Day-case hemithyroid surgery – key factors for successful same-day discharge « Contents
Authors
Katharine Davies, Inrid Hinden, Rachel Fletcher & Venkat Srinivasan
Arrowe Park Hospital, Upton, Wirral CH49 5PE
Katharine Davies Specialist Registrar ENT
Ingrid Hinden Foundation Year 2
Rachel Fletcher Foundation Year 2
Venkat Srinivasan Consultant ENT/Thyroid Surgeon
Correspondence: Katharine Davies (07841 125808), c/o Mr Srinivasan: ENT/Thyroid Surgery Department, Arrowe Park Hospital, Upton, Wirral CH49 5PE
Tel: 0151 678 5111 Fax: 0151 604 7403. Email: katdavies33@hotmail.com
Abstract
Introduction: Day-case thyroid surgery isn’t routine practice in many hospitals due to fear of potentially life-threatening complications. This single-hospital study reviewed all patients listed for hemi-thyroidectomy as day-cases over a 26-month period assessing what factor(s) influenced successful same-day discharge.
Methods: We analysed notes of patients listed between October 2012 and January 2015 with special reference to delayed discharge, complications and re-admission.
Results: We performed 95 hemithyroidectomies that had been listed as a day-case (81 females, 14 males), 56% were discharged on the same day. Of the 53 patients who were on the morning lists, 79% were discharged home the same day. Of the 42 afternoon patients only 26% were discharged the same day. No patients were re-admitted with haematoma or bleeding.
Conclusion: We show that day-case hemithyroid surgery can be safely performed without occurrence of delayed bleeding or haematoma. The key factors for successful discharge include adequate time for observation post-operatively, low volume thyroids and the intra-operative use of energy sources for haemostasis.
Key Words: Hemithyroidectomy, partial thyroidectomy, day surgery
Introduction
In the current climate of increasing pressure on the NHS, surgeons are continually reassessing their surgical practice and the surgical procedures that can be managed as a day-case without compromising patient safety. This would not only produce cost benefits but also mean fewer cancellations due to lack of inpatient beds and more resources being available for emergency patients. It has been shown to provide greater patient satisfaction and also reduces the risk of hospital acquired infections. (1) Above all else, patient safety is the most important priority for all day-case surgical procedures and therefore, day-case thyroid surgery can only be advocated if patient safety is ensured. The National Health Service set out the plan in 2000 to try and achieve a 75% day-case rate on elective procedures. (2) The British Association of Day Surgery, in 2001, added that we should be trying to achieve a 50% same-day discharge rate for partial thyroidectomy; however this practice does not seem as common in the UK as elsewhere, as less than 1% of all thyroid cases are done in this manner. (3-6)
The main complications leading to concern about day-case thyroid surgery are: hypocalcaemia, recurrent laryngeal nerve damage and delayed post-operative bleeding leading to airway compression. Post-thyroidectomy haemorrhage associated with laryngeal oedema and airway compromise has been reported to occur after 0.9-2.1% of all thyroidectomies. (5) The major argument against day-case surgery is the prospect of delayed bleeding and haematoma after discharge. (6)
Much of the literature on day-case surgery pools together both hemithyroidectomy and total thyroidectomy cases, whereas in our practice we are advocating hemithyroidectomy only to be performed as a day-case procedure in a carefully selected patient population, and there is inadequate information in this select group to arrive at meaningful conclusions. If only hemi-thyroidectomy procedure is considered for its suitability as day-case, the potential complications would be delayed bleeding and haematoma that can lead to airway compromise and one of the main objectives of this study is to assess the occurrence of these events.
In this retrospective study, we have reviewed the data on a group of patients who underwent planned day-case hemi-thyroidectomies in an attempt to ascertain any factors which enabled or precluded same day discharge.
Methods
A retrospective study was completed on data from all patients who had undergone hemithyroidectomy as a day-case procedure between October 2012 and January 2015. All the patients were appropriately consented with explanation of all possible complications. The prospect of delayed bleeding was particularly mentioned and the need to return to the hospital immediately, in case of neck swelling and bleeding, was emphasised. All patients underwent pre-operative assessment to ensure their suitability for day-case care and had their vocal cord movement checked and recorded when being listed for the procedure (Table 1). Patients were admitted to the day-case unit on the morning of the procedure and once again the possible complications were explained to the patients. A standard hemi-thyroidectomy technique was employed and all through the procedure, energy source (Ligasure, Covidien) was used for dissection and haemostasis. When dissecting closer to the nerve, bipolar diathermy was used. Continuous laryngeal nerve monitoring was used in all cases. Drains were used in most of the cases. A continuous prolene suture with beads at both ends was used to close the external wound; this was removed at their local GP practice a week later. Patients were managed post-operatively on the day-case ward. They were reviewed by the senior author prior to discharge. Those with stable observations for 6 hours and without any complication were considered suitable for discharge home into the care of a responsible adult, after fulfilling the day-case discharge criteria. Patients were followed up in the out-patient clinic around 3 weeks or sooner, if necessary. Chi-squared testing was used to see if there was a significant difference between patients operated on in the morning and in the afternoon.
Table 1: Exclusion Criteria for day case thyroid surgery
Total thyroidectomy
No responsible adults at home to care for 24 hours post-procedure
Patients with no access to a car or phone
Patients unable to follow instructions
Fixed or retrosternal goitre
Metastases
Large Goitres
Patients not fulfilling standard day case criteria - medical reasons
Results
A total of 132 hemi-thyroidectomies were performed, between October 2012 and January 2015, by a single surgeon (VS) with 95 fitting the criteria for day case discharge. Of the 95 patients that were included in the study, 14 were men (mean age 60 years with a range of 41-82) and 81 were women (mean age of 52 years with a range of 18-98). 53 patients (56%) were successfully discharged home on the day of surgery with 42 patients having to remain in hospital for at least one night. The reasons for overnight admission are given in Table 2. Out of the 53 patients operated in the morning lists, 42 were discharged home (79%) the same day as compared to only 11 patients (26%) out of the 42 patients from the afternoon lists (p<0.01). The most common reason for overnight admission in the case of afternoon patients was the lack of observation time available. In some cases, a decision was made during the surgery to keep the patients overnight due to intra-operative findings such as difficult dissection, excessive bleeding or adherence due to inflammation. Medical reasons were mainly relating to delayed recovery including nausea and vomiting. One patient developed haematoma immediately after transfer to the recovery and therefore she was taken back to theatre for exploration and haemostasis. There were no readmissions from the discharged group, due to haematoma or bleeding. One patient was assessed in the emergency department on day 7 and found to have a small seroma. She was reassured and discharged home from the department.
Thyroid size was calculated using the method described by Shabana et al. who multiplied the volume of each lobe by a correction factor of 0.529. This was used as it is not our routine practice to get pre-operative CT scans unless clinically indicated. (7) The thyroid volume was analysed to assess whether this had any impact on discharge. Overall the average thyroid size was 32.8mls. Patients operated on in the morning who stayed at least 1 post-operative day had an average thyroid volume of 50.3mls compared to those who were discharged of 30.8mls. A similar pattern was seen in the afternoon patients with those being discharged home the same day having a thyroid volume of 19mls compared to 33.6mls (see Figure 1). When pooling all the patients together there was a significant difference in size when comparing patients who went home (mean = 26.9, SD= 18.11) and those who stayed (mean = 38.2, SD = 27.5); t (93) = 2.4, p <0.05.
Overall there were 9 complications (9.4%) as documented in Table 3.
Table 2 Reasons for delayed discharge.

Intra-operative findings* - Significant oozing/bleeding, difficult dissection, fibrosis/inflammation
Haematoma** - One patient developed immediately after transfer to Recovery
Figure 1. Thyroid size in units versus outcome
Boxplot showing minimum and maximum values with 25thquartile, median and 75th quartile. * = outlier and diamond = mean
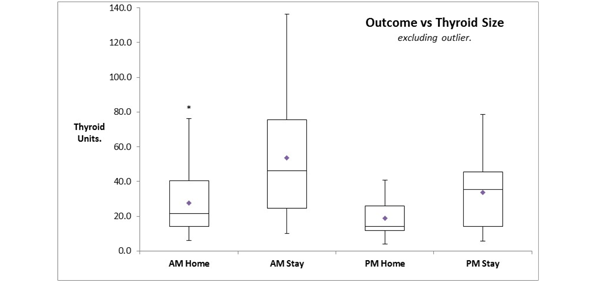
Table 3 Complications.
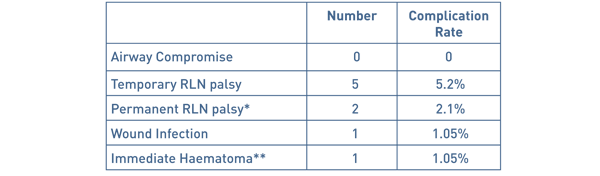
* In one case the nerve was embedded in the thyroid cancer and in the second case, in the level 6 nodes.
** One patient developed haematoma immediately after transfer to the Recovery and had to be taken back to theatre for haemostasis.
This patient is included in the Delayed Discharge group
Article continues after ad.
Discussion
Steckler in 1986 and then Mowschenson in 1995 were the first authors to suggest day-case thyroid surgery and came under intense scrutiny and criticism for advocating this.8,9 Steckler performed 48 hemithyroidectomies as day-case procedures of which 4 were kept in due to intra-operative findings. None of the discharged patients were readmitted with complications. Mowschenson successfully discharged 39 hemithyroidectomy patients home after observation of 6 - 8 hours and also had no re-admissions. Since then it has become increasingly popular in clinical practice, particularly in the USA. Some surgeons favour 23-hour surgery and feel this should be the case until strict criteria for patient selection and better research into who is at risk of post-operative bleeding can be ascertained. (5,10)
The main concerns with day case thyroid surgery are unilateral recurrent laryngeal nerve damage with dysphagia and possible aspiration in some cases, bilateral recurrent laryngeal nerve damage leading to airway compromise, delayed post-operative bleeding and hypocalcaemia.11 Our study concerns only hemithyroidectomies and the relevant factors against day case surgery would be delayed bleeding and haematoma leading to airway compromise. Multiple authors have shown successful day case thyroid procedures without readmission due to bleeding. Teoh et al. performed 50 hemithyroidectomies with a discharge rate of 98%. (12) Symes et al. successfully discharged 73 out of 75 patients within 8 hours of the procedure.13 The other two were kept for medical reasons. Howat et al. and Terris et al. discharged 75% and 83% of hemithyroidectomies home as day case respectively with no readmissions due to haematoma or bleeding. (14, 15)
The surgical techniques have evolved over time particularly for dissection and for achieving haemostasis. The newer technologies, used for haemostasis, have a significant effect in reducing the post-operative bleeding rate. Historically sutures such as silk and vicryl were used for tying the blood vessels with the potential for slippage and consequent bleeding after a few hours. In the recent years, the use of ties has declined and increasingly energy sources such as Harmonic and Ligasure are employed during surgery. Lepner demonstrated that the use of the LigaSure decreased the operation time with lower drain volume, hospital stay and a lower complication rate. (16) This was felt to be due to the fact that LigaSure delivers precise amounts of energy resulting in less thermal damage to the surrounding tissues such as the RLN and parathyroid glands. Multiple papers add weight to the argument that Ligasure decreased the operating time, ensured adequate haemostasis and they had no re-admissions with post-operative haemorrhage.17-20 Inabnet felt that the use of sutureless vessel ligation was superior over older techniques and that the important consideration was meticulous haemostasis of both the upper and lower pole.19 The paper showed that they only had one haematoma within an hour of the operation in a group of 224 patients but it does not mention whether it was a total or partial thyroidectomy. Interestingly, sutures were not used at all for haemostasis in any of the cases in our series.
Currently there is no consensus regarding the optimal duration of observation in the post-operative period, before the patient can be discharged safely. Delayed bleeding, after 24 hours, has been reported, with Leyre et al having 7 bleeds after 24 hours, however, apart from one case these were all total thyroidectomies. (22) Burkey et al looked at 13,817 thyroid and parathyroid surgeries and showed there to be 18 bleeds within 6 hours, 16 from 6 until 24 hours and 8 cases after 24 hours.23 This being the case it argues against even 23-hour surgery and the patient should stay for at least 24 hours but can this really be justified when there is substantial evidence involving high volume of patients, showing large results with no readmissions due to post-operative bleeding? (11,15)
In 1998 Lo Gerfo et al. performed a review of post-operative bleeding over a 20-year period where they identified 21 cases. (24,25) They found that there was a critical period of time in which most bleeding occurred and in all cases the patient showed signs of bleeding within a few hours and the potential for airway compromise was recognised within 4 hours. This supports the early discharge of patients and is mirrored in our results where no patients were re-admitted due to bleeding or neck swelling. In our series one patient developed significant haematoma but this occurred soon after the patient was transferred to the Recovery and this patient was taken back to theatre for haemostasis. It should be noted that none of the patients in our series developed delayed bleeding after transfer back to the ward or after discharge from the hospital.
As in all surgical disciplines, it is difficult to try and predict which patients will have post-operative bleeding, following thyroid surgery. Leyre in 2008 analysed 6830 cases of which 70 had bleeding post-operatively. (22) They found that age, gender and the type of thyroid disease were not related to haematoma formation. They also found that anticoagulation or antiplatelet therapy did not have an influence on bleeding. As regards the timing of the bleeds they found that 37 happened within 6 hours, 26 up until 24 hours and 7 after 24 hours. The majority of these were total thyroidectomies which is not a direct comparison with our study. Looking at their hemithyroidectomy bleeding rates they found that they had 7 (0.4%) within 6 hours, 4 (0.2%) up until 24 hours and 1 (0.06%) after 24 hours. In this paper they do not comment on the haemostatic technique and it could be that the more traditional methods were used.
A parallel can be drawn between day case thyroid surgery and adeno-tonsillectomy. Surgical practice has evolved and changed from the era of keeping adenoidectomy and tonsillectomy patients for several days to the current practice of discharging them on the same day, including the paediatric population. The paper by Leyre et al is quoted by Doran et al as a reason why thyroid surgery should not be done as a day case but when looking at the data and seeing that only 0.3% of all hemithyroid cases had haematoma formation with no further information about these individual cases and the techniques used can it really be the reason to stop all day case thyroid surgery?
Materazzi et al. have devised strict selection criteria for day-case thyroid surgery. (26) Anaesthetic criteria includes ages 10-85, ASA grade 1 or 2, a low intubation score and BMI less than 32. Surgical criteria included primary neck surgery, being euthyroid, gland size less than 80ml and no locally advanced malignancies or intra-thoracic goitres. Social criteria include adequate home support, a suitable living situation and the possession of a telephone. This is a very reasonable selection criteria and is the policy that we adopt with the exception that we do not do total thyroidectomies or children as day case procedures.
We are aware that one of the limitations of our study is the small number but we feel that our series can help arrive at reasonable conclusions, particularly with regard to patient safety. Increasing use of energy sources for dissection and haemostasis has transformed the thyroidectomy surgical procedure in terms of reducing the surgical time and ease of operating. We also feel that the energy sources are helpful in preventing delayed bleeding and haematoma after a reasonable period of monitoring post-operatively. We strongly feel that our number in this study, though small, is adequate to show that with the use of energy sources and adequate post-operative observation time, day-case hemithyroidectomy can be done safely in a selected patient group.
Conclusion
We believe that consideration should be given to perform hemithyroidectomy as day case procedure. Our results have shown that this can be done safely in a reasonable number of patients. We conclude that with careful patient selection and at least 6 hours of post-operative observation day-case hemithyroidectomies can be performed safely. In order to ensure safety, there does need to be strict case selection and thorough information provided to the patients. Our results show that patients operated on the morning lists are more likely to be discharged home on the same day, mainly due to the adequate observation period. It is our opinion that with the use of energy sources for haemostasis and dissection, delayed bleeding can be prevented. In this paper we have shown that with a carefully selected group of patients the overall day case rate can be higher than 50%, as advocated by the British Association of Day Surgery, and can be safely improved upon if operated in the morning. We will continue to audit our practice to assess whether this improved discharge rate continues.
Financial Support
This study received no specific grant from any funding agency, commercial or not-for-profit sectors.
References
- Sahmkow S, Audet N, Nadeau S, Camire M, Beaudoin D. Outpatient Thyroidectomy: Safety and Patients’ Satisfaction. Journal of Otolaryngology- Head and Neck Surgery. Vol 41. No S1 (April), 2012: ppS1-S12.
- Department of health. The NHS Plan. London: DH; 2000.
- Cahill CJ. Basket cases and trolleys - day surgery proposals for the millenium. Journal of one-day surgery. 1999 ,9. 11-12.
- Sahai A, Symes A, Jeddy T. Short-stay thyroid surgery. Br J Surg 2005; 92: 58-59.
- Doran H.E, England J, Palazzo F. Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl 2012; 94: 543-547
- Doran H.E, Palazzo F. Day-case thyroid surgery. BJS 2012;99: 741-743.
- Shabana W, Peeters E, De Maeseneer M. Measuring Thyroid Gland Volume: Should We Change the Correction Factor? AJR: 186, January 2006
- Steckler RM. Outpatient thyroidectomy: a feasibility study. Am J Surg 1986; 152: 417-419.
- Mowschenson PM, Hodin R. Outpatient thyroid and parathyroid surgery: a prospective study of feasibility, safety and costs. Surgery 1995; 118: 1051-1053.
- Mirnezami R, Sahai A, Symes A, Jeddy T. Day case and short stay surgery: the future for thyroidectomy? Int J Clin Prac 2007;61:1216-1222.
- Snyder S, Hamid K, Roberson C, Rai S, Bossen A, Luh J. Outpatient thyroidectomy is safe and reasonable: experience with more than 1000 planned outpatient procedures. J Am Coll Surg 2010; 210:575-584.
- Teoh AY, Tang Y, Leong H. Feasibility study of day case thyroidectomy. ANZ J Surg 2008; 78: 864-866.
- Symes A. et al. Daycase thyroidectomy. Annual meeting of the British Association of Endocrine Surgeons, Lund, Sweden, 2004. (Abstract)
- Howat G, Weisters M, Sames M, Mclaren M. A Pilot Study of Day Case and Short-stay Thyroid Surgery. The Journal of One-Day Surgery (2006) Vol 16, No 1.
- Terris D, Moister B, Seybt M, Gourin C, Chin E. Outpatient thyroid surgery is safe and desirable. Otolaryngology – Head and Neck Surgery (2007) 136, 556-559.
- Lepner U, Vaasna T. LigaSure vessel sealing system versus conventional vessel ligation in thyroidectomy. Scan J Surg 2007, 96 (1) 31-4,
- Lachanas V, Prokopakis, Mpenakis A, Karatzanis A, Velegrakis G. The use of ligasure vessel sealing system in thyroid surgery. otolaryngol head neck surg march 2005 volume 132 number 3 487-489.
- Schiphorst A, Twigt B, Elias S, Dalen T. Randomized clinical trial of LigaSure versus conventional suture ligation in thyroid surgery. Head & Neck Oncology 2012, 4:2.
- Inabnet WB, Shifrin A, Ahmed L, Sinha P. Safety of same day discharge in patients undergoing sutureless thyroidectomy: a comparison of local and general anaesthesia. Thyroid 2008; 18: 57-61.
- Seybt MW, Terris D. Outpatient thyroidectomy: experience in over 200 patients. laryngoscope 2010; 120: 959-963.
- Rosenbaum MA, Harida M, McHenry C. Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg. 2008 Mar; 195 (3): 339-43.
- Leyre P, Desurmont T, Lacoste L, Odasso C, Bouche G, Beaulieu A et al. Does the risk of compressive haematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg 2008; 393: 733-737.
- Burkey SH, van Heerden JA, Thompson GB, Grant CS, Schleck CD, Farley DR. Re-exploration for symptomatic haematomas after cervical exploration. Surgery 2001; 130:914-919.
- Lo Gerfo P, Gates R, Gazetas P. Outpatient and short-stay thyroid surgery. Head Neck 1991; 13: 97-101.
- Schwartz AE, Clark OH, Ituarte P, Lo Gerfo P, Therapeutic controversy: thyroid surgery – the choice. J Clin Endocrinol Metab 1998; 83: 1097-105.
- Materazzi G, Dionigi G, Berti P, Rago R, Frustaci G, Docimo et al. One-day thyroid surgery: retrospective analysis of safety and patient satisfaction on a consecutive series of 1,571 cases over a three year period. Eur Surg Res 2007; 39: 182-188.
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2019-journal/jods-291-february-2019/day-case-hemithyroid-surgery-key-factors-for-successful-same-day-discharge
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6103/291-davies.pdf