Day Case Holmium Laser Enucleation of the Prostate for all ages and all prostate sizes « Contents
Omar Al Kadhi, Kate Manley, Madhavi Natarajan, Anna Lipp, Rachel Morris & Mark Rochester
Norfolk and Norwich University Hospital NHS Foundation Trust, Department of Anaesthesia
Keywords: HoLEP, day case pathway, laser, prostatectomy.
Introduction:
Day case Holmium laser enucleation of the prostate (HoLEP) has been described in the literature as a safe and effective treatment for small volume prostates. Day case surgery for male lower urinary tract symptoms (LUTS) confers significant financial benefits for hospital trusts due to enhanced tariffs. This study investigates the feasibility of performing day case HoLEP for any size prostate and any age of patient.
Methods:
Data was analysed for all patients listed as a day case HoLEP at a single centre over the first 26 months of a new day case service. Intraoperative details, complications, reasons for failed discharges and 6 month International Prostate Symptom Scores (IPSS) were recorded.
Comparison of complications and outcomes are compared with those in the published literature, and reasons for increased length of stay were investigated. Three year follow-up data was collected to determine later complications such as stricture formation and the need for additional surgery for bladder outflow obstruction.
Results:
267 HoLEPs were performed, 76.7% were intended as day case procedures. Of intended day case patients, 82.9% (n=170) were discharged the same day. Complications were recorded in the immediate postoperative period in 9.41%, readmission rate was 2.94% and later complications in 4.11%. Median postoperative IPSS and QoL scores were 2 and 0 respectively.
Conclusion:
Day case HoLEP is a feasible and safe treatment regardless of age or prostate size. Complication and readmission rates compare favourably with those in the published literature. As day case HoLEP attract an enhanced tariff in addition to the benefits of a reduced length of hospital stay, developing a day case service with a dedicated patient pathway is appealing.

Introduction
Lower urinary tract symptoms (LUTS) are estimated to affect more than 40% of males over the age of 50, and a significant proportion are due to the development of benign prostatic hyperplasia (BPH)1. The gold standard management for LUTS associated with BPH has traditionally been transurethral resection of prostate (TURP). This procedure is commonly performed by UK urologists (more than 42,000 per year in England and Wales) and involves resection of prostatic tissue usually using bipolar diathermy via the transurethral route. There is a significant body of literature supporting its use for improving male LUTS from objective measures such as flow rate and also through patient-reported symptom scores such as the IPSS. TURP, although used widely, has associated risks including TUR syndrome and excessive bleeding. In addition, there is a requirement for catheterisation and bladder irrigation post-operatively and increased length of stay (LOS) in the short term, and urethral or bladder neck stricture formation and retrograde ejaculation in the longer term2–4.
Since the 1980s, advances in technology have brought numerous alternatives including photoselective vaporisation of prostate (PVP), interstitial laser coagulation and Holmium Laser enucleation of prostate (HoLEP) to the fore. HoLEP was first described by Gilling et al5 and has been increasingly performed and assessed rigorously in comparison with other techniques for removal of prostate tissue. HoLEP is a minimally invasive technique involving exposure of prostatic capsule through incision and vaporisation of peri-urethral prostate using a Holmium laser through a resectoscope with continuous saline flow, followed by separation of prostatic tissue from the capsule. This tissue is subsequently broken down using an intravesical morcellator in order to extract the tissue from the bladder6. As the procedure does not use electrical current, the irrigant used during HoLEP is non-ionic thereby reducing the risk of extravasation and serum dilution resulting in TUR syndrome which is occasionally seen following prolonged TURP.
HoLEP is a relatively bloodless procedure7 and can be used to treat a broad spectrum of prostate sizes as demonstrated in a study by Kuo8 looking at retrieval tissue of very large prostates of >75g using HoLEP. Although cost analysis place each HoLEP procedure as being more expensive than TURP, cost savings made through reduced rate of blood transfusion, reduced LOS and shorter post-operative irrigation make the two procedures comparable in terms of cost efficiency7. It is increasingly popular and has been proposed as the future ‘gold standard’ as it has similar therapeutic efficacy to TURP, is more versatile and has a favourable side effect profile3,9. In addition to being suitable for any size prostate, it has also been demonstrated that advanced age should not be an issue for performing HoLEP, with a study suggesting that the procedure is safe and effective in patients over 80 years of age10.
Day case HoLEP has previously been described in the literature as a safe and efficacious management of bladder outflow obstruction for small volume prostates of <60ml. To date, several studies have been published examining the safety and success of day case HoLEP in small patient cohorts (n=30–50)11–13. We present the outcomes of a new day case service to demonstrate the efficacy of performing day case HoLEP for any size prostate over a larger patient group (n=205).
Day case urological surgery in the elderly population has gained interest over the years, elderly and medically unfit patients can be treated safely as day cases provided they are cared for in a well organised and equipped day unit. Elderly patients have reported favourable experiences with urological day case surgery14. The current study examines the suitability of day case HoLEP for patients of any age or comorbidity, with appropriate pre-operative preparation and selection.
In the UK, day case surgery attracts an enhanced hospital payment tariff – this incentive was initiated for HoLEP and TURP by the Department of Health (DoH) payment by results (PbR) office in light of increasing demand for shorter inpatient stays due to pressure on resources. In 2011, initial day case target rates for HoLEP were set at 30%. More recently, the 2014/2015 National Tariff system has suggested a target of 60% for resection of prostate by laser15. In light of the additional cost-benefit of day case surgery, this paper also briefly examines the financial implications of performing day case HoLEP when compared to TURP, the current gold-standard.
Methods
A new day case pathway for patients undergoing HoLEP was evaluated at a single centre where over 300 procedures for BPH are performed annually. The day case pathway was commenced in September 2012; all patients regardless of age or prostate volume were listed as day case procedures unless deemed unsuitable following review by a consultant anaesthetist in a preoperative clinic. Patients were excluded on the basis of anaesthetic risk (e.g. severe ischaemic heart disease or valvular disease) or if discharge on the day of surgery was deemed to be unsafe for social reasons. All surgical procedures were performed by one of three consultant urologists experienced in performing HoLEP. Patients were discharged on the day of surgery and underwent a trial without catheter (TWOC) on day 1 postoperatively in the community, facilitated by the Community District Nursing Team. Data was gathered for all intended day case HoLEPs performed over a 26 month period including patient demographics; intraoperative details – type of anaesthesia used, time taken for resection, specimen weight and immediate complications. Reasons for failed day cases and readmission rates were also collected. Factors influencing successful daycases and failed daycases were compared, statistical analysis was performed using Fisher’s exact test and unpaired t-testing. Finally, longer-term outcomes were recorded such as 6-month IPSS scores, and 3 year follow-up to identify complications such as stricture formation, incontinence and the requirement for repeat surgery. A cost-effectiveness analysis of the procedure compared to TURP was performed to evaluate the financial benefits of performing day case HoLEP.
Results
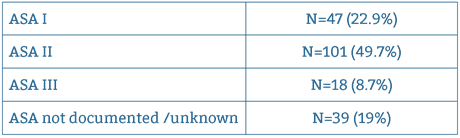
Over the 26 month period, 267 HoLEPs were performed, 76.7% (n=205) were intended as day cases. Median age was 70 years (range 44 – 89 years). American Society of Anaesthesiologists Physical Status Classification distribution is illustrated in Table 1.
27 cases (13.1%) were performed in main theatres and 86.9% (n=179) were performed in the Day Procedure Unit (DPU) theatres. The majority of cases were done under General Anaesthesia (92.23%, n=190) and the remaining 16 cases (7.77%) were done under Spinal Anaesthesia. Mean total intraoperative time was 55.91 mins with a mean enucleation time of 40.34 mins and a mean morcellation time of 15.57 mins. Mean weight of resected prostatic tissue was 32.8g (range 1–190g). Seventeen patients (8.25%) had resected weights of more than 70g.
170 patients were successfully discharged on the day of surgery (82.9%). There were 35 failed day cases – more than a third of these stayed as an inpatient for more than 1 day (range 1–4 days, mean LOS 1.5 days).
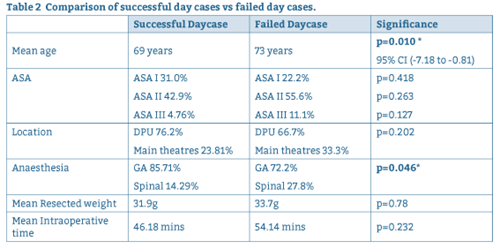
Reasons for failure of discharge on the day of surgery are summarised in Figure 1. Intraoperative factors and patient factors are compared for successful and failed day case procedures in Table 2.
Figure 1: Factors influencing failed discharge on day of surgery.
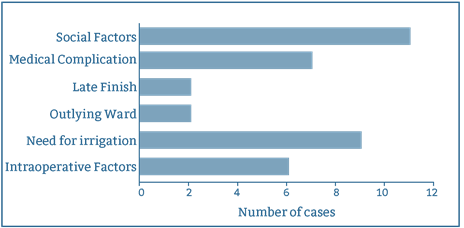
Table 2: Comparison of successful day cases vs failed day cases.
For successful day case procedures, immediate postoperative complication rate was 9.41%, (n=16) and readmission rate was 2.94% (n=5). One patient required a return to theatre for a washout / evacuation of clot from bladder for intractable bleeding. Immediate complications and reasons for readmission are summarised in Tables 3 and 4 respectively:
| Complications (immediate/early) |
| Prostate capsular perforation 2.94%, n = 5) |
| Retained fragment (1.17%, n = 2) |
| Failed TWOC (2.94%, n = 5) |
| Haematuria requiring transfusion (0.58%, n = 1) |
| Sepsis (1.17%, n = 2) |
| NSTEMI postop (0.58%, n = 1_ |
| 9.41% (n = 16) |
Table 3: Summary of Immediate /Early Postoperative Complications.
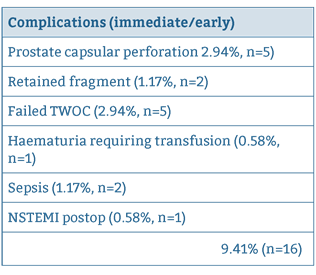
Table 4: Summary of postoperative readmissions to hospital.
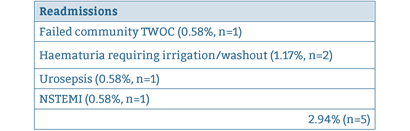
Later complications such as requirement for repeat surgery and stricture formation rate are summarised in Table 5. For late complications, follow up was carried out at a median of 3.2 years (range 2.18 – 4.4 years).
Table 5: Summary of late complications.
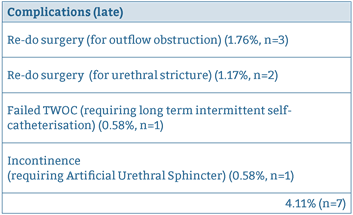
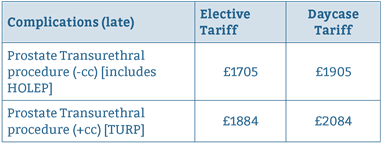
Table 6: Tariffs for HoLEP sand TURP.
Telephone follow up was conducted at 6 months and IPSS scores were collected. Of all patients contacted, a 69.7% response rate was recorded (n=143). Of the 143 patients contacted, median IPSS score was 2 "Mildly symptomatic" (range 0 – 25) and median bother / quality of life score was 0 (quality of life is assigned a score of 0 – 6, the higher score denoting greater dissatisfaction with symptoms).
Tariffs for HoLEP and TURP are summarised in Table 615. The average length of stay at our institution for TURP is 2.5 days; with the cost of an inpatient stay approximately £228 per day. Over 205 cases, it is calculated that TURP would generate a total of income £1135 per case when taking into account costs of hospital stay, compared to an income £1905 per case for day case HoLEP. This is a saving of £770 per case, which over 205 cases translates to £157,850.
Discussion
There is a significant body of evidence to suggest the HoLEP is at least equivalent, if not superior to TURP, the current gold standard. HoLEP has out-performed TURP in meta-analyses of weighted mean difference in Qmax (peak urinary flow rate) compared pre and post-operatively, and was significantly better than TURP in time spent with catheter in-situ, LOS and blood loss16–17. These findings were confirmed in a systematic review which reported that improvements to QMax and IPSS following HoLEP were significantly superior compared to TURP7. The disadvantages described with the use of HoLEP are that it requires specialist training and, hence, is not as accessible as TURP. It also requires a longer operative time, although tends to be used for larger prostates and hence efficiency of operative time related to prostatic tissue removed is comparable6,18. Despite this, HoLEP is desirable as it offers no recorded incidence of TUR syndrome5.
The results of this study suggest that day case HoLEP is indeed safe and efficacious for any age of patient and any size of prostate, provided appropriate pre-operative assessment and preparation of suitable patients is conducted. Our results compare favourably to those reported in the literature for complications, readmission rates and day case rates11–13. Outcomes such as symptom scores at 6 month telephone follow up and longer term complication rates are equivalent to TURP, in addition to a comparable mean intraoperative time2.
The achieved day case rate of 83% is more than satisfactory in light of the Department of Health (DoH) 2014/2015 National Tariff system suggested target of 60%. Performing HoLEP as a day case procedure confers significant financial benefits for an institution and enables main theatres to be used for other surgical cases which may be more in need of such a facility. Whilst the initial outlay for the laser equipment itself might be costly, the vast majority of urological units in the UK will already possess a laser suitable for HoLEP. nterest is growing in 50W HoLEP surgery given its lower capital cost 19. Whilst intraoperative time is slightly longer for HoLEP compared to TURP7, the financial cost of this is more than outweighed by the increased tariff and reduced bed occupancy afforded by day case surgery. It should also be noted that green light laser and bipolar TURP can also be done as day case procedures, however repeat surgery rates are higher for those surgeries when compared to HoLEP9.
The British Association of Day Surgery (BADS) Dataset of Procedures (Urology section) illustrates actual day case rates achieved in hospitals in England for 201520. The top 5% of hospitals achieved rate of 60%, however the top 25% achieved only 26% day case rates. The high day case rates from the current institution are largely attributed to the defined day case pathway, which ensures that appropriate patients are identified and that cases are, where possible, performed in a designated Day Procedure Unit.
Factors associated with failed day cases appear to include longer operative times, larger prostate size, increasing ASA grade, and location of procedure (in Main Theatres rather than the Day Procedure Unit). Mean age and proportion of spinal anaesthesia vs general anaesthesia were found to be statistically significantly higher in failed day cases when compared to successful ones. Factors which delay discharge such as intraoperative or anaesthetic complications are often unavoidable, however a designated day case pathway can be employed to optimise other influences, such as the location of surgery and post-operative recovery and the selection of suitable patients who have adequate support at home following discharge. The main reason for failed day cases appears to be due to lack of social support following discharge. At our institution, for a short period at the initiation of the day case pathway, pre-assessment appointments were conducted by two separate teams of nurses. Patients who were assessed by inpatient pre-assessment teams (as opposed to outpatient pre-assessment clinics) may not have adequately checked whether social circumstances were appropriate for same-day discharge – this reaffirms the importance of having a clearly defined pathway of care for a given procedure.
Effective team-working between surgeons, anaesthetists and the Day Procedure Unit nursing team is vital to ensuring the smooth running of the day case pathway, to enable appropriate pre-operative assessment and counselling of patients prior to their surgery, and to facilitate timely discharge post-operatively. We suggest that HOLEP should be assumed to be a day case pathway unless reasons are identified at surgical or nurse pre-assessment that indicate this is not likely to be possible. Achieving high day case rates for patients with any age and any size prostate is both feasible and safe and offers significant financial benefits for hospital trusts.
References
- Trueman P, Hood SC, Nayak USL, Mrazek MF. Prevalence of lower urinary tract symptoms and self-reported diagnosed "benign prostatic hyperplasia", and their effect on quality of life in a community-based survey of men in the UK. BJU Int. 1999;83(4):410–5.
- Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of Transurethral Resection of the Prostate (TURP)-Incidence, Management, and Prevention. Eur Urol. 2006;50(5):969–80.
- Razzak M. BPH: HoLEP—a steep learning curve but better for patients. Nat Rev Urol [Internet]. Nature Publishing Group; 2012;10(2):66–66. Available from: http://www.nature.com/doifinder/10.1038/nrurol.2012.236
- Chen YB, Chen Q, Wang Z, Peng YB, Ma LM, Zheng DC, et al. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year follow up. Journal of Urology. 2013: 217–22.
- Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology 1996;47(1):48–51.
- Bostanci Y, Kazzazi A, Djavan B. Laser Prostatectomy : Holmium Laser Enucleation and Photoselective Laser. 2013;15(1):1–10.
- Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al. Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement. Health Technol Assess. 2008;12(35).
- Lai M-C, Kuo Y-C, Kuo H-C. Intravesical hyaluronic acid for interstitial cystitis/painful bladder syndrome: a comparative randomized assessment of different regimens. Int J Urol [Internet]. 2013 Feb [cited 2014 Jul 21];20(2):203–7.
- Michalak J, Tzou D FJ. HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century. Am J Clin Exp Urol. 2015;3(1):36–42.
- Clyne M. BPH: Age not an issue for HoLEP. Nat Rev Urol. 2013 May;10(5):249. 1. Epub 2013 Apr 9.
- Larner TRG, Agarwal D, Costello AJ. Day-case holmium laser enucleation of the prostate for gland volumes of <60ml: early experience. BJUI. 91(1), (61–64).
- Cynk M, Georgiadis G, Moore E, Appleby J, Griffiths R, Hale J. Day-case holmium laser enucleation of the prostate. Journal of Clinical Urology 2015;8(4):268–273.
- Gabbay G et al. [Holmium laser enucleation of the prostate as a day case surgery: prospective evaluation of the first 30 patients]. Prog Urol. 2015;25(1):34–9.
- Briggs TP, Anson KM, Jones A, Coker BJ, Miller RA. Urological day case surgery in elderly and medically unfit patients using sedoanalgesia: what are the limits? Br J Urol. 1995 Jun;75(6):708–11.
- 2014/2015 National Tariff Payment System, Department of Health Gateway Reference 00883, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/300547/2014-15_National_Tariff_Payment_System_-Revised_26_Feb_14.pdf
- Aho TF. Holmium laser enucleation of the prostate: a paradigm shift in benign prostatic hyperplasia surgery. Ther Adv Urol 2013; 5(5):245–253.
- Hoffman RM, MacDonald R, Wilt TJ. Laser prostatectomy for benign prostatic obstruction. Cochrane Database Syst Rev. 2004;(1):CD001987
- Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007;94(10):1201–8.
- Khan F, Saleemi MA, Taneja S, Alam A, Al-Sheikh M, Nunney I, Aho T An Emerging Holmium laser enucleation of the prostate reality: 50-watt holium laser enucleation of the prostate surgery outcomes from a single unit. UK Journal of Urology. Apr 2016; (195)4s (570) (abstract only).
- BADS Directory of Procedures, National Dataset (Calendar Year 2015), British Association of Day Surgery, 2015.
Cite this article as https://daysurgeryuk.net/en/resources/journal-of-one-day-surgery/?u=/2017-journal/jods-272-2017/day-case-holmium-laser-enucleation-of-the-prostate-for-all-ages-and-all-prostate-sizes
Download this article as PDF here: https://appconnect.daysurgeryuk.net/media/6144/272-khadi.pdf