Perioperative Care in Hip and Knee Arthroplasty: a summary of recent ERAS Society guidance « Contents
Dr Naomi Ward1, Professor Anil Hormis2
- ST3 trainee in Anaesthesia, The Rotherham NHS Foundation Trust, Moorgate Road, Rotherham S60 2UD
- Consultant in Anaesthesia and Critical Care, The Rotherham NHS Foundation Trust, Moorgate Road, Rotherham S60 2UD
Corresponding author: naomi.ward@doctors.org.uk
In 2019 the Enhanced Recovery after Surgery (ERAS) group published a consensus statement on the perioperative care of patients undergoing lower limb (hip and knee) arthroplasty. (1) Recommendations were formulated by a multi- disciplinary panel of experts in ERAS pathways using a variety of sources and published guidelines from literature searches. We have summarised the guidelines below.
Preoperative care
Patient preparation
Patients should routinely receive preoperative education; this has been shown to reduce patient anxiety, despite not independently affecting postoperative outcomes. (1) There is strong evidence for this intervention. This should be an essential and compulsory component of ERAS pathways, if day case arthroplasty is being considered.
There is some evidence for optimising modifiable patient risk factors. In particular, smoking cessation for at least 4 weeks prior to elective lower limb arthroplasty is associated with fewer adverse outcomes; there is strong evidence for this intervention. (1) There is equally strong evidence for the use of alcohol cessation programmes in patients with high alcohol intake. (1)
Preoperative anaemia should be identified, investigated and corrected prior to surgery; there is strong evidence that this reduces postoperative blood transfusion, readmission and critical care admission, length of stay and overall costs. (1)
Preoperative physiotherapy has been suggested as an intervention to encourage early discharge; there is currently no strong evidence to support this as a recommendation. (1) It may, however, be beneficial in certain patient groups such as the elderly, and those with multiple comorbidities or frailty.
Preoperative fluid and fasting guidance
The intake of clear fluids up until 2 hours before surgery is strongly recommended in conjunction with a 6 hour fast for solid food. (1) This has been shown to have no effect on complication rates and as such is strongly recommended. (1)
The use of carbohydrate loading drinks has been shown to have mixed results; although used other types of major surgery, it is not currently recommended in lower limb arthroplasty patients as an essential routine intervention. (1)
Intra operative care
Anaesthetic considerations
A core component of ERAS pathways is a standardised anaesthetic protocol. In many hospitals, these differ and they are hard to compare.
Choice of anaesthetic technique
The avoidance of routine use of anxiolytic premedication is strongly recommended; this may however be necessary in certain patient groups to facilitate interventions. (1) This would be of particular importance if day case arthroplasty is being considered.
In terms of choice of modern general versus regional anaesthesia, there is no evidence to suggest the routine use of one over the other. (1) However, it is strongly recommended to avoid the routine use of spinal opioids due to concerns over the risks of urinary retention, pruritis and respiratory depression. (1) Similarly, despite the benefits in terms of excellent postoperative analgesia, it is strongly recommended to avoid the routine use of epidural analgesia due to the side effect profile. (1)
Prevention of postoperative nausea and vomiting (PONV)
It is strongly recommended to risk stratify patients for PONV prior to surgery and to treat with escalating classes of antiemetic depending on their risk score. (1) A risk calculator such as the Apfel score can be used; current recommendations are for those with 1-2 risk factors to receive 2 antiemetics from differing drug classes, and in those at higher risk, 3 drugs from differing classes. (2)
Prevention of perioperative blood loss
The use of tranexamic acid (TXA) is strongly recommended to reduce perioperative bleeding and hence the need for perioperative blood transfusion. (1) Studies have found TXA to be safe despite perceived risks of increasing rates of venous thromboembolism (VTE). (3)
Analgesic strategies
In general, the use of multimodal analgesia is recommended as a vital part of ERAS pathways. In particular, the routine use of paracetamol is strongly recommended; as well as reducing postoperative pain scores with a favourable side effect profile, it has also been shown to reduce the incidence of PONV. (1)
The use of non-steroidal anti- inflammatory drugs (NSAIDs) is strongly recommended routinely in patients with an absence of contraindications. (1) Patient groups in whom these drugs should be avoided include those with bleeding tendencies, peptic ulcer disease and renal or hepatic dysfunction.
Gabapentinoids are not currently recommended as part of multimodal analgesia in lower limb arthroplasty; there is a need for further study to evaluate their use. (1)
Despite ERAS programmes in general aiming to keep to a minimum the use of opioids, it is strongly recommended to use them when required as part of the multimodal analgesia programme. (1)
Local anaesthesia
Local anaesthetics can be used both in peripheral nerve blockade and for local infiltration analgesia (LIA). One advantage of LIA over nerve blockade is the avoidance of motor block and hence earlier postoperative mobilisation. This technique is strongly recommended in arthroplasty of the knee, but there is not currently little evidence to suggest its use in hip arthroplasty patients. (1)
Due to the above-mentioned risk of prolonged motor blockade, nerve block techniques are not currently recommended in ERAS lower limb arthroplasty patients. (1)
Other anaesthetic considerations
The maintenance of normothermia is an important component of ERAS pathways. There is a high level of evidence for this, with the UK’s National Institute for Clinical Excellence (NICE) recommending pre- warming and then active warming for all patients undergoing surgery. (1) It is therefore strongly recommended that normothermia is maintained in this way. (1)
Postoperative joint infection in patients undergoing lower limb arthroplasty is a potentially catastrophic outcome that is difficult to treat. As a result, it is strongly recommended that this patient group receives suitable antimicrobial prophylaxis in line with local guidelines. (1)
Hip and knee replacement surgery is associated with an increased risk of venous thromboembolism (VTE). (1) It is therefore strongly recommended that patients are mobilised as soon as possible postoperatively and receive prophylactic treatment according to local guidelines in order to reduce this risk. (1)
Fluid management is an important component of anaesthetic practice. It is strongly recommended that intraoperative fluids are used judiciously, but that they should be discontinued early to allow resumption of oral fluid intake. (1) Electrolyte abnormalities (eg) hyponatremia should be avoided by using intravenous fluids to replace insensible losses only. (1)
Surgical considerations
Differences in surgical technique have been studied as to their potential effect on discharge and complication rates. There is currently no evidence to suggest any one surgical technique as part of an ERAS pathway. (1)
Tourniquets have historically been used in knee arthroplasty to reduce intraoperative bleeding; it has however been demonstrated that this does not reduce total blood loss and may hamper early postoperative recovery. (1, 4) As a result, the avoidance of routine use of tourniquets is strongly recommended. (1) Likewise, the avoidance of routine use of surgical drains is strongly recommended due to the increased risk of blood loss. (1)
The routine use of urinary catheters is not recommended in ERAS patients undergoing lower limb arthroplasty. (1) Where these are necessary, the aim should be to remove as soon as the patient is able to pass urine, and ideally within 24 hours of surgery. (1) Postoperatively, a bladder volume threshold of 800ml should be used to indicate the need for urinary catheterisation. (1)
Postoperative care and discharge
Return to normality is an essential part of ERAS protocols and this encompasses early return to oral nutrition. It is strongly recommended that patients are encouraged to resume normal eating and drinking as soon as possible. (1) There is good evidence for early postoperative mobilisation; it is strongly recommended that this is promoted. (1)
Discharge criteria are an important component of the ERAS pathway and it is strongly recommended that units have a set of objective discharge criteria. (1) They may include the ability to self- care, toilet and dress oneself and independently mobilise. (1)
Conclusion
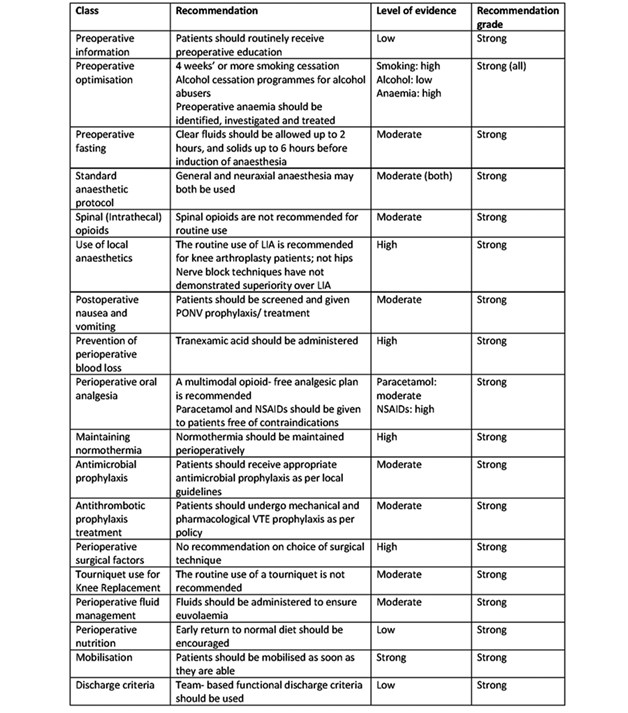
This is a summary of the recommendations from the ERAS Society on the perioperative management of patients undergoing hip and knee replacement surgery. A summary of all the recommendations and the grade of evidence can be found in Table 1. The guidelines are an attempt to summarise a wide range of heterogenous protocols in the literature. We would urge colleagues to read the entire guidance and consider implementation of these components in their ERAS pathways within their arthroplasty units. The aim should be to decrease length of stay (LOS) and in some cases, potentially aim, for day case hip and knee arthroplasty.
Table 1. Summary of ERAS society guidelines for lower limb arthroplasty. Adapted from (1).
References
- Wainwright T, Gill M, McDonald D et al. (2019): Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations, Acta Orthopaedica, 2019, DOI: 10.1080/17453674.2019.1683790.
- Gan T, Diemunsch P, Habib A et al. Consensus guidelines for the management of post operative nausea and vomiting. Anesth Analg. 2014 Jan;118(1):85-113. doi: 10.1213/ANE.0000000000000002
- Fillingham Y, Ramkumar D, Jevsevar D et al. The safety of tranexamic acid in total joint arthroplasty: a direct meta- analysis. J Arthroplasty. 2018 Oct;33(10):3070-3082.e1. doi: 10.1016/j.arth.2018.03.031.
- Zhang, W., Li, N., Chen, S. et al. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res 9, 13 (2014). https://doi.org/10.1186/1749-799X-9-13.
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2020-journal/jods-302-may-2020/perioperative-care-in-hip-and-knee-arthroplasty-a-summary-of-recent-eras-society-guidance
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/37934/302-perioerative-care.pdf