
Primary Anti-reflux Surgery
There was an equal sex distribution and median age 49 years (Range 16.9 to 84.1 years). The median BMI was 29 (Absolute range 17.8 – 39.1 Kg/m2). There were 101 patients classed as ASA class 1(50%), 90 class 2 (44.6%) and 11 class 3 (5.4%). There were 97 Anterior (48.01%) and 105 Nissen (51.98%) fundoplications performed by 5 surgeons. 135 patients (66.8%) underwent oesophageal physiology studies.
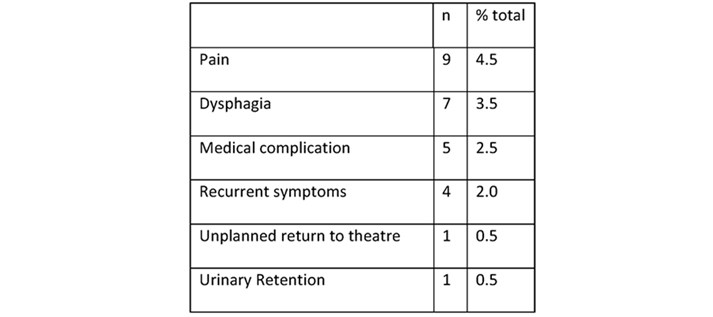
The day case rate was 86.6% (155/179) with a 23-hour stay rate of 95.5% (193/202). In 23 patients it was not clearly documented for that episode to be intended as day case. The mean LOS was 0.4 days (median = 0, SD 1.7). Our 2-day readmission rate was 4.95% (n=10) and 30-day readmission 8.4% (n=17), with pain (4.5%, n=9) and dysphagia (3.5%, n=7) the most common reasons for readmission. During the study period, for the four complete calendar years (2015-2018) we demonstrated a statistically significant improvement in our day case rate χ2(n= 174, (p = 0.0036)).
There were 0 conversions to open and 0 mortalities in study period. Two patients had unplanned return to theatre before they met discharge criteria. One for bleeding and one for oesophageal injury requiring transfer to tertiary centre (Table 1). Reasons for delayed discharge included pain (n=2), nausea (n=2) and medical complications (n=2).
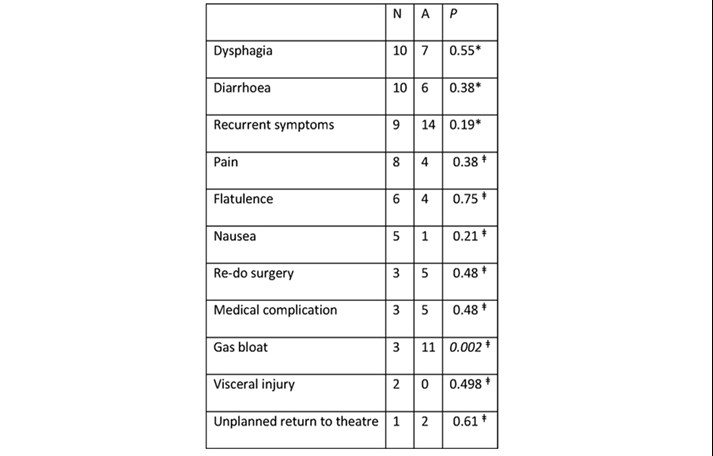
The median follow-up period was 2 years (743 days, min 66, max 1965). 18 patients (8.9%) complained of ongoing dysphagia at clinic review and three had endoscopic dilatation. During the 5-year study period, 24 patients (11.9%) were referred back with recurrent symptoms. The overall revision surgery rate in the study period was 4% (n=8). There were no significant differences in complications between anterior and Nissen fundoplication other than gas bloat (11 (6.9%) vs 3 (2.9%), Fisher’s Exact p=0.002).
Discussion
This study has several limitations. Data regarding patient symptoms were subjective and not measured using validated HRQL questionnaires introducing the possibility of observation bias. Follow-up duration was variable, with those undergoing recent surgery having shorter follow-up. Patients were not randomised introducing the possibility of selection bias. Recurrent symptoms were recorded at clinic review if present or from re-referral in the study period. It is possible that more patients had recurrent symptoms but did not seek medical attention and this was not routinely captured using a validated questionnaire.
Overall, our results indicate the safety and reproducibility of anti-reflux surgery as a day case procedure using a standardised treatment protocol. 86.6% of patients were performed as day case, which is significantly higher than the 15.1% national rate published by Palser et al (2018)17. This also compares favourably to other published series12-15.
In keeping with the experience of1, 12, 13, 17, 20 our operative complication rate was low, but we had a higher than expected rate of early readmissions (Tables 1 & 2). Early readmissions were mainly related to post-operative pain, odynophagia and dysphagia. Our protocol does encourage the use of soluble analgesia at home with a supply of anti-emetic medication to counteract nausea. It is our practice to stop antacid medications on discharge. Despite the early planned telephone follow up and availability of contacting the surgical service out of hours, one third of all readmissions were related to pain (Table 2). The majority of readmissions did not require any intervention other than analgesia at supportive treatment. Early telephone follow up, to maintain patient safety, may lower the threshold at which we review patients in preference to management in the community. Overall, our 30-day readmission rate has improved from 14% in 201618 to 8.4% in 2019.
Table 1.
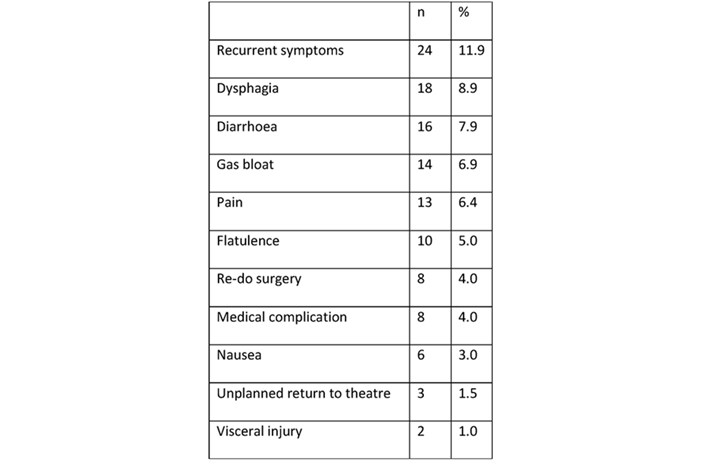
Table 2.
From our discharge data it is possible to see the time of day at which patients were discharged home, with many leaving in the evening. It is important that a day case ward has the staffing and operational hours to facilitate safe discharge up to 220012, 14. Patients undergoing anti reflux surgery can require multiple anti emetics to be able to tolerate oral fluids and time to recover from the process, hence we suggest placing these patients first on the operating list.
Early dysphagia is well recognised complication of treatment for GORD, occurring in a greater proportion of surgically treated than medically managed patients1, but becoming more comparable in the long term1. Overall, our dysphagia rate was 8.9% with three patients requiring endoscopic dilatation (1.5%), comparing favourably to other studies 1, 12, 15.
The long-term efficacy of anti-reflux surgery is well documented 1, 12, 15, 21, 22 but recurrent symptoms and PPI use have been documented in up to 48% of patients6. Review of cases over the study period indicated 11.9% of patients complained of recurrent symptoms and were reinvestigated. 1 patient had early recurrence with incarceration after retching and was re-operated on as an emergency. 7 patients (3.5%) had later revisional surgery. Some authors have reported on revision surgery occurring up to 10 years after first primary surgery22.
In our cohort there was no statistically significant difference in complications between anterior and Nissen fundoplication cases apart from an increase in gas bloat in anterior operations (Table 3). Dysphagia rates were similar between operation types as were readmissions and total complications.
Table 3.
Subsequent to this data set we have continued our protocol and anecdotally continue to have similar results. Despite the potential methodological biases this protocol is likely to have external validity and be reproducible at other centres. Those patients deemed high peri-operative risk by surgeons and anaesthetists may benefit from modified approach and longer period of observation.
Conclusion
Using a standardised peri-operative protocol, patient counselling and early telephone follow up, a day case rate of >80% for laparoscopic anti-reflux surgery is achievable. This is in keeping with the recently published Getting It Right First Time (GIRFT) document for General Surgery.
Conflict of interest statement
There were no funding sources for this study and no conflict of interest declared.
References
- Garg, S.K. and Gurusamy, K.S., 2015. Laparoscopic fundoplication surgery versus medical management for gastro‐oesophageal reflux disease (GORD) in adults. Cochrane Database of Systematic Reviews, (11).
- Galmiche, J.P., Hatlebakk, J., Attwood, S., Ell, C., Fiocca, R., Eklund, S., Långström, G., Lind, T., Lundell, L. and LOTUS Trial Collaborators, 2011. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. Jama, 305(19), pp.1969-1977.
- Watson, D.I., Jamieson, G.G., Pike, G.K., Davies, N., Richardson, M. and Devitt, P.G., 1999. Prospective randomized double‐blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. British journal of surgery, 86(1), pp.123-130.
- Booth, M.I., Stratford, J., Jones, L. and Dehn, T.C.B., 2008. Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro‐oesophageal reflux disease based on preoperative oesophageal manometry. British Journal of Surgery, 95(1), pp.57-63.
- Memon, M.A., Subramanya, M.S., Hossain, M.B., Yunus, R.M., Khan, S. and Memon, B., 2015. Laparoscopic anterior versus posterior fundoplication for gastro-esophageal reflux disease: a meta-analysis and systematic review. World journal of surgery, 39(4), pp.981-996.
- Robertson, A.G., Patel, R.N., Couper, G.W., de Beaux, A.C., Paterson‐Brown, S. and Lamb, P.J., 2017. Long‐term outcomes following laparoscopic anterior and Nissen fundoplication. ANZ journal of surgery, 87(4), pp.300-304.
- Nilsson, G., Larsson, S. and Johnsson, F., 2000. Randomized clinical trial of laparoscopic versus open fundoplication: blind evaluation of recovery and discharge period. British Journal of Surgery, 87(7), pp.873-878
- Ackroyd, R., Watson, D.I., Majeed, A.W., Troy, G., Treacy, P.J. and Stoddard, C.J., 2004. Randomized clinical trial of laparoscopic versus open fundoplication for gastro‐oesophageal reflux disease. British Journal of Surgery, 91(8), pp.975-982
- Bammond, C., 2005. BADS Fellowship report: developing day case Nissen fundoplication. JOURNAL OF ONE DAY SUroeders, J.A., Rijnhart-de Jong, H.G., Draaisma, W.A., Bredenoord, A.J., Smout, A.J. and Gooszen, H.G., 2009. Ten-year outcome of laparoscopic and conventional nissen fundoplication: randomized clinical trial. Annals of surgery, 250(5), pp.698-706
- Salminen, P., Hurme, S. and Ovaska, J., 2012. Fifteen-year outcome of laparoscopic and open Nissen fundoplication: a randomized clinical trial. The Annals of thoracic surgery, 93(1), pp.228-233.
- HRGERY, 15(4), p.89.
- Jensen, C.D., Gilliam, A.D., Horgan, L.F., Bawa, S. and Attwood, S.E., 2009. Day-case laparoscopic Nissen fundoplication. Surgical endoscopy, 23(8), pp.1745-1749
- Khan, S.A. and Stephens, L., 2012. Day-case laparoscopic Nissen fundoplication. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 16(1), p.50.
- Brown, J.J., Bawa, S., Horgan, L.F. and Attwood, S.E., 2013. Achieving day-case laparoscopic nissen fundoplication: an analysis of patient and operative factors. Journal of Laparoendoscopic & Advanced Surgical Techniques, 23(9), pp.751-755
- Mistry, P., Zaman, S., Shapey, I., Daskalakis, M., Nijjar, R., Richardson, M., Super, P. and Singhal, R., 2018. Building a model for day case hiatal surgery-Lessons learnt over a 10 year period in a high volume unit: A case series. International Journal of Surgery, 54, pp.82-85.
- https://gettingitrightfirsttime.co.uk/wp-content/uploads/2018/08/GIRFT-GeneralSurgery-Aug17-O1.pdf. NHS Improvement. Accessed 12.8.19
- Palser, T.R., Ceney, A., Navarro, A., Swift, S., Bowrey, D.J. and Beckingham, I.J., 2018. Variation in laparoscopic anti-reflux surgery across England: a 5-year review. Surgical endoscopy, pp.1-7.
- Javed, O., Maitland, L., Peyser, P., Finlay, I. and Clarke, M., 2017, September. Day-case laparoscopic anti-reflux surgery: experience in Cornwall. In BRITISH JOURNAL OF SURGERY(Vol. 104, pp. 18-18). 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY
- https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. American Society of Anesthesiologists. Accessed 4.5.20
- Barthelsson, C., Lützén, K., Anderberg, B., Bringman, S. and Nordström, G., 2003. Patients’ experiences of laparoscopic fundoplication in day surgery. Ambulatory Surgery, 10(2), pp.101-107
- Galmiche, J.P., Hatlebakk, J., Attwood, S., Ell, C., Fiocca, R., Eklund, S., Långström, G., Lind, T., Lundell, L. and LOTUS Trial Collaborators, 2011. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. Jama, 305(19), pp.1969-1977
- Castelijns, P.S.S., Ponten, J.E.H., Vd Poll, M.C.G., Bouvy, N.D. and Smulders, J.F., 2018. Quality of life after Nissen fundoplication in patients with gastroesophageal reflux disease: Comparison between long-and short-term follow-up. Journal of minimal access surgery, 14(3), p.213.
Appendix
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/40118/303-achieving-success-in-day-case-laparoscopic-anti-reflux-surgery-using-a-standardised-peri-operative-protocol-in-a-cornish-cohort.pdf