A successful revolution in day case breast surgery « Contents
Authors
Dr Alexandra Humphreys Specialist Registrar in Anaesthesia
Dr William Hare Core Trainee in Anaesthesia
Miss Jacqueline Rees-Lee . Consultant Oncoplastic Breast and Plastic Surgeon
Mr Michael Green Consultant Breast and Oncoplastic Surgeon
Dr Mary Stocker Consultant Anaesthetist
Torbay and South Devon NHS Foundation Trust, Torbay, United Kingdom.
Abstract
Introduction: The British Association of Day Surgery (BADS) recommends that 95% of conservative breast cancer surgery and 50% of mastectomies for breast cancer are performed as day case.
Despite Torbay Hospital being one of the top performers in the country for day case rates for most procedures, in January 2015 we were ranked in the lowest quartile nationally for day case rates for breast cancer surgery.
We present our strategy for revolutionising our day case breast surgery service.
Methodology: A multidisciplinary team developed day case pathways for patients undergoing breast cancer surgery. In January 2015 the pathway for conservative surgery was introduced. The pathway for mastectomies was introduced in January 2017.
Results: Between 1st January 2015 and 30th September 2017, the day case rates for conservative surgery improved from 16.5% to 97.8%. During the same time frame, the rates for mastectomies improved from 0% to 85.7%.
Between 1st October 2015 and 30th September 2017, 350 procedures were successfully performed as a day case. Follow up data exists for 288 (82%) of these patients; 100% of these patients were satisfied with the day surgery service provided.
National benchmarking for day case rates now rank us as 14th for mastectomy, 3rd for wide local excision of breast tissue and 2nd for sentinel lymph node biopsy.
Conclusion: By introducing these pathways, we have revolutionised our service, achieved the BADS day case targets and are now one of the top performers nationally.
Introduction
Performing breast cancer surgery as a day case procedure is safe, and is well tolerated by patients (1). Patients undergoing breast cancer surgery experience less psychological distress when treated as a day case patient, as opposed to an inpatient (2).
The British Association of Day Surgery (BADS) directory of procedures recommends that 95% of conservative breast cancer surgery and 50% of mastectomies for breast cancer are performed as day case (3).
Torbay Hospital has an outstanding day surgery unit (DSU), and is one of the top performers in the country for day case rates for most procedures. However, in January 2015, the day case rates for breast cancer surgery were significantly below average. Over the previous 12 months, only 16.5% of patients undergoing breast conservative cancer surgery, and 0% of patients undergoing mastectomies, were performed as day case. At the time we were ranked in the lowest quartile nationally for day surgery rates for all benchmarked breast cancer procedures (4). Day case pathways existed for many other procedures, but not for breast surgery, and so the decision was made to develop two separate pathways for patients undergoing breast cancer surgery, these being conservative breast procedures or mastectomies.
We shall herein describe the process by which we transformed our day case breast surgery processes, and the results that we have achieved.
Methodology
We convened a multidisciplinary team consisting of medical and nursing staff from both the breast-care and DSU. Together, we developed the ideal pathway for day case breast cancer patients. Key to this was shared learning between the teams, both of whom had invaluable expertise essential for the development of a successful pathway. In January 2015, we introduced the pathway for conservative breast cancer surgery. This included procedures such as wide local excision of breast, sentinel lymph node biopsy and axillary clearance, but did not include mastectomy surgery. In November 2016, the team went to the ‘Breast Surgery as Day Surgery’ conference, a joint conference run by BADS and Healthcare Conferences UK. Here, the team found out about the best practice across the country, in particular day surgery mastectomy pathways; this gave us the incentive to further develop our day case breast cancer pathways to include mastectomies. We introduced the day case pathway for mastectomies in January 2017.
Patients undergoing breast reconstruction were not included in the pathways nor dataset discussed here as this surgery is unlikely to be undertaken on a day-case basis.
Pathways
Although the pathway for breast conservative surgery is distinct from the pathway for mastectomies, both share salient features, and so they will be discussed as one here.
Pre-surgery
The day surgery pathway begins with a ‘one-stop’ clinical process. The surgical team see and consent patients in a dedicated ‘results clinic’. Once a decision has been made they complete the consent process and are automatically allocated to a theatre list as a day case.
The breast care nurses then see each patient. Patients receive information leaflets, and education about analgesia, mobility and nutrition. Where relevant, patients receive education on drain management; this is demonstrated to them, together with advice about how to look after the drain. Patients are also fitted with a support bra to be worn day and night post-operatively, and mastectomy patients are fitted for a prosthesis.
Patients then go immediately from the surgical clinic to the day surgery pre-operative assessment clinic. Our experience has shown that having pre-operative assessment provided by specialist day surgery pre-operative assessment nurses is essential for ensuring patients are adequately prepared for their day surgery pathway. A senior day surgery anaesthetist is available to directly support the nurses when more complex decisions are needed.
Day of surgery
Patients are admitted via the surgical admissions ward. Localisation procedures (wires, skin marks and radioisotope injections) are scheduled as part of the pathway to minimise theatre delays. Preoperative analgesia with paracetamol is routine. Anxiolytic pre-medication is not given.
We anesthetise patients using techniques that give a rapid onset and offset with a clear-headed emergence; in this unit, we use total-intravenous anaesthesia for the majority of patients. Patients receive generous infiltration of local Levobupivicaine at the surgical site. Surgical drains are only inserted if deemed absolutely vital; their insertion is the exception, not the rule.
Recovery staff in the DSU provide immediate post-operative care. DSU staff have been trained by the breast care unit specifically with regards to drain management, dressings and appropriate bras. Discharge from the DSU is nurse led. The breast care nurses are available to provide support to DSU if needed.
DSU staff discharge all patients with analgesia, 24 hour contact information and wound care advice. If a drain has been inserted then, DSU staff give patients an information booklet, drain bags and appropriate waste bin, and organise drain removal.
Post-operative
On discharge from the DSU, patients are given a telephone number to call in case of concerns. During 0800-2000, this reaches the DSU discharge ward; out of hours, patients are directed to the clinical site manager. Here, advice is given and the relevant teams are contacted if re-admission is required.
DSU staff make a telephone call to all patients on the first day post operation. The call assesses general wellbeing, pain, nausea and other symptom, and advice is given for any specific problems. Patients are signposted to the breast care nurses if any psychological concerns are identified. Any patients that have been discharged with a drain in situ are telephoned by the ‘medical admissions team’ (a service run by the hospital providing care to patients at home) daily until the drain is removed.
Patients have open access to contact the breast care nurses., who run daily ‘drop-in’ clinics. The breast care nurses provide ongoing support if patients are experiencing post-operative complications.
Patients attend a wound clinic appointment on day five post operation. After discussion in the MDT, patients attend a post-op results clinic with further wound check.
The success of our new pathways were evaluated by analysis of day case rates published by national organisations (NHS Digital and NHS Model Hospital). We also analysed our trust data collected via our in house electronic patient record system Galaxy Surgery Ócsc to ascertain further detail of day case rates, unplanned admission rates and post-operative patient outcomes.
Article continues after ad.
Results
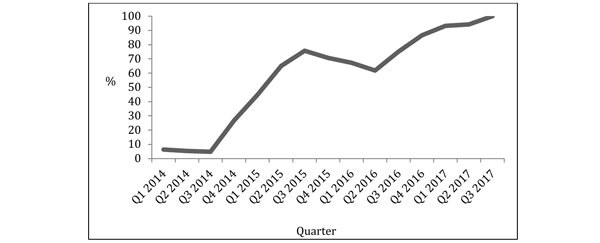
Breast conservative surgery
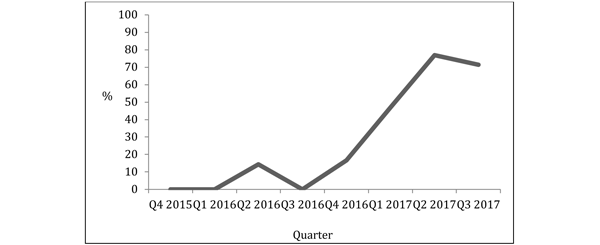
We obtained data for breast care rates from the Clinical Indicators provided by NHS Digital (4). These rates represent the overall day case rate over the preceding 12 month period. On 1st January 2015, the rate of patients undergoing breast conservative cancer surgery as a day case in the previous 12 months was 16.5%. By 30th September 2017, this had risen to 91.4%. Analysis of our trust data for the last quarter of this time period showed rates had risen to 97.8%.
We are now ranked 2nd out of 130 acute trusts for our sentinel lymph node day case rates, and 3rd for our wide local excision of breast tissue day case rates (4).
Figure 1: Rate of patients undergoing wide local excision as a day case per quarter.
Unplanned admission for breast conservative surgery
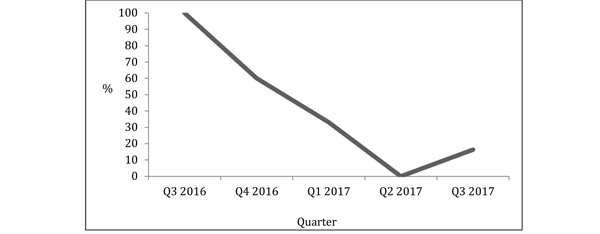
Between 1st October 2015 and 30th September 2017, we performed 404 breast conservative cancer surgeries. 352 of these were booked as a day case. 36 of these patients that were intended to be day case were admitted on the day of surgery, giving an unplanned admission rate of 10.2%. By the last quarter of this time frame, the unplanned admission rate had reduced to 2.2%.
Figure 2: Rate of unplanned admissions for all breast conservative cancer surgery per quarter.
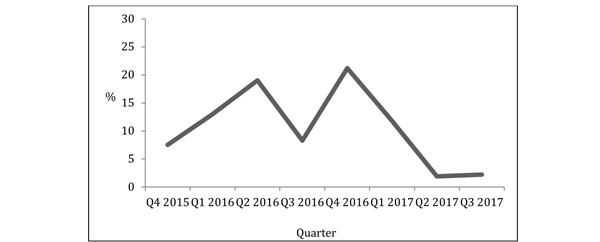
The unplanned admission rate was highest for axillary dissection, with 2 out of 6 patients undergoing this procedure being admitted.
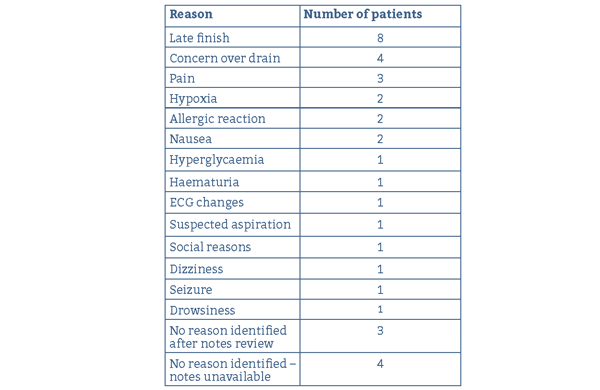
The most common reasons for admission were late finish (8 patients) and concerns about the drain (4 patients). Other reasons for admission included complications such as anaphylaxis and seizures.
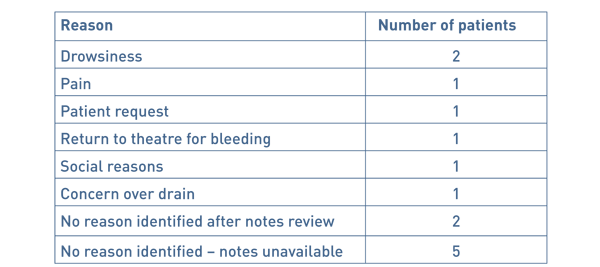
Table 1: Reasons for admission for conservative breast cancer surgery.
Mastectomies
On 1st January 2015, the rate of patients undergoing a mastectomy for breast cancer as a day case in the previous 12 months was 0%; by 30th September 2017, this had risen to 52.4%. During the last quarter of this time period it had risen to 71%, and during the last month it had risen to 85.7%.
We are now ranked 14th out of 130 acute trusts for our mastectomy day case rates (4).
Figure 3: Rate of patients undergoing mastectomy for breast cancer as a day case per quarter.
Unplanned admission for mastectomy
Between 1st October 2015 and 30th September 2017, we performed 130 mastectomies for breast cancer. 48 of these were booked as a day case. 14 of these patients that were intended to be day case were admitted on the day of surgery, giving an unplanned admission rate of 29%. By the last quarter of this time frame, the unplanned admission rate had reduced to 16.6%.
Figure 4: Rate of unplanned admissions for mastectomy for breast cancer per quarter.
The most common reasons for admission was drowsiness (2 patients). Other reasons included social reasons and return to theatre.
Table 2 Reasons for admission for conservative breast cancer or surgery.
Demographics and post-operative outcomes for successful day case patients
350 procedures were successfully performed as a day case.
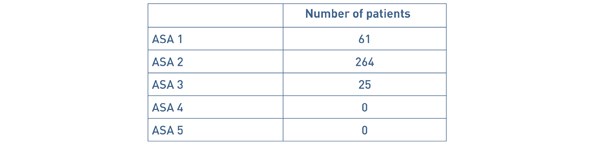
The area served by our hospital has a high proportion of elderly people; 31.00% of the local population are aged 70 years and over, compared with a national average of 25.23% (4). The age of patients that were successfully treated as a day case ranged from 23 – 99 years. 35 patients were aged 80 years and over. ‘American Society of Anaesthesiologists Physical Status Classification’ (ASA) status is shown in Table 3. Our DSU has no cut off for age, ASA or BMI of patients that may be performed as a day case.
Table 3: ASA status of patients successfully managed as a day case.
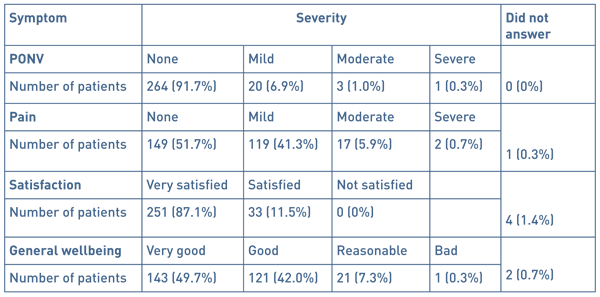
We attempt to contact all patients the day after surgery by telephone. We were able to contact 288 (82%) of the patients. Post-operative symptoms are shown in Table 4.
Table 4: Post-operative symptoms reported by patients.
Discussion
BADS recommends that we should perform 95% of breast conservative surgeries and 50% of mastectomies as day case. By introducing these pathways, we have vastly improved the proportion of patients achieving successful day case surgery for breast cancer. We have exceeded these targets and have improved from one of the poorest performing trusts nationally to one of the top performers. Our comprehensive data shows that this has been safe and that the greater majority of patients are satisfied with their care taking place in a day case environment.
In addition to the recognised benefits to patients, there are benefits to the trust. This pathway has been one of the contributing factors to enabling the trust to close an entire female surgical ward with huge associated financial savings. We also have the ability to continue elective work despite winter pressures of lack of beds and cancellation of all elective surgery. Our patients therefore have a reduction in the risk of cancellation.
Staff involved with the care of these patients feel that there are several aspects that have made the transition work well. This includes the ability to access DSU from the inpatient theatre suite. A significant number of our patients undergo their surgery through our inpatient operating theatres, due to insufficient capacity to meet all our demand in the DSU, coupled with the need to efficiently utilise main theatre time. Patients undergoing surgery in inpatient theatres can transfer to DSU as soon as possible from primary recovery, and then reap the benefits of the DSU. The hard work and commitment from the breast care nurses is invaluable in enabling patients with drains to be managed at home, as well as giving confidence to a vulnerable group of patients. A robust support system with all patients being telephoned post operatively, as well as the ability for all patients to receive rapid access to hospital care if needed, has added to the success. Confidence in staff and hence patients that complications in this type of surgery are rare has helped the transition.
The team feel that the most difficult part of the transformation was the management of patient expectations. The work of the breast care nurses has, again, been invaluable helping this and therefore in enabling the pathways to succeed. Drain management for outpatients was an additional hurdle. Thanks to the support from the breast care nurses, we have been able to insert drains as needed, and have found that discharging patients with drains in situ is safe and acceptable.
Conclusion
By introducing a pathway for patients undergoing conservative breast cancer surgery, and a pathway for patients undergoing a mastectomy for breast cancer, we have dramatically improved our day case rates. Our rates for day case breast surgery are now comparable to our day case rates for most other procedures, whereby we are one of the top performers in the country. We have demonstrated that breast surgery as a day case procedure reduces cost and risk of cancellation, is safe, and that patients treated on our pathways have a high level of satisfaction.
References
- Marla, S, and Stallard S. Systematic review of day surgery for breast cancer. Int J Surg 2009;7:318–323
- Margolese, R, and Lasry, J. Ambulatory surgery for breast cancer patients. Ann Surg Oncol 2000; 7(3):181–187
- British Association of Day Surgery. BADS Directory of Procedures, 5th edn. London: BADS, 2016.
- NHS Digital Clinical Indicators. https://previewer.digital.nhs.uk/ Accessed 15/03/2018.
Acknowledgments
The authors wish to thank the breast care nurses at Torbay Hospital for their advice and support in the writing of this paper.
Funding
None declared
Conflict of interest
None declared
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2019-journal/jods-291-february-2019/a-successful-revolution-in-day-case-breast-surgery
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6102/291-humphreys.pdf