Complications for Intra-capsular Coblation Tonsillectomy vs Dissection Tonsillectomy: A local Hospital’s Experience « Contents
N Keates* & J Rainsbury**
*ST3, ENT, Derriford Hospital, Derriford Road, Plymouth, UK
**Consultant, ENT, Derriford Hospital, Derriford Road, Plymouth, UK
Corresponding Author
Natasha Keates Email: n.keates@nhs.net
Abstract
Aims: The aim was to complete a first cycle audit looking at the complication rate for the two procedures and determine whether the new procedure (Intra-capsular Coblation Tonsillectomy) was as safe or safer when compared to current standard management, and as such should be preferable.
Methods: Cases of Coblation procedures for one surgeon were found via coding and the complications determined via E-discharge or patient notes if required. The most recent equal number of dissection tonsillectomies for the same surgeon were also reviewed. We reviewed cases from October 2016 to November 2018. Cases of both procedures were for paediatric patients with an indication of obstructive sleep apnoea (OSA) for tonsillectomy. 52 cases of coblation tonsillectomy were found so 104 were reviewed in total.
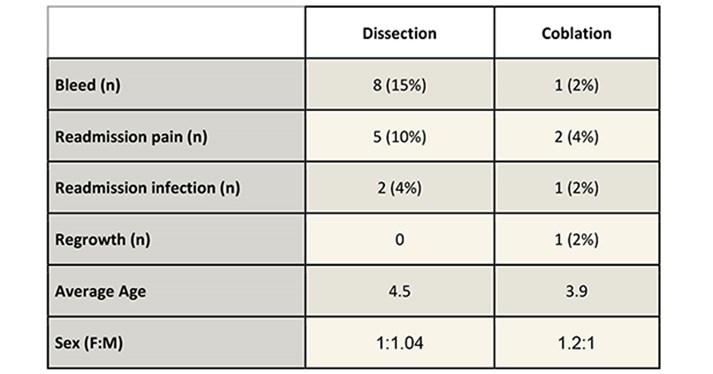
Results: There were 8 bleeds vs 1 for coblation, 5 readmissions for pain vs 2 for coblation, 2 readmissions for infection vs 1 for coblation. The coblation category did show 1 case of tonsil regrowth which was treated with subsequent dissection tonsillectomy.
Dissection: coblation had an average age of 4.5 vs 3.9 respectively. Female to Male ratio was 1:104 vs 1.2:1 for coblation.
Conclusions: Intra-capsular coblation tonsillectomy in this patient group is safer than dissection tonsillectomy with the added possible complication of tonsil regrowth. The complication profile for coblation is reduced which is in the interest of patients and their safety. It also reduced the readmission rate which has ongoing positive cost implications for the department.
Introduction
Tonsillectomy is a common procedure performed for several indications including recurrent tonsillitis, obstructive sleep apnoea (OSA) and occasionally for histological biopsies. It is generally considered to be a safe procedure but with a documented risk of post op bleeds, and an associated return to theatre rate. It is also considered to be a painful procedure post op and patients are generally recommended to take 2 weeks off school or work’ (1).
Evelina have published a case series of intracapsular coblation tonsillectomies, reporting a reduced complication profile in comparison to the more traditional dissection tonsillectomy. They have also reported reduced post op pain and earlier return to school rates1.
Intracapsular tonsillectomies have been offered within Derriford by one consultant for paediatric patients with OSA for the last couple of years.
The aim of this first cycle audit was to compare the current complication profile of the unit’s standard treatment (Dissection tonsillectomy) and compare it to a case series of a new treatment (intracapsular coblation tonsillectomy). So, the treatment with the safer complication profile can be offered to paediatric patients with OSA.
The audit standards were set as the departments current practice. The current audited bleed post tonsillectomy bleed rate, readmission rate and tonsillar regrowth as reported within this audit.
The bleed rate has been noted by the department to be higher than the reported national average. This is however in keeping with the regionally reported bleed rate. Comparison have been made between technique and operator (including grade) with no culpable variation noted. This has contributed to the interest in coblation tonsillectomy with its possible lower complication profile to reduce the rate of post op bleeds/complications and provide safer care for our patients.
Methods
The coding office provided a list of all tonsillectomies regardless of procedure between October 2016 and November 2018 on a single consultant’s theatre list. These dates were chosen to ensure a reasonably sized case series. Cases of coblation were hand searched from the coding list, 52 were found in total. Unclearly coded cases were reviewed with notes (12 in total) but no further coblation cases were found. As this consultant doesn’t perform extra-capsular coblation tonsillectomies we were able to clearly confirm the cases via coding and the online discharge summaries.
This list of patients was then matched by the most recent equal number of dissection tonsillectomies performed on this consultant list.
Inclusion criteria for both procedures were for paediatric patients with an indication of obstructive sleep apnoea (OSA) alone for tonsillectomy. Although trainees will have also performed some of these cases, we did not limit the audit to one operator in order to reflect a real-life complication profile from a multi-operator theatre list. All patients included were from one consultant’s practice.
51 cases of coblation tonsillectomy were found so 102 cases of tonsillectomy were reviewed in total. Statistical analysis was developed using SPSS version 25.
Results
.
Limitations
The reduction in admissions due to pain and infection were not statistically significant (Chi Squared test). The increase in regrowth with coblation was also not statistically significant. The reduction in post op bleeds however was shown to be statistically significant (Chi Squared test) with a P value of 0.015. The groups were compared with an un-paired T-Test which showed that there was no significant difference in the mean for Gender or age.
The groups were not matched but statistical analysis shows no significant difference between the age or gender of the groups. Both groups of patients were from a single consultant’s practice and so reflect the standard variation seen in a consultant’s patient population with regards to proportion performed under supervision by trainees.
Discussion
As is demonstrated from the results table we found that Coblation intracapsular tonsillectomy has a safer complication profile with a statistically significant reduction in post op bleeds. The reduction in re-admission rates was not statistically significant but this may be limited by sample size. The coblation group also showed an acceptably low regrowth rate which is in line with the Evelina case series published (2).
It is important to note that the post tonsillectomy bleeds were universally secondary bleeds with only one requiring intervention. The patient requiring intervention was from the dissection group.
The audit concludes that the complication profile for intracapsular tonsillectomy is reduced compared to dissection tonsillectomy in paediatric patients with obstructive sleep apnoea, when performed by a competent surgeon. With a 13% reduction in post op bleeds and a 7% reduction in readmission due to pain or infection. There is a 2% risk of regrowth in the intracapsular group but this is in line with other studies findings and is acceptable in comparison to the overall risk reduction associated with this procedure.
Following local departmental presentation of this audit the reduced complication profile was considered persuasive and so the other consultants who operate on this patient group have agreed to engage in education and training in order to provide this treatment to their patients.
The outcome will then be re-audited as a unit to see if it has had a wider effect on the unit’s complication rate as a whole.
References
- Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope. 2007;117(4):717‐
- Hoey, AW, Foden, NM, Hadjisymeou Andreou, S, Noonan, F, Chowdhury, AK, Greig, SR et al. Coblation intracapsular tonsillectomy (tonsillotomy) in children: a prospective study of 500 consecutive cases with long-term follow-up. Clin Otolaryngol 2017;42:1211–17
(Click on image to go to the company website.)
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/34941/301-keates.pdf