On-The-Day Theatre Cancellations: A Retrospective Study « Contents
Sanjeev Kotecha1 and Achal Khanna2
1 FY2, Oxford University Hospitals NHS Foundation Trust (formerly of Milton Keynes University Hospital NHS Foundation Trust)
2 Consultant Upper GI Surgeon, Milton Keynes University Hospital NHS Foundation Trust
Contact: Sanjeev_Kotecha@hotmail.co.uk
Keywords: surgery, theatre, cancellations
Abstract
Introduction: The aim of this study is to evaluate on-the-day (OTD) theatre cancellations at Milton Keynes University Hospital (MKUH) and to identify the reasons behind these cancellations.
Methods: All patients undergoing elective surgery in the general, colorectal and breast surgery specialties over a six-month period were included. The reasons behind these cancellations were then ascertained using the electronic patient record system. Cancellations were defined as either ‘avoidable’: bed availability, did not attend (DNA), unwell, surgical cancellation, medication issues, not fasted; or ‘unavoidable’: insufficient time, self-cancellation.
Results: Out of 1003 planned procedures, 19.4% (195 patients) were cancelled overall. 40% of cancellations were identified as being OTD (78/195). Of these, 89.7% (70/78) were ‘avoidable’ with the most common reasons being bed availability (27/70) and DNAs (14/70). 10.3% (8/78) of OTD cancellations were deemed ‘unavoidable.’
Conclusions: OTD theatre cancellations account for significant financial burden across healthcare systems worldwide. Their unpredictable nature exacerbates wasted time of theatre staff and resources. The implementation of measures to reduce all kinds of OTD cancellations, especially ‘avoidable’ ones, would lead to increased efficiency and cost-effectiveness.
Introduction
Growing financial pressures on the National Health Service (NHS) and budget constraints mean that running a system that is efficient and economical as possible is essential. Operating theatres comprise a significant proportion of any hospital’s expenditure, which consists of utility bills, equipment, drugs and human resources [1], [2]. One area that has come under scrutiny is the cancellation of surgical procedures. It is well known that these cancellations can occur for a wide range of reasons, both clinical and non-clinical in nature. When procedures are cancelled in advance, it gives departments the opportunity to ensure that available slots are filled. However, cancellations that arise on-the-day (OTD) of any given procedure tend to lead to a waste of hospital resources. Given that these OTD cancellations are inherently difficult to predict, they are responsible for a substantial source of inefficiency in a system that is already fiscally burdened. This project aims to retrospectively assess OTD theatre cancellations at Milton Keynes University Hospital (MKUH) and to determine the reasons behind these cancellations.
Methods
For the purpose of this audit, patients that were booked to undergo elective surgical procedures by the general, colorectal and breast surgical specialties were included. This covers both day case surgery as well as patients requiring inpatient admission pre- and/or post-operatively. Emergency cases were not considered. A six-month period of January – June 2018 was used for patient selection in this study in order to account for any seasonal disparities that may exist in OTD cancellations [3]. Once eligible patients had been identified, the local electronic patient record system was used for data acquisition so that the circumstances leading to the cancellations could be determined.
Cancellations were categorised as being ‘avoidable’ or ‘unavoidable.’ ‘Avoidable’ cancellations include bed availability (i.e. insufficient capacity), did not attend (DNA; implies that the hospital is not notified of non-attendance), unwell (e.g. respiratory tract infection), surgical cancellation (deemed no longer necessary on the day by the lead surgeon or the procedure is cancelled for anaesthetic reasons e.g. further pre-operative assessment is required), medication issues (e.g. oral anticoagulants not being stopped in a timely manner), not fasted (e.g. patient has eaten just prior to their procedure). ‘Unavoidable’ cancellations include: insufficient time (e.g. other cases over-running), self-cancellation (whereby the patient cancels their own procedure but does not inform the hospital until the day of the procedure).
Results
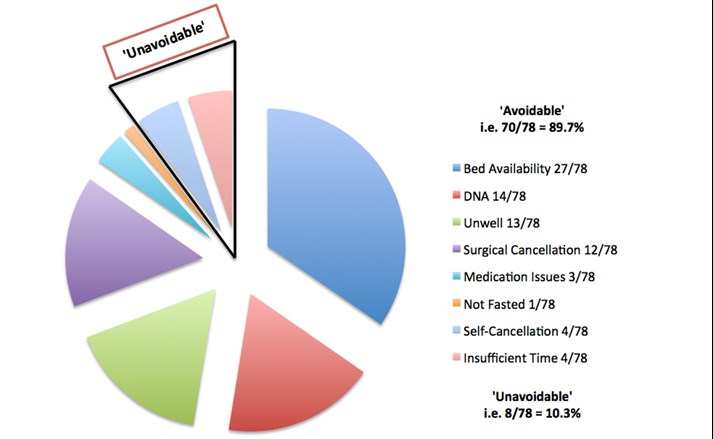
There was a total of 1003 planned elective procedures to be carried out by the above specialties in the six-month period. 19.4% (195/1003) of overall procedures were cancelled, with 40% of these (78/195) being OTD cancellations (Table 1). The nature of the OTD cancellations was assessed to determine whether they were ‘avoidable’ or ‘unavoidable’ (Figure 1). 89.7% (70/78) of OTD cancellations were deemed to be ‘avoidable.’ A lack of available beds was the most prevalent reason, accounting for over a third of all OTD cancellations (27/78). DNAs, the patient being too unwell for surgery as well as a decision by the surgical/anaesthetic team to cancel the procedure were all approximately equal in their incidence, each accounting for 15-20% of OTD cancellations (n. = 14, 13 and 12 out of 78 respectively). 10.3% (8/78) of OTD cancellations were ‘unavoidable,’ with insufficient theatre time and self-cancellations each being responsible for 4 out of the total 8 ‘unavoidable’ OTD cancellations.
Table 1 – Total number of planned procedures per specialty with a breakdown of cancellations (both OTD and total).
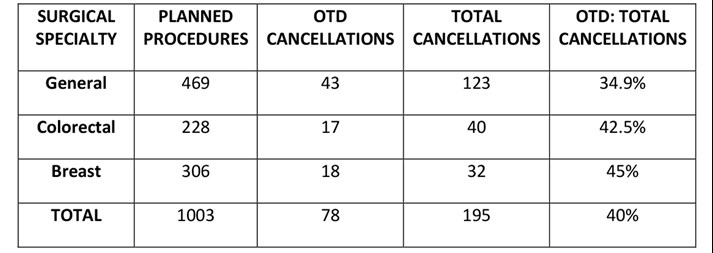
Figure 1 – Pie chart depicting breakdown of ‘avoidable’ and ‘unavoidable’ OTD cancellations.
Discussion
Over the time period surveyed, OTD cancellations represented 40% of the total cancellations of planned procedures at MKUH. In comparison, a 2018 prospective, cohort study examined theatre cancellations over a one-week period across almost 250 NHS hospitals. Approximately 15,000 patients were included and OTD cancellation rate was found to be 13.9%, much lower than in this study at MKUH [4]. When compared with the official NHS England statistics, the overall cancellation rate nationally was 1% for the same six-month period of 2018, compared to 19.4% overall cancellation rate found in this study at MKUH [5]. Data on cancellations that are specifically OTD, is no longer collected on a national scale; instead data on ‘last minute’ cancellations is routinely collated, and this involves a larger subset of patients compared to OTD cancellations. When put into perspective, it is evident that the cancellation rate at MKUH is far less favourable compared to other studies and nationally.
When assessing the reasons behind OTD cancellations, it was found that 89.7% were ‘avoidable,’ with 10.3% ‘unavoidable.’ However, these definitions are certainly equivocal and debatable. Some of the ‘avoidable’ reasons in this study can be regarded as being difficult to prevent. For example, a lack of bed availability could be secondary to a variety of unforeseen factors but addressing this by revising bed space forecasting could make a substantial difference in reducing OTD cancellation rates. DNAs could be improved by better communication between the hospital and the patient (e.g. sending electronic or telephone reminders), and surgical cancellations (by either the surgical or anaesthetic teams) could be improved by establishing local pathways [6]. These three ‘avoidable’ reasons accounted for the majority of all OTD cancellations. Being unwell OTD of surgery cannot be predicted but unless the patient has become unwell within 24 hours of admission, this is another potentially preventable cause for cancellations, again through improved communication between the hospital and the patient. Medication and fasting issues can be targeted through relatively simple measures such as electronic protocols. In terms of the ‘unavoidable’ cancellations, insufficient theatre time often arises due to preceding cases overrunning. Nonetheless, there are times when teams feel as though theatre lists have been over-booked, which is something that can certainly be prevented. Finally, patients calling OTD of surgery to cancel their procedure (self-cancellation) is obviously difficult for hospitals to predict in advance but this could be mitigated in many cases by improved peri-operative communication with patients. Despite being classified as ‘avoidable’ and ‘unavoidable,’ it can be argued that these are all areas worth targeting due to the wide-ranging consequences of OTD cancellations, including: economic, clinical and service-related implications [7].
Given the current economic situation of the NHS, ensuring that all areas of healthcare provision are as cost-effective as possible is essential. A recent study in Finland evaluating the cost of OTD cancellations showed that the average wasted expense for one procedure is around €2,500 [1]. Similar studies in the USA show mean costs that are approximately double this figure [8]. The financial losses incurred are due to a variety of reasons, ranging from wasted time of theatre staff to wasted medications, as well as other wasted resources such as materials and utilities. Additionally, these squandered resources lead to unnecessary harm to the environment. Clinical and patient-related implications are also important to consider. Although these procedures are carried out on an elective basis and may not necessarily be life or limb-saving procedures, patients are forced to endure their symptoms for longer if procedures are cancelled. From a psychological wellbeing point of view, patients have to suffer the stress and disappointment of hearing that their procedure has been cancelled at such short notice [9]. Moreover, there is evidence to suggest surgical outcomes are poorer as a result of OTD cancellations [10]. Service-related implications are another key factor to examine. Not only are these cancellations leading to waiting lists becoming increasingly protracted, but they are also hindering the clinical flow of patients, especially inpatients who have been admitted specifically for their procedure [11].
As far as limitations of this study are concerned, it is important to point out that not all surgical specialties have been considered. Furthermore, despite the sample period being a six-month window (to try and mitigate any disparities that might exist between summer and winter months [3]), the sampling period coupled with a sample size of 1003 patients are relatively small. Ideally the acquisition of data that is similar to that of this study needs to be carried out on a larger scale to truly establish any generalisable trends.
To conclude, the reasons behind OTD cancellations can be complex and multi-factorial. Nevertheless, given the significant consequences that they can have from an economic, clinical and service standpoint, it is crucial to try and improve the rates of theatre cancellations. The often-unpredictable nature of OTD cancellations makes the task more difficult but targeting both ‘avoidable’ and ‘unavoidable’ reasons should be a priority at the forefront of all surgical departments nationally. Plans are in place to try and improve peri-operative communication with patients, through either electronic or telephone reminders, in an attempt to address several causes for OTD cancellations. It would then be prudent to re-evaluate for any discernible and viable improvement, in order to try and create a safer, more efficient and cost-effective service.
Acknowledgements
Dominic Larner (Theatre Information Administrator, MKUH).
References
- Turunen E., Miettinen M., Setälä L. et al.; Financial cost of elective day of surgery cancellations; Hosp. Adm.; 2018; 7(6); pp.30-6.
- Macario A.; What does one minute of operating room time cost? Clin. Anes.; 2010; 22(4); pp.233-36.
- Royal College of Surgeons England; Over 62,000 fewer operations performed this winter, following necessary cancellations; RCS Eng.; 2018.
- Wong DJN, Harris SK and Moonesinghe SR; Cancelled operations: a 7-day cohort study of planned adult inpatient surgery in 245 UK National Health Service hospitals; BJA; 2018.
- Performance Analysis Team; Cancelled Elective Operations; NHS England and NHS Improvement; 2019.
- Olson R.P. and Dhakal I.B.; Day of surgery cancellation rate after preoperative telephone nurse screening or comprehensive optimization visit; Med. (Lond.); 2015; 4(12).
- Caesar U. Karlsson J., Olsson L.E. et al.; Incidences and root causes of cancellations for elective orthopaedics procedures: a single center experience of 17,625 consecutive cases; Patient Saf. Surg.; 2014; 8(24).
- Pohlman G.D., Staulcup S.J., Masterson R.M. et al.; Contributing factors for cancellations of outpatient pediatric urology procedures: single center experience; Urol.; 2012; 188(4); pp.1634-8.
- Leslie R.J., Beiko D., van Vlymen J. et al.; Day of surgery cancellation rates in urology: identification of modifiable factors; Urol. Assoc. J.; 2013; 7(5-6); pp.167-73.
- Magnusson H., Felländer-Tsai L., Hansson M.G. et al.; Cancellations of elective surgery may cause an inferior postoperative course: the ‘invisible hand’ of health-care prioritization? Ethics; 6; pp.27-31.
- Lau H.K., Chen T.H., Liou C.M. et al.; Retrospective analysis of surgery postponed or cancelled in the operating room; Clin. Anesth.; 2010; 22(4); pp. 237-40.
(Click on image to go to the company website.)
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2020-journal/jods-301-february-2020/on-the-day-theatre-cancellations-a-retrospective-study
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/34939/301-kotecha.pdf