The Postoperative Carer: A Global View and Local Perspectives: Dr Johannes Retief, Dr Rachel Morris & Dr Mary Stocker « Contents
Authors
Dr Johannes Retief Anaesthesia Registrar, Department of Anaesthesia and Perioperative Medicine, Torbay and South Devon NHS Foundation Trust, Lowes Bridge, Torquay, TQ2 7AA.
Email: jretief@nhs.net Tel: 07919 363 563
Dr Rachel Morris Consultant Anaesthetist, Department of Anaesthesia, Norfolk and Norwich University Hospitals NHS Foundation Trust, Colney Lane, Norwich, NR4 7UY.
Email: rachel.morris@nnuh.nhs.uk Tel: 01603 286 286
Dr Mary Stocker Consultant Anaesthetist, Department of Anaesthesia and Perioperative Medicine, Torbay and South Devon NHS Foundation Trust, Lowes Bridge, Torquay, TQ2 7AA
Email: mary.stocker@nhs.net Tel: 01803 654 159
Keywords: Postoperative carer, 24-hour care, day case discharge
Abstract
Introduction: Having a responsible adult with you for 24 hours after day surgery remains an absolute eligibility criterion for day surgery in the large majority of centres. However, with advances in anaesthetic and surgical techniques, as well as a shortage of inpatient capacity, this is increasingly being challenged for some patients. We reviewed the literature available and present a summary of our findings. We also describe two alternative options to inpatient care for those patients who are not able to provide their own carer.
Methods: A MEDLINE database search was performed. Guidelines from different anaesthesia bodies were obtained from their respective websites. Archives from the Journal of One Day Surgery were also searched. Practical solutions are described which have been pioneered in the units where the authors work.
Results: Guidelines from five different anaesthesia bodies, seven studies utilising patient questionnaires or surveys, three surveys of practice and three review or other articles are discussed. Two examples of managing patients with no carer is available are also described.
Conclusion: There is a wide variation in practice in this area of day surgery, both in terms of what the patients choose to do (despite instructions) and what different departments recommend. Day surgery units should have dynamic policies in place and seek innovative solutions when faced with patients who do not have overnight care.
Introduction
Having a responsible adult with you for 24 hours after day surgery remains an absolute eligibility criterion for day surgery in the large majority of centres. However, with advances in anaesthetic and surgical techniques, this is increasingly being challenged for some patients. Also, in the current climate of bed shortages in United Kingdom (UK) hospitals alternative arrangements need to be found to for patients without 24-hour care at home. We reviewed the literature available and present a summary of our findings. There is no conclusive evidence about whether a carer is needed postoperatively and for how long. We also describe two different local practices that are in place for patients who are not able to provide their own carer. In one centre, overnight care can be arranged for patients who are not able to provide family or friends to stay with them. In the second example, overnight care is no longer mandated for certain eligible patients, should they be unable to provide a carer. Day surgery units should have dynamic approaches when faced with patients who do not have overnight care. Clarification of terminology between carer and escort is important. An ‘escort’ generally refers to a person who accompanies the patient from the hospital to their home. Unless specified, this differs from the ‘overnight carer’ or ‘postoperative carer’, who is the person that stays with the patient overnight or for 24 hours. We mainly consider the latter but, as there is often some overlap, literature regarding patient escorts will be considered when relevant.
Methods
Searches of the MEDLINE database and archive of the Journal of One Day Surgery were conducted using a wide variety of search terms which encompassed day surgery, carer, responsible adult and care at home. In addition, guidelines from a range of international and national anaesthesia bodies were obtained directly from their respective websites. Examples of practice described are from the authors’ units with previously unpublished data presented. These results have been previously presented at British Association of Day Surgery (BADS) Annual Scientific Meetings [1, 2].
Results
The literature review on this subject can broadly be divided into four categories:
- National and international guidelines
- Patient questionnaires and surveys
- Surveys of practice
- Review and other articles
Each of these will be considered in turn below. We also describe two different approaches employed by day surgery units for patients who are not able to provide their own overnight care.
National and international guidelines
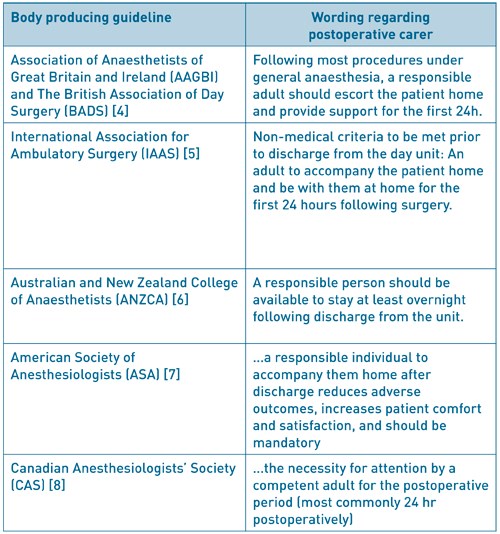
Table 1 gives an overview of guidelines from several countries. In general, a carer postoperatively is still recommended. However, the arbitrary time frame of 24 hours is not universally mandated. The Royal College of Anaesthetists (RCOA) produce Guidelines for the Provision of Anaesthesia Services (GPAS) [3]. In the chapter regarding provision of anaesthesia services for day surgery, it is interesting to note the following statement: “A carer may not be essential if there has been a good recovery after brief or non-invasive procedures and where any post-operative haemorrhage is likely to be obvious and controllable with simple pressure”. This, together with the word ‘most’ in the joint Association of Anaesthetists of Great Britain and Ireland (AAGBI) and British Association of Day Surgery (BADS) guidelines [4] gives some indication that a blanket rule may not be appropriate for all patients.
Table 1: Guidelines pertaining to day surgery for different countries and extracts from sections
regarding the postoperative carer
Patient questionnaires and surveys
Fahy and colleagues investigated the practicality of conducting post-anaesthetic follow-up by questionnaire [9] after finding that interviewing patients was expensive and difficult. With a 96% response rate, this was shown to be a useful research tool and has been used extensively in the day surgery population since. Ogg, a founding member of BADS, utilised a patient questionnaire to gauge patient outcomes 48 hours after day surgery [10]. Unfortunately, it did not specifically ask about an overnight carer. However, of interest is that 31% of patients made the journey home alone with 9% of patients driving themselves. 30% and 43% drove within 12 and 24 hours respectively.
A Canadian telephone survey of 750 day surgery patients [11] found that although all patients were escorted out of the hospital, 29 patients (4%) had no one staying with them overnight. However, there is no information regarding whether these patients had any problems in that period. This was followed by a telephone survey in the UK regarding compliance with post-operative instructions [12]. 240 patients at three different hospitals were telephoned at 24 to 48 hours postoperatively. Although all the patients were discharged into the care of a responsible adult, 32 patients (13.3%) failed to have a carer for 24 hours and three patients (1.3%) spent the night alone. From one centre, the mean time a carer spent was 19 hours. They raised the issue that there were few guidelines on the role of the carer or how much supervision was required. They also recommended that further studies need to establish the necessity of 24-hour care post-operatively.
Another telephone survey looked at the issue of how long a carer stayed post-discharge and explored the patients’ views on the subject [13]. The data was analysed according to procedure complexity, stratified according to anticipated pain score. There was a stepwise increase in the time it took for patients to feel ‘safe’ as the complexity increased, with a statistically significant increase in the time taken to feel safe between the ‘no anticipated pain’ group and ‘severe anticipated pain’ group. They enquired after the patients’ opinion of the 24-hour recommendation (Table 2). Overall, 59% of patients felt the 24-hour recommendation for a carer was ‘about right’. However, when analysed according to expected pain levels (reflecting procedure complexity), it is clear that patients with expected pain of moderate or severe may in fact feel that 24 hours is not enough. This was not the case in those with expected pain of ‘none’ or ‘mild’ many of whom felt that the requirement for 24 hours postoperative care was too long.
Table 2: Patients opinion of the 24-hour recommendation, grouped according to expected pain levels
(based on procedure complexity and experience).

Adapted from: Barker J, Holmes K, Montgomery J, et al. How long is 24 hours? A survey of how long a carer stays with the patient post discharge. Journal of One-Day Surgery. 2014. 24(2): 57-60.
A further study utilised postal surveys to evaluate the compliance with 24-hour adult supervision and found an overall non-compliance rate of 18% (62 out of 351 patients) [14]. The length of time the carer stayed in this case varied, with 9 patients admitting the carer stayed for less than one hour. 15 patients (4%) experienced problems which required medical help but only two of these patients said they needed the carer to obtain the help (to contact ambulance or general practice (GP) services). They also asked about the patients’ attitudes towards having a carer stay with them (see Table 3). Overall only 30% felt it was ‘essential’. However, of those that required help with daily living (99/351; 28%), 63% felt it was essential. A large proportion of patients liked having someone with them but were of the opinion that they “would have been fine on my own”. 10% of patients felt that it was either “a waste of my carer’s time” or “I would rather have been on my own”.
Table 3: Patients answers to the question: “How did you feel about having an adult stay with you
for 24 hours after surgery?”.
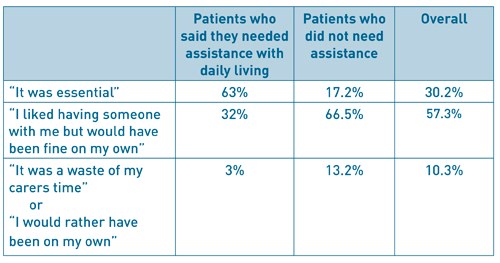
Adapted from: Wessels F, Kerton M, Hopwood H. Evaluating the need for day surgery patients to have 24 hours of adult supervision postoperatively. Journal of One Day Surgery. 2015. 24(4): 17-23
In 2014 the Norfolk and Norwich University Hospital surveyed 100 day case patients over a 2-week period by questionnaire, with a 64% response rate [2]. The two main aims were to gather information about how many patients, who might be safe at home alone, do not have a carer available and whether patients felt they would need assistance at home after their surgery (and if so, why). Laparoscopic and airway surgery patients were excluded as it was felt they would not be safe at home alone after surgery. Paediatric patients were also excluded. 8 responses were excluded (unplanned admissions, laparoscopic surgery and 1 blank form). The survey showed that the majority of the remaining surveyed patients (66.6%) had a carer for at least 24 hours and 33.3% did not. One of the questions asked was ‘whether the patients felt they needed assistance at home postoperatively?’ 59% of patients felt they would need a carer present after surgery. However, the main reason patients wanted assistance at home was for support, with no anaesthetic or surgical complications reported. 41% felt they did not need assistance at home post operatively. 5 of the patients surveyed lived alone and 4 of them said they would not need assistance. The one patient that said they needed assistance had lower limb metal work removal and found mobilisation difficult. Two patients who had eye surgery both felt they needed assistance due to impaired vision. This was taken into account when writing the self-care pathway. The survey confirmed that patients were making decisions about how much care they felt they needed postoperatively. This is in line with the evidence presented in the rest of the article. The vast majority of patients want and are able to arrange someone to be present for the following 24 hours after discharge. However, some patients do not and therefore a Self-Care Pathway was designed, discussed below.
Surveys of practice
A survey of Canadian anaesthetists with 774 replies (57.8% response rate) found that 11.2% would anaesthetise a patient despite knowing the patient had no escort [15]. It is unclear whether they would then expect the patient to be admitted but some of those in this group did add that they would only agree if a patient signed a release form. An international survey of 100 centres in 8 European countries had a response rate of 70% [16]. Routine demand for an escort varied widely between countries, from 36% to 100%. Routinely securing someone to be at home for the first post-operative night was done by 81% of centres but ranges from two thirds to 100%. Despite contacting the authors, we were unfortunately not able to get the UK specific data for this particular area of practice. The same group sent questionnaires to all 92 hospitals in Sweden, particularly looking at the clinical practice and routines for day surgery [17]. In this survey, 27/73 units (37%) did not insist on an escort at discharge but it did not report on the requirement for 24-hour, or overnight, care.
Review and other articles
In 2009, Ip and Chung examined the most recent findings as to whether an escort after ambulatory surgery is a necessity or luxury [18]. Although the term escort is used, they make the point that ‘the role of an escort should be more than merely providing the patient with the ride home’. They recommend that patients without an escort should either be rescheduled or admitted to a 23-hour care bed post-operatively.
In a summary article by Abdullah and Chung regarding discharge criteria for ambulatory surgery [19], citing three malpractice cases of car accidents after ambulatory surgery [20], they recommend that patients should be made aware of the importance of having a responsible adult escort them home and stay with them overnight.
A prospective study [21] over a 38-month period collected data on patients with no escort at a day surgery unit in Toronto. They defined ‘no escort’ as not having a responsible individual to accompany the patient home. Out of 28,391 patients, 60 patients (0.2%) had no escort. They identified two groups in this cohort: those who were known to have no escort (24 patients) and those whose escort did not show up (36 patients). Five of these patients had their surgery cancelled but the remainder underwent surgery. Those with no escort were offered admission but if this was not possible, risks were explained and a self-discharge form signed. Of note, 28.2% of those with no escort also had no overnight care. Outcomes of the no escort group were compared to a matched control group that did have an escort and no differences were found in rates of unanticipated admission, emergency visits or readmission within 30 days.
Alternative solutions to inpatient care for patients without home care
Patients who do not have overnight care available, for example from family or friends, are often admitted to hospital overnight. Not only does this incur cost to the trust and occupy an inpatient bed, a precious resource in the current climate, but patients are not able to reap all the benefits that day surgery provides. In addition, the vast majority of patients would prefer to recuperate in their own surroundings if at all possible.
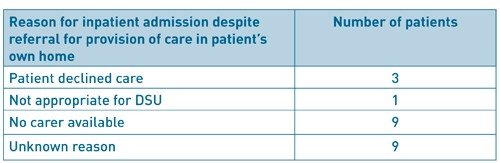
The Torbay Experience: Provision of a carer
In the Torbay Day Surgery Unit, patients who are unable to arrange overnight care are offered a carer to stay with them for the first postoperative night (at no cost to the patient). This means the patients and hospital continue to benefit from the established day surgery pathway. It is more cost effective for the trust (£100-£150 versus £300 estimated cost of an inpatient stay) and releases valuable inpatient beds for those more in need of this resource. Eligible patients are identified at the pre-operative assessment clinic and details given to a hospital discharge coordinator. This person then liaises with relevant care agencies and the patient to arrange overnight care. Between April 2014 and February 2017, 139 such referrals were made (Figure 1). 57 (41%) had a carer provided, of interest, 21 patients (15%) who initially had no care managed to find care from family and friends. 11 patients had their surgery cancelled for reasons other than post-operative care and 22 patients still needed admission for varying reasons (Table 4). Unfortunately, occasionally, the agencies do not have carer availability (9 patients in this period). Very few patients (3) declined the option of provided care, resulting in hospital admission. On routine post-operative telephone follow up, all the patients who were contacted were satisfied with their overall day surgery experience, including post-operative care (figure 2).
Having a system in place to provide patients with overnight care following day surgery can be a cost effective and beneficial alternative to admission to hospital. There is a reduction in inequality of care and more patients are able to benefit from day surgery. In addition, the use of an inpatient bed, a precious resource, may be avoided.
Figure 1: Numbers of patients referred for provision of a carer at Torbay Hospital Day Surgery Unit
(April 2014 – February 2017).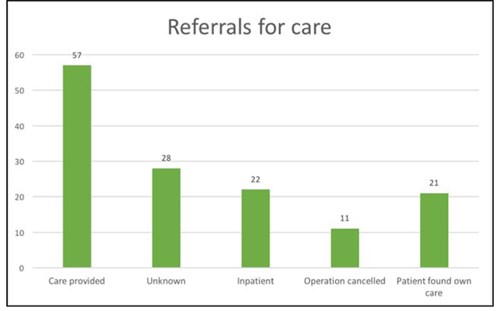
Figure 2: Overall satisfaction of day surgery experience for patients who have had carer provided overnight
at Torbay Day Surgery Unit.
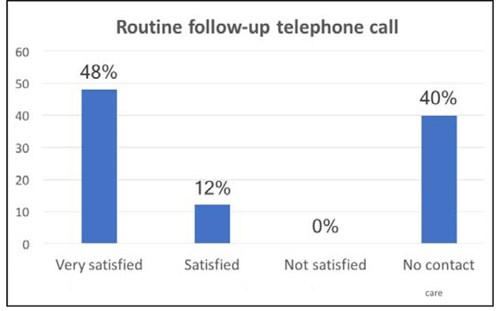
Table 4: Reason for inpatient admission despite referral for provision of a carer at Torbay Day Surgery Unit.
The Norfolk and Norwich Experience: The Self-Care Pathway
Like all hospitals the Norfolk and Norwich University Hospital has problems with lack of inpatient beds and it is important to ensure patients are only admitted overnight when absolutely necessary. A regular reason for admission after surgery suitable for same day discharge is patients who live alone and are unable to find someone to stay with them for 24 hours. To ensure effective use of inpatient beds and to enable day surgery to be an option for all patients it was decided to explore ways that patients who live alone could have their operation without an inpatient stay. After the survey (see above) and review of the literature it was decided that for some patients having certain procedures that it would be safe for them to go home without a carer.
A pathway was therefore developed that balanced the risks of surgery and patient’s wishes, to allow suitable patients to return home with no carer in place (Figure 3). Criteria for patients to meet self-care pathway includes:
- Safe surgery for home alone
- Patient would like to go home alone
- No comorbidities excluding patients from day case
- Need an escort home in private car
- Decision made in preoperative assessment clinic
Figure 3: Norfolk and Norwich University Hospitals NHS Foundation Trust ‘Self-Care Pathway’
following day surgery.
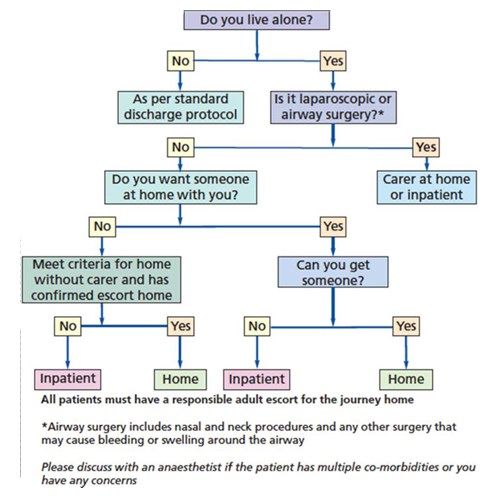
The criteria for patients to meet the self-care pathway are:
- Safe surgery for home alone
- Patient would like to go home alone
- No comorbidities excluding patients from day case
- Need an escort home in private car
- Decision made in preoperative assessment clinic
Added benefits, for the pathway, include no cost implications for the hospital and a reduction in admission rates. The planning for this is all done by the nurses in preoperative assessment clinic (POA). All patients are given information at this point about their procedure and the anaesthetic so patients can make informed decisions. Posters are also displayed in the POA waiting area so patients are aware of this process.
The pathway is in line with the guidance in the RCOA ‘Guidance of the provision of anaesthetic services [1]’: ‘Following procedures under general anaesthesia, a responsible adult should escort the patient home and provide support for the first 24 hours after surgery. A carer at home may not be essential if there has been good recovery after brief or non-invasive procedures and where any post-operative haemorrhage is likely to be obvious and controllable with simple pressure. Transport home should be by private car or taxi; public transport is not normally appropriate.’ In writing the pathway we took in to account patient’s wishes but also the safety of the procedures. Our surgical exclusions in the pathway are in line with GPAS guidelines. Our main concerns for postoperative complications were haemorrhage and airway compromise, these are not common causes for readmission but they could be catastrophic, therefore we excluded all airway surgery, surgery around the neck and laparoscopic surgery where direct pressure cannot be applied. Also, patients having eye surgery, if partially sighted in their other eye, are not considered to be able to go home on their own for obvious patient safety reasons. On the day of surgery, the responsible surgeon and anaesthetist are able to change the pathway to the inpatient pathway if required.
Patients who prefer to have a carer after surgery but are unable to arrange this will be offered an overnight bed but will be made aware that there may be a risk of cancellation on the day if the beds are not available. Also, as usual, patients are encouraged to find someone to stay with them if they do not fit the criteria for the self-care pathway. All surgeons, anaesthetists and nursing staff were informed of the pathway. We have a lead nurse to help with education and implementation in Day Procedure Unit. Recently we have adopted a ‘self-care pathway’ outcome on the computer system which links with the operating list. It is important to note that patients must still have an escort to take them home. An escort home provides important functions such as helping with information recall, providing observation on the way home and settling the patient in on arrival home. Since introduction the self-care pathway has been successfully implemented. A small survey after introduction showed all patients managed on the self-care pathway were satisfied and no problems have occurred with these patients.
Conclusion
It is clear that there is a wide variation in practice in this area of day surgery, both in terms of what the patients choose to do (despite instructions) and what different departments recommend. Concern regarding impairment of cognitive and psychomotor skills has often been cited as reasons for requiring care following day surgery. In addition, the legal implications of driving after anaesthesia cannot be underestimated as demonstrated in case reports of accidents and subsequent malpractice suits in patients who drove after day surgery [20]. However, it is imperative to make a distinction between the patient driving and the patient having overnight care - these two are clearly not the same and as such should not be grouped together. It remains imperative that patients are escorted home by a responsible adult and seen safely into their home so that someone knows they have had surgery and are home alone, if this is going to be the case.
Day surgery has continually evolved over many years and now encompasses a wide spectrum of procedures and patients. This means that a ‘one size fits all’ approach to certain aspects of the practice of day surgery may not be in the best interests of the patients or departments and hospital trusts. Articles and recommendations have often focussed on the day surgery population as a whole but it is clear that different patient groups are likely to have different requirements post-operatively. This is demonstrated in the survey by Barker et al. where the time it took for patients to feel safe varied depending on the extent of their surgical procedure and expected pain levels. It may therefore be more appropriate to identify different groups of patients depending on the procedures and their wishes. GPAS guidelines for day surgery state ‘A carer at home may not be essential if there has been good recovery after brief or non-invasive procedures and where any post-operative haemorrhage is likely to be obvious and controllable with simple pressure’. This encompasses a large number and variety of day case procedures. This is demonstrated well by the policy at Norfolk and Norwich, where carefully selected patients may be sent home, despite no carer being present overnight.
It should be noted that although we describe the literature on this subject, this is not a formal systematic review or analysis of the evidence and we accept this as a limitation of this article. Similarly, caution must be applied when applying results of international studies and surveys to the UK population and practice due to the clinical heterogeneity as well as differing healthcare structures (e.g. private vs. public funded). A UK based randomised controlled trial in this area may well be indicated.
While the literature is limited, there is no firm evidence of harm when no carer is present. Many patients presenting for day surgery will ‘by default’ have someone available for support at home in the form of a spouse, partner or family member. This support is often invaluable to the patient following their procedure. However, day surgery units should have dynamic policies in place and seek innovative solutions when faced with patients who do not have overnight care. This is reflected in the latest guidelines in the United Kingdom [1, 2].
Acknowledgements
This article is based on two presentations given at the 2017 BADS Annual Scientific Meeting in Southport.
References
- Noble T. A Model for Providing Day Surgery for Patients with No Overnight Care. Journal of One-Day Surgery. 2014. 24S. B1.
- Allan K, Morris R, Lipp A. Day Procedure Survey: Self Care Post Discharge at the Norfolk and Norwich University Hospital (NNUH). Journal of One-Day Surgery. 2015. 25S. A20.
- Royal College of Anaesthetists (RCOA). Guidelines for the Provision of Anaesthesia Services (GPAS). Guidelines on the provision of anaesthesia services for day surgery (2016). https://www.rcoa.ac.uk/system/files/GPAS-2016-06-DAYSURGERY.pdf
- Verma R, Alladi R, Jackson I, Johnston I, Kumar C, Page C, Smith I, Stocker M, Tickner C, Williams S and Young R. Day case and short stay surgery: 2, Anaesthesia 2011; 66: pages 417-434
- Discharge Process and Criteria. International Association for Ambulatory Surgery. http://www.iaas-med.com/index.php/iaas-recommendations/discharge-process-and-criteria Accessed 1 March 2017.
- Australian and New Zealand College of Anaesthetists (ANZCA). Guidelines for the Perioperative Care of Patients Selected for Day Stay Procedures (PS15). 2016. http://www.anzca.edu.au/documents/ps15-2010-recommendations-for-the-perioperative-ca.pdf
- Apfelbaum JL, Silverstein JH, Chung FF, Connis RT, Fillmore RB, Hunt SE, Nickinovich DG, Schreiner MS, Silverstein JH, Apfelbaum JL, Barlow JC, Chung FF, Connis RT, Fillmore RB, Hunt SE, Joas TA, Nickinovich DG, Schreiner MS; American Society of Anesthesiologists Task Force on Postanesthetic Care. Practice Guidelines for Postanesthetic care. An Updated Report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. Anesthesiology. 2013; 118: 291-307.
- Dobson G,Chong M, Chow L, Flexman A, Kurrek M, Laflamme C, Lagacée A, Stacey S, Thiessen B. Dobson G, Chong M, Chow L, et al. Guidelines to the Practice of Anesthesia – Revised edition 2017. Canadian Journal of Anesthesia. 2017. 64: 65-91.
- Fahy A, Watson BG and Marshall M. Postanaesthetic follow-up by questionnaire: A research tool. British Journal of Anaesthesia. 1969; 41: 439.
- Ogg TW. An assessment of postoperative outpatient cases. British Medical Journal. 1972; 4: 573-576.
- Correa R, Menezes RB, Wong J, Yogendran S, Jenkins K, Chung F. Compliance with postoperative instructions: a telephone survey of 750 day surgery patients. Anaesthesia. 2001; 56: 447-484.
- Cheng CJC, Smith I, Watson BJ. A multicentre telephone survey of compliance with postoperative instructions. Anaesthesia. 2002; 57(8): 805-11.
- Barker J, Holmes K, Montgomery J, Bennun I, Stocker M. How long is 24 hours? A survey of how long a carer stays with the patient post discharge. Journal of One-Day Surgery. 2014. 24(2): 57-60.
- Wessels F, Kerton M, Hopwood H. Evaluating the need for day surgery patients to have 24 hours of adult supervision postoperatively. Journal of One-Day Surgery. 2015. 24(4): 17-2.
- Friedman Z, Chung F, Wong DT. Ambulatory surgery adult patient selection criteria – survey of Canadian anesthesiologists. Canadian Journal of Anesthesia. 2004; 51(5): 437-44.
- Stomberg MW, Brattwall M, Jakobsson JG. Day surgery, variations in routines and practices a questionnaire survey. International Journal of Surgery. 2013; 11(2): 178-82.
- Segerdahl M, Warren-Stomberg M, Rawal N, Brattwall M, Jakobsson J. Clinical practice and routines for day surgery in Sweden: results from a nation-wide survey. Acta Anaesthesiologica Scandinavica. 2008; 52: 117-124.
- Ip HYV, Chung F. Escort accompanying discharge after ambulatory surgery: a necessity or a luxury? Current Opinion in Anesthesiology. 2009. 22: 748-54.
- Abdullah HR, Chung F. Postoperative issues: discharge criteria. Anesthesiology Clinics. 2014; 32: 487-493
- Chung F, Assmann N. Car accidents after ambulatory surgery in patients without an escort. Anesthesia and Analgesia. 2008; 106(3): 817-820.
- Chung F,Imasogie N, Ho J, Ning X, Prabhu A, Curti B. Frequency and implications of ambulatory surgery without a patient escort. Canadian Journal of Anesthesia. 2005; 52(10): 1022-1026.
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6186/281-retief.pdf