Experience of introducing Urolift procedure to the Day Procedure Unit at Norfolk and Norwich University Hospital « Contents
Mark Rochester Consultant Urological Surgeon and Service Director
Anna Lipp Consultant Anaesthetist and Clinical Lead Day Surgery
Urology, Norfolk and Norwich University Hospital, Colney Lane, Norwich UK
Aims & Objectives
Aims
Introduce an ambulatory surgical treatment option for men with lower urinary tract symptoms (LUTS) from benign prostate hypertrophy (BPH), guided by NICE recommendations1.
Objectives
- Increase theatre capacity and reduce pressure on inpatient beds, thereby reducing pressure on waiting times
- Offer greater treatment choice to men requiring surgery for LUTS from BPH
- Reduce complications from existing surgical intervention for LUTS from BPH
Context
NNUH is a large teaching hospital with a busy Urology department. It has a local catchment area of over 800,000 patients and a large elderly population. It performs 350– 400 bladder outlet obstruction procedures each year, and has significant and increasing pressure on waiting times for urological procedures, especially for cancer, where volume is high.
There is an urgent need to free up theatre capacity and inpatient beds. The current standard of surgical care offered to men with LUTS from BPH at NNUH is either transurethral resection of the prostate (TURP) or holmium laser enucleation of the (HoLEP). NNUH performs around 150 TURP procedures each year, with an average length of stay of 3 days. It performs a similar number of HoLEP procedures each year, and patients are normally discharged the same day with a catheter.
TURP and HoLEP are both performed under a general or spinal anaesthetic and take up an average of 56 and 72 minutes of theatre time (patient turnaround time) respectively. While both TURP and HoLEP are effective at relieving the symptoms of LUTS, they can be associated with significant post-operative complications, including bleeding, infection and incontinence, which can prolong length of stay and delay recovery, and can also require further intervention, Permanent side effects can include sexual dysfunction and urinary incontinence.
TURP and HoLEP also necessitate the use of a catheter after the procedure (often for several days after a TURP) increasing the risk of urinary tract infection UroLift presented an opportunity to employ an ambulatory and minimally invasive procedure to treat a large proportion of patients who require surgery for LUTS from BPH. In addition to reducing the length of stay and theatre time, UroLift is also associated with a significantly reduced risk of permanent side effects and serious complications, compared with TURP and HoLEP.
Urolift can be performed under local anaesthesia(LA) which both avoids risks of general anaesthesia and has significantly reduced costs. Local anaesthesia can be administered by the surgeon, avoiding requirement for an anaesthetist and the costs of drugs and equipment required for a general anaesthetic. If a suitably equipped procedure room is available, procedures under LA could potentially be performed there freeing up operating theatres with GA capacity for other procedures.
NICE suggests that UroLift will help improve productivity through reduced post-discharge follow-up both in primary care and outpatient settings. UroLift also does not require the patient to be catheterised, therefore reducing the risk of catheterisation-associated UTI. As a short, ambulatory procedure, performed under a local anaesthetic, UroLift provided the opportunity for more efficient use of the Day Procedure Unit at NNUH.
Methods
In January 2015, a business plan was developed and taken through usual Trust business planning process. The focus of the business case was reduction in inpatient bed days, theatre hours, waiting times and cost savings.
A particular point of interest was savings that could be made from the avoidance of fines for waiting time breaches. UroLift was approved by the New Procedures Committee in August 2015, and by the Divisional Board in October 2015, following funding negotiation with commissioners.
NNUH offers a ‘one-stop’ urology clinic, which provides comprehensive assessment of patients with urological symptoms. At this clinic, a history is taken, the patient is examined and prostate symptoms are assessed using the International Prostate Symptom Score (IPSS) questionnaire. Flow rate and residual volume are measured and patients with LUTS undergo a flexible cystoscopy to determine suitability for different surgical options.
Once a full assessment is complete, patients are counselled on the different treatment options and patient information sheets are provided. Patients leave the clinic with a management plan, which may include surgery as an option.
The first patients to be treated with UroLift were identified through a series of four dedicated one-stop LUTS clinics, which were run over November and December 2015. Clinical training for UroLift and case observation took place and in January 2016 the first UroLift procedures were performed.
Patients requiring surgery for LUTS are offered a choice of surgical options, which now include UroLift. The majority of patients requiring surgical intervention for their BPH symptoms would be clinically eligible for UroLift, however some patients would not be considered suitable due to the size of their prostate (over 100ml) or the presence of an obstructive median lobe.
UroLift procedures are performed in the Day Procedure Unit. Initially these were performed under a general anaesthetic, but as confidence of the surgeon in the procedure grew, local anaesthetic (instillagel) was offered alone or combined with propofol sedation and this is now routine. The topical local anaesthetic is chilled in the refrigerator to 4ºC and one 11ml syringe delivered after consent has been taken in the preoperative bay, 10 minutes before the procedure. Patients are encouraged to hold the tip of the penis to prevent the gel from leaving the urethra until they arrive in theatre. Two to four UroLift implants are used, depending on the size of the prostate. No catheter is used and patients are discharged as soon as they have voided – normally after a couple of hours. No routine discharge medication apart from analgesia is prescribed. Patients are followed up with a symptom score measure and flow rate at 3 months to enable prospective audit of the service.
Results and evaluation
Over 90 patients have been treated with UroLift. In the majority of these patients, local anaesthetic was used and is now routine. The results of a recent audit of the first 12 months of the service are shown in the table below.
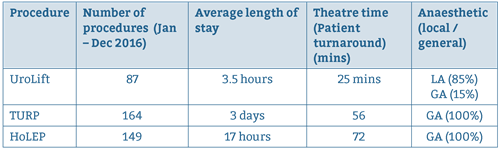
Procedure
In this cohort, the average number of implants required per patient was 2.8. However, during this early part of our learning curve, we tended to recruit patients with smaller prostates, who required fewer implants.
We currently offer UroLift to patients with prostates up to 100ml and requirement overall is up to 4 implants per patient. Complications are very rarely seen and are very minor compared with the number and severity of complications routinely reported with TURP. At the 3 month follow-up, patients had significant improvements in the key clinical parameters, including IPSS, quality of life scores, urinary flow rate (Qmax) and post-void residual volume (RV).
Encouragingly, improvements in the average IPSS mirrored that observed at 3 months in clinical trials with UroLift with a reduction in mean IPSS score from 21.6 to 12.5 and mean bother score from 4.4 to 2.3. The team concluded that UroLift is an effective treatment option for men requiring surgery for LUTS from BPH. The UroLift procedure is straightforward and easy to learn, without requirement for additional resources apart from the UroLift implants themselves. It can be easily performed under a local anesthetic, enabling quick turnaround in theatre.
Procedure time (patient turnaround time) is 25 mins, and 7-8 cases can be done in an afternoon list. Recovery is quick and the side effects and complex complications commonly associated with other surgical interventions are avoided. Unlike other surgical options for LUTS, UroLift is a true ambulatory procedure, where patients are discharged without a catheter after only a few hours and require minimal follow-up.
Analysis of the cases performed to date concluded that UroLift is a cost effective treatment, compared with other surgical options, and we expect it to provide significant efficiency and productivity savings by reducing inpatient bed stay, theatre time and follow-up. For the future role of UroLift, the team are considering moving the procedure out of the day unit into an ambulatory setting, which would relieve pressure on the Day Procedure Unit. Also the procedure may lend itself to a ‘see and treat’ pathway whereby patients are assessed and treated in the same day, which would provide further efficiency savings.
Key learning points
- Commence funding discussions with commissioners as early as possible and involve department Business Manager for support and in development of business case.
- The business case should take into consideration that most men with lower urinary tract symptoms (not in retention) and obstructing flow rate are candidates for UroLift. These men will have a prostate size of <100ml and will have no significant median lobe. The average number of implants required is less than 4, however, many patients require 2 or 3. Occasionally, with a large prostate, 5 or 6 implants are required
- Training should follow the manufacturer’s rigorous format to ensure best clinical outcomes.
- Surgeons may want to perform initial cases under a general anaesthetic until they are confident with the procedure. After this, the procedure can easily be performed under a local anaesthetic, or light sedation if required.
- Data collection and audit is very important to demonstrate patient outcomes and benefits, as well as efficacy savings.
- Assessment of patients is best carried out in a one-stop clinic, with access to cystoscopy, in order to limit patient visits.
Reference
1 https://www.nice.org.uk/guidance/conditions-and-diseases/urological-conditions/lower-urinary-tract-symptoms